Abstract
Background
Morbidly obese patients are at increased risk to develop venous thromboembolism (VTE), especially after bariatric surgery. Adequate postoperative thrombosis prophylaxis is of utmost importance. It is assumed that morbidly obese patients need higher doses of low molecular weight heparin (LMWH) compared to normal-weight patients; however, current guidelines based on relative efficacy in obese populations are lacking.
Objectives
First, we will evaluate the relationship between body weight descriptors and anti-Xa activity prospectively. Second, we will determine the dose-linearity of LMWH in morbidly obese patients.
Setting
This study was performed in a general hospital specialized in bariatric surgery.
Methods
Patients were scheduled for a Roux-en-Y gastric bypass with a total bodyweight (TBW) of ≥ 140 kg. Patients (n = 50, 64% female) received a daily postoperative dose of 5700 IU of nadroparin for 4 weeks. Anti-Xa activity was determined 4 h after the last nadroparin administration. To determine the dose linearity, anti-Xa was determined following a preoperative dose of 2850 IU nadroparin in another 50 patients (52%).
Results
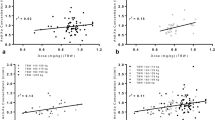
TBW of the complete group was 148.5 ± 12.6 kg. Mean anti-Xa activity following 5700 IU nadroparin was 0.19 ± 0.07 IU/mL. Of all patients, 32% had anti-Xa levels below the prophylactic range. Anti-Xa activity inversely correlated with TBW (correlation coefficient − 0.410) and lean body weight (LBW; correlation coefficient − 0.447); 67% of patients with a LBW ≥ 80 kg had insufficient anti-Xa activity concentrations. No VTE events occurred.
Conclusions
In morbidly obese patients, a postoperative dose of 5700 IU of nadroparin resulted in subprophylactic exposure in a significant proportion of patients. Especially in patients with LBW ≥ 80 kg, a higher dose may potentially be required to reach adequate prophylactic anti-Xa levels.


Similar content being viewed by others
References
Afshin A et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. https://doi.org/10.1056/NEJMoa1614362.
Frühbeck G. Bariatric and metabolic surgery: a shift in eligibility and success criteria. Nat Rev Endocrinol. 2015;11(8):465–77. https://doi.org/10.1038/nrendo.2015.84.
Freeman AL, Pendleton RC, Rondina MT. Prevention of venous thromboembolism in obesity. Expert Rev Cardiovasc Ther. 2010;8(12):1711–21. https://doi.org/10.1586/erc.10.160.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA : J Am Med Assoc. 2004;292(14):1724–37. https://doi.org/10.1001/jama.292.14.1724.
Quebbemann B, Akhondzadeh M, Dallal R. Continuous intravenous heparin infusion prevents peri-operative thromboembolic events in bariatric surgery patients. Obes Surg. 2005;15(9):1221–4. https://doi.org/10.1381/096089205774512528.
Scholten DJ, Hoedema RM, Scholten SE. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg. 2002;12(1):19–24. https://doi.org/10.1381/096089202321144522.
Escalante-Tattersfield T, Tucker O, Fajnwaks P, et al. Incidence of deep vein thrombosis in morbidly obese patients undergoing laparoscopic Roux-en-Y gastric bypass. Surger Obes Related Dis : Off J Am Soc Bariatric Surger. 2008;4:126–30.
Smith MD, Patterson E, Wahed AS, et al. Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Obes Surg. 2011;21(11):1687–92. https://doi.org/10.1007/s11695-011-0497-8.
Becattini C, Agnelli G, Manina G, et al. Venous thromboembolism after laparoscopic bariatric surgery for morbid obesity: clinical burden and prevention. Surger Obes Relat Dis : Off J Am Soc Bariatric Surger. 2012;8:108–15.
