Abstract
Purpose
The current study was conducted to explore the clinical features and risk factors of patients with asthma complicated by obstructive sleep apnea-hypopnea syndrome (OSAHS).
Methods
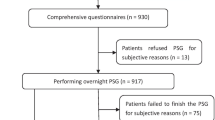
Patients with asthma who underwent polysomnography in our hospital from August 2017 to December 2019 were enrolled in the study. Data on demographics, pulmonary function testing, polysomnography, blood gases, mean pulmonary artery pressure, and vascular endothelial growth factor (VEGF) were compared between the two groups.
Results
Of 238 patients with asthma, 93 who also had OSAHS formed the observation group and were subclassified into mild (n = 33), moderate (n = 41), and severe (n = 19) categories, while 145 patients with asthma alone were assigned to the control group. No significant differences were found in sex, age, course of disease, or pulmonary function between the two groups (P > 0.05), while the observation group showed more frequent allergic rhinitis and had greater BMI, neck circumference, mean pulmonary artery pressure (mPAP), and VEGF than those in the control group (P < 0.001). The peak expiratory flow (PEF), forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and FEV1/FVC in the mild group and the moderate group were higher than those in the severe group (P < 0.001). The durations of AHI and SaO2 < 90% in the mild group and the moderate group were shorter than that in the severe group, and the lowest level of SaO2 in the mild group and the moderate group was higher than that in the severe group (P < 0.05). The mPAP and VEGF of the mild and moderate groups were lower than those of severe group (P < 0.001), with mild group lower than moderate group (P < 0.001).
Conclusion
Significant differences in allergic rhinitis, BMI, neck circumference, AHI, SaO2, mPAP, and VEGF were observed in patients with asthma complicated by OSAHS. These parameters are risk factors associated with asthma complicated by OSAHS.
Similar content being viewed by others
References
Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, Bai C, Kang J, Ran P, Shen H, Wen F, Chen Y, Sun T, Shan G, Lin Y, Xu G, Wu S, Wang C, Wang R, Shi Z, Xu Y, Ye X, Song Y, Wang Q, Zhou Y, Li W, Ding L, Wan C, Yao W, Guo Y, **ao F, Lu Y, Peng X, Zhang B, **ao D, Wang Z, Chen Z, Bu X, Zhang H, Zhang X, An L, Zhang S, Zhu J, Cao Z, Zhan Q, Yang Y, Liang L, Tong X, Dai H, Cao B, Wu T, Chung KF, He J, Wang C (2019) Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet. 394(10196):407–418. https://doi.org/10.1016/s0140-6736(19)31147-x
Lu K, Zhao Y, Chen J, Hu DY, **ao H (2020) Interactive association of sleep duration and sleep quality with the prevalence of metabolic syndrome in adult Chinese males. Experimental and therapeutic medicine 19(2):841–848. https://doi.org/10.3892/etm.2019.8290
Mahesh M (2020) Family Physician's knowledge, awareness and practices about peak flow meters in the management of bronchial asthma - a Study from Mysore City, South India. J Assoc Physicians India 68(1):82
M M. Family Physician's Knowledge (2020) Awareness and Practices about Peak Flow Meters in the management of Bronchial Asthma - a Study from Mysore City, South India. The Journal of the Association of Physicians of India 68(1):80
Mao T, Zhang J (2019) Uncovering synergistic mechanism of Chinese herbal medicine in the treatment of atrial fibrillation with obstructive sleep apnea hypopnea syndrome by network pharmacology. 2019:8691608–8691613. https://doi.org/10.1155/2019/8691608
Schulz S, Ritter J, Schneider G, Guntinas-Lichius O, Voss A (2019) Risk detection in patients with obstructive sleep apnea syndrome based on cardiovascular time series analysis. Conf Proc IEEE Eng Med Biol Soc 2019:6794–6797. https://doi.org/10.1109/embc.2019.8856472
Yang X, **ao Y, Han B, Lin K, Niu X, Chen X (2019) Implication of mixed sleep apnea events in adult patients with obstructive sleep apnea-hypopnea syndrome. Sleep Breath 23(2):559–565. https://doi.org/10.1007/s11325-018-1745-0
Singh A, Prasad R, Garg R, Kant S, Hosmane GB, Dubey A, Agarwal A, Verma RK (2017) A study to estimate prevalence and risk factors of obstructive sleep apnoea syndrome in a semi-urban Indian population. Monaldi Arch Chest Dis 87(1):773. https://doi.org/10.4081/monaldi.2017.773
Tsoy UA, Sviryaev YV, Korostovtseva LS, Semenov AP, Vaulina DA, Nepran VI et al (2015) Clinical features of obstructive sleep apnea syndrome in patients with acromegaly. Ter Arkh 87(4):47–52. https://doi.org/10.17116/terarkh201587447-52
