Abstract
Purpose
To assess changes in sleep-related symptoms in patients with breast cancer, endometrial cancer and melanoma previously examined for sleep-related symptoms and the presence of PSG (polysomnography)-determined OSA, ≥ 3 years post-treatment; and to evaluate how CPAP treatment affects sleep-related symptoms in patients previously diagnosed with OSA.
Methods
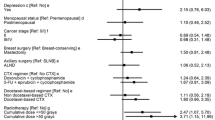
Patients initially recruited from breast cancer, endometrial cancer, and melanoma follow-up clinics at Westmead Hospital (Sydney, Australia) participated in this questionnaire-based study. Demographic and change in cancer status data were collected at follow-up. Patients completed the Pittsburgh Sleep Quality Index [poor sleep quality, PSQITOTAL ≥ 5au], Insomnia Severity Index, Epworth Sleepiness Scale and Functional Outcomes of Sleep Questionnaire; with ΔPSQITOTAL ≥ 3au indicating a clinically meaningful change in sleep quality over follow-up. PSG-determined OSA was confirmed using the apnoea-hypopnoea index. CPAP compliance was determined via self-report (CPAP compliant, CPAP; not compliant, non-CPAP). Logistic regression models determined if changes in cancer status, AHI, cancer subgroup or CPAP treatment was predictive of ΔPSQITOTAL ≥ 3 au and p < 0.05 indicated statistical significance.
Results
The 60 patients recruited had breast cancer (n = 22), endometrial cancer (n = 15), and melanoma (n = 23). Cancer subgroups were similarly aged, and all had median follow-up PSQITOTAL scores ≥ 5au; breast cancer patients scoring the highest (p < 0.05). The CPAP group had significantly reduced PSQITOTAL scores (p = 0.02) at follow-up, unlike the non-CPAP group. Cancer subgroups had similar median ISITOTAL, ESSTOTAL and FOSQ-10TOTAL scores at follow-up, regardless of CPAP treatment. There were no significant predictors of ΔPSQITOTAL ≥ 3 au at follow-up.
Conclusion
Sleep-related symptoms persist in patients with cancer ≥ 3 years after treatment, although these symptoms improve with CPAP. Future studies should evaluate how CPAP affects survival outcomes in cancer patients with comorbid OSA.



Similar content being viewed by others
Data availability
The datasets generated and analysed in the current study are available from the corresponding author, on reasonable request.
References
Lowery-Allison A et al (2018) Sleep problems in breast cancer survivors 1–10 years posttreatment. Palliat Support Care 16(3):325–334. https://doi.org/10.1017/S1478951517000311
Kairaitis K et al (2022) Cancer sleep symptom-related phenotypic clustering differs across three cancer specific patient cohorts. J Sleep Res 31(5):e13588. https://doi.org/10.1111/jsr.13588
Lis C, Gupta D, Grutsch J (2008) The relationship between insomnia and patient satisfaction with quality of life in cancer. Support Care Cancer 16(3):261–266. https://doi.org/10.1007/S00520-007-0314-Z/TABLES/4
Palesh O et al (2014) Actigraphy-measured sleep disruption as a predictor of survival among women with advanced breast cancer. Sleep 37(5):837–842. https://doi.org/10.5665/SLEEP.3642
Lee LJ, Ross A, Griffith K (2020) Symptom clusters in breast cancer survivors: a latent class profile analysis. Oncol Nurs Forum 47(1):89–100. https://doi.org/10.1188/20.ONF.89-100
Ye L et al (2014) The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J 44(6):1600–1607. https://doi.org/10.1183/09031936.00032314
Cabezas E et al (2019) Sleep disordered breathing is highly prevalent in patients with lung cancer: results of the sleep apnea in lung cancer study. Respiration 97(2):119–124. https://doi.org/10.1159/000492273
Campos-Rodriguez F et al (2022) Association between sleep-disordered breathing and prostate cancer. Sleep Med 91:35–42. https://doi.org/10.1016/J.SLEEP.2022.02.007
Subramanian H et al (2022) Screening for obstructive sleep apnoea in post-treatment cancer patients. Cancer Rep 6(3):e1740. https://doi.org/10.1002/cnr2.1740
Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin C (2011) Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J Clin Oncol 29(26):3580–3586. https://doi.org/10.1200/JCO.2010.33.2247
Chan J et al (2023) Trajectories of sleep disturbance in cancer survivors during the first two years post-treatment. Sleep. https://doi.org/10.1093/sleep/zsad052
Berry R et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events: deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Med 8(5):597. https://doi.org/10.5664/JCSM.2172
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Johns MW (1991) A new method for measuring daytime sleepiness: the epworth sleepiness scale. Sleep 14(6):540–545. https://doi.org/10.1093/SLEEP/14.6.540
Bastien CH, Vallières A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2(4):297–307. https://doi.org/10.1016/S1389-9457(00)00065-4
Chasens E, Ratcliffe S, Weaver T (2009) Development of the FOSQ-10: a short version of the functional outcomes of sleep questionnaire. Sleep 32(7):919. https://doi.org/10.1093/SLEEP/32.7.915
Hughes C et al (2009) Acupuncture and reflexology for insomnia: a feasibility study. Acupunct Med 27(4):163–168. https://doi.org/10.1136/AIM.2009.000760
Morin C, Belleville G, Bélanger L, Ivers H (2011) The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 34(5):601–608. https://doi.org/10.1093/sleep/34.5.601
Shisler R, Sinnott J, Wang V, Hebert C, Salani R, Felix A (2018) Life after endometrial cancer: a systematic review of patient-reported outcomes. Gynecol Oncol 148(2):403–413. https://doi.org/10.1016/J.YGYNO.2017.11.007
Jacobsen A et al (2017) Determinants for adherence to continuous positive airway pressure therapy in obstructive sleep apnea. PLoS ONE 12(12):e0189614. https://doi.org/10.1371/journal.pone.0189614
