Abstract
Background
Oesophageal replacement by colonic interposition remains a major challenge due to its complexity and high incidence of complications; here we applied the two-stage operation strategy to oesophageal replacement by colonic interposition in high-risk oesophageal cancer patients following gastrectomy.
Methods
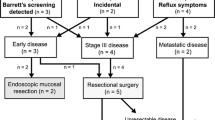
We performed a retrospective analysis on the data of patients with a history of distal gastrectomy who underwent one-stage and two-stage oesophageal replacement by colonic interposition from February 2012 to February 2020, and explored the relationship between the staging strategy and postoperative outcomes.
Results
The clinical data of 93 patients were collected and analysed. There were no significant differences in the patients’ characteristics between the two groups (all p > 0.05), except for comorbidities and Charlson Comorbidity Index (all p < 0.05). The Clavien–Dindo score between the two groups was also not significantly different (p > 0.05). The logistic regression models revealed that patients who had received preoperative therapy had a higher Clavien–Dindo score (p < 0.05), but the stage strategy did not (p > 0.05).
Conclusions
The two-stage operation is feasible in high-risk patients who need to undergo colonic interposition for oesophageal replacement. At the same time, it lowers the technical threshold of colonic interposition for oesophageal replacement, increasing this surgical technique’s acceptability.
Similar content being viewed by others
References
Lee SS, Chung HY, Kwon OK, Yu W. Long-term Quality of Life After Distal Subtotal and Total Gastrectomy: Symptom- and Behavior-oriented Consequences. Annals of surgery. 2016;263(4):738-744. https://doi.org/10.1097/sla.0000000000001481
Im MH, Kim JW, Kim WS, et al. The impact of esophageal reflux-induced symptoms on quality of life after gastrectomy in patients with gastric cancer. Journal of gastric cancer. 2014;14(1):15-22. https://doi.org/10.5230/jgc.2014.14.1.15
Haverkamp L, Seesing MF, Ruurda JP, Boone J, R VH. Worldwide trends in surgical techniques in the treatment of esophageal and gastroesophageal junction cancer. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2017;30(1):1-7. https://doi.org/10.1111/dote.12480
Sert G, Chen SH, Chen HC. Repair of the marginal artery with an interpositional vein graft during colon interposition for esophageal reconstruction. Microsurgery. 2020;40(7):823-824. https://doi.org/10.1002/micr.30618
Daldoul S, Moussi A, Sayari S, Ben Moussa M. Original treatment for ischaemic stenosis of colon interposition: Report of two cases. European annals of otorhinolaryngology, head and neck diseases. 2017;134(1):43-45. https://doi.org/10.1016/j.anorl.2016.08.004
Dewever M, Gomes T, Madrazo Z, López A, Farrán L, Viñals JM. Failed colonic interposition after esophagogastrectomy: What’s the next step? Cirugia espanola. 2016;94(1):54-57. https://doi.org/10.1016/j.ciresp.2014.10.001
Oezcelik A, Banki F, DeMeester SR, et al. Delayed esophagogastrostomy: a safe strategy for management of patients with ischemic gastric conduit at time of esophagectomy. Journal of the American College of Surgeons. 2009;208(6):1030-1034. https://doi.org/10.1016/j.jamcollsurg.2009.02.055
Maish MS, DeMeester SR. Indications and technique of colon and jejunal interpositions for esophageal disease. The Surgical clinics of North America. 2005;85(3):505-514. https://doi.org/10.1016/j.suc.2005.01.014
Brierley JD GM, Wittekind C, editor. TNM Classification of Malignant Tumors, 8th edn. Oxford: Wiley-Blackwell. 2017
Low DE, Alderson D, Cecconello I, et al. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Annals of surgery. 2015;262(2):286-294. https://doi.org/10.1097/sla.0000000000001098
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of surgery. 2004;240(2):205-213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Kamarajah SK, Lin A, Tharmaraja T, et al. Risk factors and outcomes associated with anastomotic leaks following esophagectomy: a systematic review and meta-analysis. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2020;33(3). https://doi.org/10.1093/dote/doz089
Linden PA, Towe CW, Watson TJ, et al. Mortality After Esophagectomy: Analysis of Individual Complications and Their Association with Mortality. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2020;24(9):1948-1954. https://doi.org/10.1007/s11605-019-04346-2
Ohi M, Toiyama Y, Omura Y, et al. Risk factors and measures of pulmonary complications after thoracoscopic esophagectomy for esophageal cancer. Surgery today. 2019;49(2):176-186. https://doi.org/10.1007/s00595-018-1721-0
Situ D, Wei W, Lin P, et al. Do tumor grade and location affect survival in esophageal squamous cell carcinoma? Survival analysis of 302 cases of pT3N0M0 esophageal squamous cell carcinoma. Annals of surgical oncology. 2013;20(2):580-585. https://doi.org/10.1245/s10434-012-2656-0
Li XM, Xu ZZ, Wen ZP, et al. Usefulness of preoperative coronary computed tomography angiography in high risk non-cardiovascular surgery old patients with unknown or suspected coronary artery disease. BMC cardiovascular disorders. 2020;20(1):450. https://doi.org/10.1186/s12872-020-01731-7
Zheng L, Jiang J, Liu Y, Zheng X, Wu C. Correlations of recurrence after radical surgery for esophageal cancer with glucose-lipid metabolism, insulin resistance, inflammation, stress and serum p53 expression. Journal of BUON : official journal of the Balkan Union of Oncology. 2019;24(4):1666-1672
Kassis ES, Kosinski AS, Ross P, Jr., Koppes KE, Donahue JM, Daniel VC. Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. The Annals of thoracic surgery. 2013;96(6):1919-1926. https://doi.org/10.1016/j.athoracsur.2013.07.119
Schizas D, Giannopoulos S, Vailas M, et al. The impact of cirrhosis on esophageal cancer surgery: An up-to-date meta-analysis. American journal of surgery. 2020;220(4):865-872. https://doi.org/10.1016/j.amjsurg.2020.02.035
Morita M, Nakanoko T, Fu**aka Y, et al. In-hospital mortality after a surgical resection for esophageal cancer: analyses of the associated factors and historical changes. Annals of surgical oncology. 2011;18(6):1757-1765. https://doi.org/10.1245/s10434-010-1502-5
Stein HJ, Bartels H, Siewert JR. [Esophageal carcinoma: 2-stage operation for preventing mediastinitis in high risk patients]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. 2001;72(8):881-886. https://doi.org/10.1007/s001040170083
Ong GB, Lam KH, Wong J, Lim TK. Factors influencing morbidity and mortality in esophageal carcinoma. The Journal of thoracic and cardiovascular surgery. 1978;76(6):745-754
Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surgical infections. 2017;18(6):722-735. https://doi.org/10.1089/sur.2017.089