Birkmeyer NJ, Finks JF, Carlin AM, et al. Comparative effectiveness of unfractionated and low-molecular-weight heparin for prevention of venous thromboembolism following bariatric surgery. Arch Surg. 2012;147(11):994–8. https://doi.org/10.1001/archsurg.2012.2298.
Finks JF, English WJ, Carlin AM, et al. Predicting risk for venous thromboembolism with bariatric surgery: results from the Michigan Bariatric Surgery Collaborative. Ann Surg. 2012;255(6):1100–4. https://doi.org/10.1097/SLA.0b013e31825659d4.
Stroh C, Birk D, Flade-Kuthe R, et al. Evidence of thromboembolism prophylaxis in bariatric surgery-results of a quality assurance trial in bariatric surgery in Germany from 2005 to 2007 and review of the literature. Obes Surg. 2009;19(7):928–36. https://doi.org/10.1007/s11695-009-9838-2.
Melinek J, Livingston E, Cortina G, et al. Autopsy findings following gastric bypass surgery for morbid obesity. Arch Pathol Lab Med. 2002;126(9):1091–5. https://doi.org/10.1043/0003-9985(2002)126<1091:AFFGBS>2.0.CO;2.
Overby DW, Kohn GP, Cahan MA, et al. Prevalence of thrombophilias in patients presenting for bariatric surgery. Obes Surg. 2009;19(9):1278–85. https://doi.org/10.1007/s11695-009-9906-7.
De Luca M, Angrisani L, Himpens J, et al. Indications for surgery for obesity and weight-related diseases: position statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg. 2016;26(8):1659–96. https://doi.org/10.1007/s11695-016-2271-4.
Wei MY, Ward SM. The anti-factor Xa range for low molecular weight heparin thromboprophylaxis. Hematol Rep. 2015 Nov 23;7(4):5844. https://doi.org/10.4081/hr.2015.6027.
Nutescu EA, Spinler SA, Wittkowsky A, et al. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43(6):1064–83. https://doi.org/10.1345/aph.1L194.
Kalfarentzos F, Stavropoulou F, Yarmenitis S, et al. Prophylaxis of venous thromboembolism using two different doses of low-molecular-weight heparin (nadroparin) in bariatric surgery: a prospective randomized trial. Obes Surg. 2001;11(6):670–6. https://doi.org/10.1381/09608920160558588.
Celik F, Huitema AD, Hooijberg JH, et al. Fixed-dose enoxaparin after bariatric surgery: the influence of body weight on peak anti-Xa levels. Obes Surg. 2015;25(4):628–34. https://doi.org/10.1007/s11695-014-1435-3.
Mushtaq A, Vaughns JD, Ziesenitz VC, et al. Use of enoxaparin in obese adolescents during bariatric surgery—a pilot study. Obes Surg. 2015;25(10):1869–74. https://doi.org/10.1007/s11695-015-1630-x.
Diepstraten J, Hackeng CM, van Kralingen S, et al. Anti-Xa levels 4 h after subcutaneous administration of 5,700 IU nadroparin strongly correlate with lean body weight in morbidly obese patients. Obes Surg. 2012;22:79122.
Janmahasatian S, Duffull SB, Ash S, et al. Quantification of lean bodyweight. Clin Pharmacokinet. 2005;44(10):1051–65. https://doi.org/10.2165/00003088-200544100-00004.
Heizmann M, Baerlocher GM, Steinmann F, et al. Anti-Xa activity in obese patients after double standard dose of nadroparin for prophylaxis. Thromb Res. 2002;106(4-5):179–81. https://doi.org/10.1016/S0049-3848(02)00188-3.
Barras MA, Duffull SB, Atherton JJ, et al. Individualized compared with conventional dosing of enoxaparin. Clin Pharmacol Ther. 2008;83(6):882–8. https://doi.org/10.1038/sj.clpt.6100399.
Mahe I, Drouet L, Chassany O, et al. Low molecular weight heparin for the prevention of deep venous thrombosis: a suitable monitoring in elderly patients? Pathophysiol Haemost Thromb. 2002;32(3):134–6. https://doi.org/10.1159/000065216.
