Summary
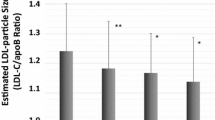
It has been demonstrated that pitavastatin can significantly reduce low-density lipoprotein (LDL) cholesterol (LDL-C), but its impact on lipoprotein subfractions and oxidized low-density lipoprotein (oxLDL) has not been determined. The aim of the present study was to investigate the potential effects of pitavastatin on subfractions of LDL and high-density lipoprotein (HDL) as well as oxLDL in untreated patients with coronary atherosclerosis (AS). Thirty-six subjects were enrolled in this study. Of them, 18 patients with AS were administered pitavastatin 2 mg/day for 8 weeks and 18 healthy subjects without therapy served as controls. The plasma lipid profile, lipoprotein subfractions and circulating oxLDL were determined at baseline and 8 weeks respectively. The results showed that pitavastatin treatment indeed not only decreased LDL-C, total cholesterol (TC), triglycerides (TG) and apolipoprotein B (ApoB) levels, and increased HDL cholesterol (HDL-C), but also reduced the cholesterol concentration of all of the LDL subfractions and the percentage of intermediate and small LDL subfractions. Meanwhile, pitavastatin could decrease plasma oxLDL levels. Furthermore, a more close correlation was found between oxLDL and LDL-C as well as LDL subfractions after pitavastatin treatment. We concluded that a moderate dose of pitavastatin therapy not only decreases LDL-C and oxLDL concentrations but also improves LDL subfractions in patients with AS.
Similar content being viewed by others
References
Mudd JO, Borlaug BA, Johnston PV, et al. Beyond low-density lipoprotein cholesterol: defining the role of low-density lipoprotein heterogeneity in coronary artery disease. J Am Coll Cardiol, 2007,50(18):1735–1741
Reith C, Armitage J.. Management of residual risk after statin therapy. Atherosclerosis, 2016,245:161–170
Xu RX, Zhang Y, Ye P, et al. Analysis of Lipoprotein Subfractions in Chinese Han Patients with Stable Coronary Artery Disease. Heart Lung Circ, 2015,24(12):1203–1210
Qi Y, Fan J, Liu J, et al. Cholesterol-overloaded HDL particles are independently associated with progression of carotid atherosclerosis in a cardiovascular disease-free population: a community-based cohort study. J Am Coll Cardiol, 2015,65(4):355–363
Zhu CG, Zhang Y, Xu RX, et al. Circulating non-HDL-C levels were more relevant to atherogenic lipoprotein subfractions compared with LDL-C in patients with stable coronary artery disease. J Clin Lipidol, 2015,9(6):794–800
Voros S, Joshi P, Qian Z, et al. Apoprotein B, small-dense LDL and impaired HDL remodeling is associated with larger plaque burden and more noncalcified plaque as assessed by coronary CT angiography and intravascular ultrasound with radiofrequency backscatter: results from the ATLANTA I study. J Am Heart Assoc, 2013, 2(6):e000344
Joksić J, Sopić M, Spasojević-Kalimanovska V, et al. Higher circulating resistin protein and PBMCs resistin mRNA levels are associated with increased prevalence of small dense LDL particles in coronary artery disease patients. Clin Exp Pharmacol Physiol, 2016,43(1):22–28
Huang YQ, Cai AP, Chen JY, et al. The relationship of plasma mir-29a and oxidized low density lipoprotein with atherosclerosis. Cell Physiol Biochem, 2016,40(6):1521–1528
Wang A, Yang Y, Su Z, et al. Association of oxidized low-density lipoprotein with prognosis of stroke and stroke subtypes. Stroke, 2017,48(1):91–97
Zhang L, Jia YH, Zhao XS, et al. Trichosanatine alleviates oxidized low-density lipoprotein induced endothelial cells injury via inhibiting the lox-1/p38 mapk pathway. Am J Transl Res, 2016,8(12):5455–5464
Barrios V, Escobar C. Clinical benefits of pitavastatin: focus on patients with diabetes or at risk of develo** diabetes. Future Cardiol, 2016,12(4):449–466
Jeong HS, Hong SJ, Son S, et al. Incidence of new-onset diabetes with 1 mg versus 4 mg pitavastatin in patients at high risk of develo** diabetes during a 3-year follow-up. Cardiovasc Diabetol, 2019,18(1):162–170
Vallejo-Vaz AJ, Kondapally Seshasai SR, Kurogi K, Michishita I, et al. Effect of pitavastatin on glucose, HbA1c and incident diabetes: A meta-analysis of randomized controlled clinical trials in individuals without diabetes. Atherosclerosis, 2015,241(2):409–418