Kim J (2019) Multicollinearity and misleading statistical results. Korean J Anesthesiol 72(6):558–569. https://doi.org/10.4097/kja.19087
Ancoli-Israel S et al (2014) Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Support Care Cancer 22(9):2535–2545. https://doi.org/10.1007/s00520-014-2204-5
Forsse D et al (2022) Longitudinal effects of adjuvant chemotherapy and lymph node staging on patient-reported outcomes in endometrial cancer survivors: a prospective cohort study. Am J Obstet Gynecol 226(1). https://doi.org/10.1016/j.ajog.2021.08.011
Ziefle S et al (2011) Health-related quality of life before and during adjuvant interferon-α treatment for patients with malignant melanoma (DeCOG-Trial). J Immunother 34(4):403–408. https://doi.org/10.1097/CJI.0b013e31821b7a4b
Kondratavičienė L, Malakauskas K, Vaitukaitienė G, Balsevičius T, Žemaitis M, Miliauskas S (2022) Short-term continuous positive air pressure treatment: effects on quality of life and sleep in patients with obstructive sleep apnea. Medicina (B Aires) 58(3):350. https://doi.org/10.3390/medicina58030350
Glidewell R, Renn B, Roby E, Orr W (2014) Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med 15(8):899–905. https://doi.org/10.1016/j.sleep.2014.05.001
Antic N et al (2011) The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep 34(1):111–119. https://doi.org/10.1093/sleep/34.1.111
Justeau G et al (2022) Cancer risk in patients with sleep apnoea following adherent 5-year CPAP therapy. Eur Respir J 59(4). https://doi.org/10.1183/13993003.01935-2021
Martínez-García MA et al (2014) Obstructive sleep apnea is associated with cancer mortality in younger patients. Sleep Med 15(7):742–748. https://doi.org/10.1016/J.SLEEP.2014.01.020
Douglas J et al (2017) Guidelines for sleep studies in adults - a position statement of the Australasian Sleep Association. Sleep Med 36(Suppl 1):S2–S22. https://doi.org/10.1016/J.SLEEP.2017.03.019
Acknowledgements
The authors would like to thank Ayey Madut, Hong Man, Catherine Kennedy, Annie Stenlake, Masrura Kabir, Alissa Phung, Ragini Gengiah, Professor Christine L. Clarke, Associate Professor Nirmala Pathmanathan, Associate Professor James French, Dr Kristina Lindemann, Dr Robyn Sayers, Professor Paul Harnett, and Professor John Wheatley for their assistance with this study, alongside the Sydney West Translational Cancer Research Centre.
Funding
This study was funded by the Sydney West Translational Cancer Research Centre, Grant/Award Number: 15/TRC/1–01; Neil and Norma Hill Foundation; ResMed Foundation; Strategic Priorities Areas for Research Collaboration Grant from the University of Sydney.
Author information
Authors and Affiliations
Contributions
Harini Subramanian: Data curation (lead); formal analysis (lead); visualization (lead); writing – original draft (equal); writing – review and editing (lead). Ritu Trivedi: Data curation (supporting), investigation (lead), writing – review and editing (supporting). Veronika Fuchsova: Data curation (supporting); formal analysis (lead); investigation (supporting), writing – review and editing (supporting). Elisabeth Elder: Funding acquisition (supporting); resources (equal); writing – review and editing (supporting). Alison Brand: Funding acquisition (supporting); resources (equal); writing – review and editing (supporting). Julie Howle: Funding acquisition (supporting); resources (equal); writing – review and editing (supporting). Anna deFazio: Funding acquisition (supporting); resources (equal); writing – review and editing (supporting). Graham J Mann: Funding acquisition (supporting); resources (equal); writing – review and editing (supporting). Terence Amis: Conceptualization (equal); formal analysis (supporting); funding acquisition (lead); methodology (equal); project administration (equal); supervision (equal); visualization (supporting); writing – original draft (equal); writing – review and editing (lead). Kristina Kairaitis: Conceptualization (equal); formal analysis (supporting); funding acquisition (lead); methodology (equal); project administration (lead); supervision (equal); visualization (supporting); writing – original draft (equal); writing – review and editing (lead).
Corresponding author
Ethics declarations
The authors explicitly state that there are no conflicts of interest in relation to this article. Anna DeFazio declares receiving research grants and honoraria from AstraZeneca, although not in connection to the subject matter or materials discussed in this manuscript. Kristina Kairaitis declares receiving honoraria for sleep education from SomnoMed.
Ethics approval
Approval was obtained from the Western Sydney Local Health District Ethics Committee (HREC: AU RED LNR/18/WMEAD/418). Procedures used in this study adhere to the principles of the Declaration of Helsinki.
Consent to participate and publish
Informed consent was obtained from all individual participants included in the study. All participants signed informed consent regarding publishing their data.
Competing interests
The authors have no competing interests to declare, that are relevant to the content of this article. Anna DeFazio declares receiving research grants and honoraria from AstraZeneca, although not in connection to the subject matter or materials discussed in this manuscript. Kristina Kairaitis declares receiving honoraria for sleep education from SomnoMed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Subramanian, H., Trivedi, R., Fuchsova, V. et al. Follow-up assessment of sleep-related symptoms in patients after treatment for cancer: responses to continuous positive airway pressure treatment for co-morbid obstructive sleep apnoea. Sleep Breath 28, 725–733 (2024). https://doi.org/10.1007/s11325-023-02946-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02946-6