Alkhalil M, Schulman E, Getsy J (2009) Obstructive sleep apnea syndrome and asthma: what are the links? J Clin Sleep Med 5(1):71–78
Oyama B, Tsuburai T, Tsuruoka H, Nishida K, Usuba A, Hida N, Inoue T, Komase Y, Mineshita M, Miyazawa T (2019) Complicating effects of obstructive sleep apnea syndrome on the severity of adult asthma. J Asthma:1–6. https://doi.org/10.1080/02770903.2019.1652643
Group CMARBA (2008) Guidelines for the prevention and treatment of bronchial asthma (definition, diagnosis, treatment and management of bronchial asthma). Chinese Journal of Tuberculosis and Respiratory Diseases 31(3):177–185
Department of Respiratory Diseases CMA (2003) Guidelines for the diagnosis and treatment of obstructive sleep apnea hypopnea syndrome (draft). Chinese Journal of Otorhinolaryngology Head and Neck Surgery 15(3):192–195
Kilaikode S, Weiss M, Megalaa R, Perez G, Nino G (2019) Asthma is associated with increased probability of needing CPAP in children with severe obstructive sleep apnea. Pediatr Pulmonol 54(3):342–347. Epub 2019/01/12. https://doi.org/10.1002/ppul.24245
Wang J, **e Y, Ma W (2015) The research progress of relationship between the obstructive sleep apnea hypopnea syndrome and asthma. Lin chuang er bi yan hou tou **g wai ke za zhi = Journal of clinical otorhinolaryngology, head, and neck surgery 29(4):381–384
Lu Y, Gu Q, Pang C, Gao F, Liu C, Du J et al (2014) Treatment of obstructive sleep apnea-hypopnea syndrome for children refractory asthma, Zhonghua er bi yan hou tou **g wai ke za zhi = Chinese journal of otorhinolaryngology head and neck surgery. 49(6):462–467
Korn S (2005) Nasal and bronchial provocation with allergen in patients with mild asthma and allergic rhinitis -- similarities and differences. Pneumologie. 59(10):717–719. https://doi.org/10.1055/s-2005-915561
Zhang RH, Zhao W, Shu LP, Wang N, Cai YH, Yang JK et al (2020. doi: ARTN e13046) Obstructive sleep apnea is associated with coronary microvascular dysfunction: a systematic review from a clinical perspective. J Sleep Res. https://doi.org/10.1111/jsr.13046
Li LW, Xu ZW, ** XM, Yan CH, Jiang F, Tong SL et al (2015) Sleep-disordered breathing and asthma: evidence from a large multicentric epidemiological study in China. Resp Res 16. doi: ARTN 56. https://doi.org/10.1186/s12931-015-0215-5
Wang Y, Liu K, Hu K, Yang J, Li Z, Nie M, Dong Y, Huang H, Chen J (2016) Impact of obstructive sleep apnea on severe asthma exacerbations. Sleep Med 26:1–5. https://doi.org/10.1016/j.sleep.2016.06.013
Huang L, Yu JL (2019) Validation of NoSAS score and obstructive sleep apnea hypopnea syndrome screening model for female snorers in females with obstructive sleep apnea. Zhongguo yi xue ke xue yuan xue bao Acta Academiae Medicinae Sinicae 41(6):825–831. https://doi.org/10.3881/j.issn.1000-503X.11131
Julien JY, Martin JG, Ernst P, Olivenstein R, Hamid Q, Lemiere C et al (2009) Prevalence of obstructive sleep apnea-hypopnea in severe versus moderate asthma. J Allergy Clin Immunol 124(2):371–376. https://doi.org/10.1016/j.jaci.2009.05.016
Teodorescu M, Consens FB, Bria WF, Coffey MJ, McMorris MS, Weatherwax KJ et al (2009) Predictors of habitual snoring and obstructive sleep apnea risk in patients with asthma. Chest. 135(5):1125–1132. https://doi.org/10.1378/chest.08-1273
Castillo MFR, Cohen A, Edberg D, Hoppensteadt D, Fareed J, Martin B, Halaris A (2020) Vascular endothelial growth factor in bipolar depression: a potential biomarker for diagnosis and treatment outcome prediction. Psychiatry Res 284:112781. https://doi.org/10.1016/j.psychres.2020.112781
Luo W, Miao DS, He F (2006) Correlation of body mass index, neck circumference and obstructive sleep apnea hypopnea syndrome. Zhonghua er bi yan hou tou **g wai ke za zhi = Chinese journal of otorhinolaryngology head and neck surgery 41(6):460–461
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethics approval
The study protocol was approved by the Ethics Committee of Bei**g Chaoyang Hospital, Capital Medical University.
Informed consent
Written informed consent was obtained from all the study subjects before enrollment.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, JL., Feng, XK., Zhang, DM. et al. Clinical features and risk factors in patients with asthma complicated with obstructive sleep apnea-hypopnea syndrome: a hospital-based study. Sleep Breath 25, 339–345 (2021). https://doi.org/10.1007/s11325-020-02127-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02127-9