Christogiannis LG, Kostapanos MS, Tellis CC, et al. Distinct effects of fixed combinations of valsartan with either amlodipine or hydrochlorothiazide on lipoprotein subfraction profile in patients with hypertension. J Hum Hypertens, 2013,27(1):44–50
Goliasch G, Oravec S, Blessberger H, et al. Relative importance of different lipid risk factors for the development of myocardial infarction at a very young age (</= 40 years of age). Eur J Clin Invest, 2012,42(6):631–636
El Harchaoui K, van der Steeg WA, Stroes ES, et al. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol, 2007,49(5):547–553
Cromwell WC, Otvos JD, Keyes MJ, et al. LDL Particle Number and Risk of Future Cardiovascular Disease in the Framingham Offspring Study-Implications for LDL Management. J Clin Lipidol, 2007,1(6):583–592
Toft-Petersen AP, Tilsted HH, Aaroe J, et al.. Small dense LDL particles-a predictor of coronary artery disease evaluated by invasive and CT-based techniques: a case-control study. Lipids Health Dis, 2011,10:21–27
Xu RX, Guo YL, Li XL, et al. Impact of short-term low-dose atorvastatin on low-density lipoprotein and high-density lipoprotein subfraction phenotype. Clin Exp Pharmacol Physiol, 2014,41(7):475–481
Saku K, Zhang B, Noda K, et al. Randomized head-to-head comparison of pitavastatin, atorvastatin, and rosuvastatin for safety and efficacy (quantity and quality of LDL): the PATROL trial. Circ J, 2011,75(6):1493–1505
Tokuno A, Hirano T, Hayashi T, et al. The effects of statin and fibrate on lowering small dense LDL-cholesterol in hyperlipidemic patients with type 2 diabetes. J Atheroscler Thromb, 2007,14(3):128–132
Sone H, Takahashi A, Shimano H, et al. HMG-CoA reductase inhibitor decreases small dense low-density lipoprotein and remnant-like particle cholesterol in patients with type-2 diabetes. Life Sci, 2002,71(20):2403–2412
Barylski M, Toth PP, Nikolic D, et al. Emerging therapies for raising high-density lipoprotein cholesterol (HDL-C) and augmenting HDL particle functionality. Best Pract Res Clin Endocrinol Metab, 2014,28(3):453–461
Kypreos KE, Gkizas S, Rallidis LS, et al. HDL particle functionality as a primary pharmacological target for HDL-based therapies. Biochem Pharmacol, 2013,85(11):1575–1578
Salonen JT, Salonen R, Seppanen K, et al. HDL, HDL2, and HDL3 subfractions, and the risk of acute myocardial infarction. A prospective population study in eastern Finnish men. Circulation, 1991,84(1):129–139
Kawano M, Nagasaka S, Yagyu H, et al. Pitavastatin decreases plasma prebeta1-HDL concentration and might promote its disappearance rate in hypercholesterolemic patients. J Atheroscler Thromb, 2008,15(1):41–46.
Kakuda H, Matoba M, Nakatoh H, et al. Comparison of atorvastatin, pitavastatin and rosuvastatin for residual cardiovascular risk using non-fasting blood sampling. Scand J Clin Lab Invest, 2014,74(4):285–295
Frostegard J, Zhang Y, Sun J, et al. Oxidized Low-Density Lipoprotein (OxLDL)-Treated Dendritic Cells Promote Activation of T Cells in Human Atherosclerotic Plaque and Blood, Which Is Repressed by Statins: microRNA let-7c Is Integral to the Effect. J Am Heart Assoc, 2016,5(9):e003976
He L, Xu R, Wang J, et al. Prestroke statins use reduces oxidized low density lipoprotein levels and improves clinical outcomes in patients with atrial fibrillation related acute ischemic stroke. BMC Neurol, 2019,19(1):240–247
Taguchi A, Hayashi S. Study of MDA-LDL by pioglitazone and pitavastatin in patients with type 2 diabetes. Nihon Rinsho, 2011,69(1):100–104
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported, in part, by Capital Special Foundation of Clinical Application Research (No. Z121107001012015), Capital Health Development Fund (No. 201614035), CAMS Major Collaborative Innovation Project (No. 2016-I2M-1-011) and PUMC Youth Fund (No. 3332018200).
Conflict of Interest Statement
No conflict of interests has been disclosured.
Rights and permissions
About this article
Cite this article
Xu, Rx., Zhang, Y., Zhang, Y. et al. Effects of Pitavastatin on Lipoprotein Subfractions and Oxidized Low-density Lipoprotein in Patients with Atherosclerosis. CURR MED SCI 40, 879–884 (2020). https://doi.org/10.1007/s11596-020-2263-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-020-2263-4