Abstract
Purpose
Major Depressive Disorder (MDD) and Insomnia Disorder (ID) are prevalent psychiatric conditions often occurring concurrently, leading to substantial impairment in daily functioning. Understanding the neurobiological underpinnings of these disorders and their comorbidity is crucial for develo** effective interventions. This study aims to analyze changes in functional connectivity within attention networks and default mode networks in patients with depression and insomnia.
Methods
The functional connectivity alterations in individuals with MDD, ID, comorbid MDD and insomnia (iMDD), and healthy controls (HC) were assessed from a cohort of 174 participants. They underwent rs-fMRI scans, demographic assessments, and scale evaluations for depression and sleep quality. Functional connectivity analysis was conducted using region-of-interest (ROI) and whole-brain methods.
Results
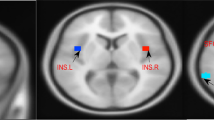
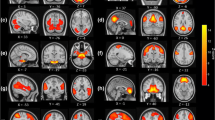
The MDD and iMDD groups exhibited higher Hamilton Depression Scale (HAMD) scores compared to HC and ID groups (P < 0.001). Both ID and MDD groups displayed enhanced connectivity between the left and right orbital frontal cortex compared to HC (P < 0.05), while the iMDD group showed reduced connectivity compared to HC and ID groups (P < 0.05). In the left insula, reduced connectivity with the right medial superior frontal gyrus was observed across patient groups compared to HC (P < 0.05), with the iMDD group showing increased connectivity compared to MDD (P < 0.05). Moreover, alterations in functional connectivity between the left thalamus and left temporal pole were found in iMDD compared to HC and MDD (P < 0.05). Correlation analyses revealed associations between abnormal connectivity and symptom severity in MDD and ID groups.
Conclusions
Our findings demonstrate distinct patterns of altered functional connectivity in individuals with MDD, ID, and iMDD compared to healthy controls. These findings contribute to a better understanding of the pathophysiology of depression and insomnia, which could be used as a reference for the diagnosis and treatments of these patients.







Similar content being viewed by others
Data availability
Data available upon request in line with relevant restrictions, e.g. privacy or ethical.
References
Hoekzema E et al (2014) An independent components and functional connectivity analysis of resting state fMRI data points to neural network dysregulation in adult ADHD. Hum Brain Mapp 35(4):1261–1272
Ferri J et al (2018) Resting-state thalamic dysconnectivity in schizophrenia and relationships with symptoms. Psychol Med 48(15):2492–2499
Wang T et al (2016) Regional homogeneity changes in patients with primary insomnia. Eur Radiol 26(5):1292–1300
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9(1):97–113
Petersen SE, Posner MI (2012) The attention system of the human brain: 20 years after. Annu Rev Neurosci 35:73–89
Bagherzadeh-Azbari S et al (2019) Neuroimaging insights into the link between depression and Insomnia: A systematic review. J Affect Disord 258:133–143
Wang YF et al (2015) Reliable Attention Network Scores and Mutually Inhibited Inter-network Relationships Revealed by Mixed Design and Non-orthogonal Method. Sci Rep 5:10251
Xuan B et al (2016) The activation of interactive attentional networks. Neuroimage 129:308–319
Joo EY et al (2013) Brain Gray Matter Deficits in Patients with Chronic Primary Insomnia. Sleep 36(7):999–1007
Nofzinger EA et al (2004) Functional neuroimaging evidence for hyperarousal in insomnia. Am J Psychiatry 161(11):2126–2128
Keller AS, Ball TM, Williams LM (2020) Deep phenoty** of attention impairments and the “Inattention Biotype” in Major Depressive Disorder. Psychol Med 50(13):2203–2212
Rock PL et al (2014) Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med 44(10):2029–2040
(APA) APA (2013) Diagnostic and Statistical Manual of Mental Disorders V. Text Revision Washington, DC:American Psychiatric Press
Wang H, Mo C, Fang F (2020) Dissociated deficits in attentional networks in social anxiety and depression. Sci China Life Sci 63(7):1071–1078
De Lissnyder E et al (2010) The association between depressive symptoms and executive control impairments in response to emotional and non-emotional information. Cogn Emot 24(2):264–28
Jiang L et al (2018) Altered functional and causal connectivity in attention and default mode network of postconcussional syndrome patients. Chinese J Neurol 17(10):1008—1013