Samama MM, Gerotziafas GT. Comparative pharmacokinetics of LMWHs. Semin Thromb Hemost. 2000;26:31–8.
Diepstraten J, Janssen EJ, Hackeng CM, et al. Population pharmacodynamic model for low molecular weight heparin nadroparin in morbidly obese and non-obese patients using anti-Xa levels as endpoint. Eur J Clin Pharmacol. 2015;71(1):25–34. https://doi.org/10.1007/s00228-014-1760-4.
Gómez-Ambrosi J, Silva C, Galofré JC, et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes. 2012;36(2):286–94. https://doi.org/10.1038/ijo.2011.100.
Gómez-Ambrosi J et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care. 2012;35(2):383–8. https://doi.org/10.2337/dc11-1334.
Gómez-Ambrosi J, Andrada P, Valentí V, et al. Dissociation of body mass index, excess weight loss and body fat percentage trajectories after 3 years of gastric bypass: relationship with metabolic outcomes. Int J Obes. 2017;41(9):1379–87. https://doi.org/10.1038/ijo.2017.134.
Abou-Nukta F, Alkhoury F, Arroyo K, et al. Clinical pulmonary embolus after gastric bypass surgery. Surger Ob Relat Dis : Off J Am Soc Bariatric Surger. 2006;2(1):24–8; discussion 9. https://doi.org/10.1016/j.soard.2005.09.016.
Cotter SA, Cantrell W, Fisher B, et al. Efficacy of venous thromboembolism prophylaxis in morbidly obese patients undergoing gastric bypass surgery. Obes Surg. 2005;15(9):1316–20. https://doi.org/10.1381/096089205774512690.
Winegar DA, Sherif B, Pate V, et al. Venous thromboembolism after bariatric surgery performed by Bariatric Surgery Center of Excellence Participants: analysis of the Bariatric Outcomes Longitudinal Database. Surger Obes Relat Dis : Off J Am Soc Bariatric Surger. 2011;7:181–8.
Agarwal R, Hecht TE, Lazo MC, et al. Venous thromboembolism prophylaxis for patients undergoing bariatric surgery: a systematic review. Surger Obes Relat Dis : Off J Am Soc Bariatric Surger. 2010;6(2):213–20. https://doi.org/10.1016/j.soard.2009.11.018.
Homan J, Ruinemans-Koerts J, Aarts EO, et al. Management of vitamin K deficiency after biliopancreatic diversion wit or without duodenal switch. Surg Obes Relat Dis. 2016;12(2):338–44. https://doi.org/10.1016/j.soard.2015.09.021.
Venclauskas L, Maleckas A, Arcelus JI. European guidelines on perioperative venous thromboembolism prophylaxis: surgery in the obese patient. Eur J Anaesthesiol. 2017; nov 6;
K D, Kraaij L, Aarts EO, et al. Fast-track bariatric surgery improves perioperative care and logistics compared to conventional care. Obes Surg. 2015;25(1):28–35. https://doi.org/10.1007/s11695-014-1355-2.
Singh K, Podolsky ER, Um S, et al. Evaluating the safety and efficacy of BMI-based preoperative administration of low-molecular-weight heparin in morbidly obese patients undergoing Roux-en-Y gastric bypass surgery. Obes Surg. 2012;22(1):47–51. https://doi.org/10.1007/s11695-011-0397-y.
Egan G, Ensom MH. Measuring anti-factor xa activity to monitor low-molecular-weight heparin in obesity: a critical review. Can J Hospital Pharm. 2015;68(1):33–47.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Schijns, W., Deenen, M.J., Aarts, E.O. et al. The Effect of Obesity on Anti-Xa Concentrations in Bariatric Patients. OBES SURG 28, 1997–2005 (2018). https://doi.org/10.1007/s11695-018-3130-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3130-2