Kaiser RH et al (2015) Large-Scale Network Dysfunction in Major Depressive Disorder: A Meta-analysis of Resting-State Functional Connectivity. JAMA Psychiat 72(6):603–611
Cheng W et al (2016) Medial reward and lateral non-reward orbitofrontal cortex circuits change in opposite directions in depression. Brain 139(Pt 12):3296–3309
Nie X et al (2015) Functional connectivity of paired default mode network subregions in primary insomnia. Neuropsychiatr Dis Treat 11:3085–3093
Lin P et al (2016) Static and dynamic posterior cingulate cortex nodal topology of default mode network predicts attention task performance. Brain Imaging Behav 10(1):212–225
Whitfield-Gabrieli S, Ford JM (2012) Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol 8:49–76
Smith V, Mitchell DJ, Duncan J (2018) Role of the Default Mode Network in Cognitive Transitions. Cereb Cortex 28(10):3685–3696
Zhu X et al (2017) Rumination and Default Mode Network Subsystems Connectivity in First-episode, Drug-Naive Young Patients with Major Depressive Disorder. Sci Rep 7:43105
Brakowski J et al (2017) Resting state brain network function in major depression - Depression symptomatology, antidepressant treatment effects, future research. J Psychiatr Res 92:147–159
Philippi CL et al (2018) Neural and behavioral correlates of negative self-focused thought associated with depression. Hum Brain Mapp 39(5):2246–2257
Guo W et al (2018) Increased anterior default-mode network homogeneity in first-episode, drug-naive major depressive disorder: A replication study. J Affect Disord 225:767–772
Rolls ET (2016) A non-reward attractor theory of depression. Neurosci Biobehav Rev 68:47–58
Rolls ET (2017) The roles of the orbitofrontal cortex via the habenula in non-reward and depression, and in the responses of serotonin and dopamine neurons. Neurosci Biobehav Rev 75:331–334
Feffer K et al (2018) 1Hz rTMS of the right orbitofrontal cortex for major depression: Safety, tolerability and clinical outcomes. Eur Neuropsychopharmacol 28(1):109–117
Fossati P (2013) Imaging autobiographical memory. Dialogues Clin Neurosci 15(4):487–490
Freton M et al (2014) The eye of the self: precuneus volume and visual perspective during autobiographical memory retrieval. Brain Struct Funct 219(3):959–968
Delaveau P et al (2016) Antidepressant short-term and long-term brain effects during self-referential processing in major depression. Psychiatry Res Neuroimaging 247:17–24
Acknowledgements
This work was supported by the programs of the National Natural Science Foundation of China International Cooperation and Exchange Project (81761128036); National Natural Science Foundation of China Regional Science Fund Project (81960262, 81560235, 31760294); Guizhou Provincial Precision Diagnosis and Treatment International Scientific Cooperation Base for Severe Depressive Disorders (Guizhou Science and Technology Cooperation Platform Talent [2018]5802); Guizhou Province High-Level Innovative Talent Training Program—Hundred-Level Talent (Guizhou Science and Technology Cooperation Platform Talent [2016]5679); Guiyang Science and Technology Plan Project (Zhu Ke Contract [2018]1-94)
Funding
This work was supported by the programs of the National Natural Science Foundation of China International Cooperation and Exchange Project (81761128036); National Natural Science Foundation of China Regional Science Fund Project (81960262, 81560235, 31760294); Guizhou Provincial Precision Diagnosis and Treatment International Scientific Cooperation Base for Severe Depressive Disorders (Guizhou Science and Technology Cooperation Platform Talent [2018]5802); Guizhou Province High-Level Innovative Talent Training Program—Hundred-Level Talent (Guizhou Science and Technology Cooperation Platform Talent [2016]5679); Guiyang Science and Technology Plan Project (Zhu Ke Contract [2018]1–94).
Author information
Authors and Affiliations
Contributions
Yong-xue Hu, **g-yu Shi, Guang-yuan **a, Long-fei Liu, Pei-fan Li, Qing Shan and Yi-ming Wang designed the study. Yong-xue Hu and Yi-ming Wang participated in the conception of the study. **g-yu Shi, Guang-yuan **a, Long-fei Liu, Pei-fan Li and Qing Shan managed and conducted the statistical analyses and interpreted the data. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, Yx., Shi, Jy., **a, Gy. et al. Analysis of functional connectivity changes in attention networks and default mode networks in patients with depression and insomnia. Sleep Breath (2024). https://doi.org/10.1007/s11325-024-03064-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-024-03064-7