Abstract
Mechanical thrombectomy (MT) is the standard of care for patients with acute ischemic stroke from large vessel occlusion (AIS-LVO). The association of blood pressure variability (BPV) during MT and outcomes are unknown. We leveraged a supervised machine learning algorithm to predict patient characteristics that are associated with BPV indices. We performed a retrospective review of our comprehensive stroke center’s registry of all adult patients undergoing MT between 01/01/2016 and 12/31/2019. The primary outcome was poor functional independence, defined as 90-day modified Rankin Scale (mRS) ≥ 3. We used probit analysis and multivariate logistic regressions to evaluate the association of patients’ clinical factors and outcomes. We applied a machine learning algorithm (random forest, RF) to determine predictive factors for the different BPV indices during MT. Evaluation was performed with root-mean-square error (RMSE) and normalized-RMSE (nRMSE) metrics. We analyzed 375 patients with mean age (± standard deviation [SD]) of 65 (15) years. There were 234 (62%) patients with mRS ≥ 3. Univariate probit analysis demonstrated that BPV during MT was associated with poor functional independence. Multivariable logistic regression showed that age, admission National Institutes of Health Stroke Scale (NIHSS), mechanical ventilation, and thrombolysis in cerebral infarction (TICI) score (OR 0.42, 95% CI 0.17–0.98, P = 0.044) were significantly associated with outcome. RF analysis identified that the interval from last-known-well time-to-groin puncture, age, and mechanical ventilation were among important factors significantly associated with BPV. BPV during MT was associated with functional outcome in univariate probit analysis but not in multivariable regression analysis, however, NIHSS and TICI score were. RF algorithm identified risk factors influencing patients’ BPV during MT. While awaiting further studies’ results, clinicians should still monitor and avoid high BPV during thrombectomy while triaging AIS-LVO candidates quickly to MT.
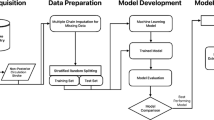
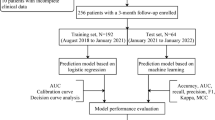
Graphical abstract





Similar content being viewed by others
Data availability
Data cannot be shared per our institution’s IRB agreement.
References
Tran QK, Yarbrough KL, Capobianco P et al (2020) Comparison of outcomes after treatment of large vessel occlusion in a critical care resuscitation unit or a neurocritical care unit. Neurocrit Care 32(3):725–733. https://doi.org/10.1007/s12028-019-00825-1
Goyal M, Demchuk AM, Menon BK et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372(11):1019–1030. https://doi.org/10.1056/NEJMoa1414905
Linfante I, Starosciak AK, Walker GR et al (2016) Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J Neurointerv Surg 8(3):224–229. https://doi.org/10.1136/neurintsurg-2014-011525
Sallustio F, Motta C, Pizzuto S et al (2017) CT angiography-based collateral flow and time to reperfusion are strong predictors of outcome in endovascular treatment of patients with stroke. J Neurointerv Surg 9(10):940–943. https://doi.org/10.1136/neurintsurg-2016-012628
Manning LS, Mistri AK, Potter J, Rothwell PM, Robinson TG (2015) Short-term blood pressure variability in acute stroke: post hoc analysis of the controlling hypertension and hypotension immediately post stroke and continue or stop post-stroke antihypertensives collaborative study trials. Stroke 46(6):1518–1524. https://doi.org/10.1161/STROKEAHA.115.009078
Cernik D, Sanak D, Divisova P et al (2019) Impact of blood pressure levels within first 24 hours after mechanical thrombectomy on clinical outcome in acute ischemic stroke patients. J Neurointerv Surg 11(8):735–739. https://doi.org/10.1136/neurintsurg-2018-014548
Bennett AE, Wilder MJ, McNally JS et al (2018) Increased blood pressure variability after endovascular thrombectomy for acute stroke is associated with worse clinical outcome. J Neurointerv Surg 10(9):823–827. https://doi.org/10.1136/neurintsurg-2017-013473
Mistry EA, Mehta T, Mistry A et al (2020) Blood pressure variability and neurologic outcome after endovascular thrombectomy: a secondary analysis of the BEST study. Stroke 51(2):511–518. https://doi.org/10.1161/STROKEAHA.119.027549
Chang JY, Jeon SB, Lee JH, Kwon OK, Han MK (2018) The relationship between blood pressure variability, recanalization degree, and clinical outcome in large vessel occlusive stroke after an intra-arterial thrombectomy. Cerebrovasc Dis 46(5–6):279–286. https://doi.org/10.1159/000495300
Naito H, Hosomi N, Kuzume D et al (2020) Increased blood pressure variability during the subacute phase of ischemic stroke is associated with poor functional outcomes at 3 months. Sci Rep 10(1):811. https://doi.org/10.1038/s41598-020-57661-z
Fukuda K, Kai H, Kamouchi M et al (2015) Day-by-day blood pressure variability and functional outcome after acute ischemic stroke: fukuoka stroke registry. Stroke 46(7):1832–1839. https://doi.org/10.1161/STROKEAHA.115.009076
Tran QK, Najafali D, Tiffany L et al (2021) Effect of blood pressure variability on outcomes in emergency patients with intracranial hemorrhage. West J Emerg Med 22(2):177–185. https://doi.org/10.5811/westjem.2020.9.48072
Tiffany L, Haase DJ, Boswell K et al (2021) Care intensity of spontaneous intracranial hemorrhage: effectiveness of the critical care resuscitation unit. Am J Emerg Med 46:437–444. https://doi.org/10.1016/j.ajem.2020.10.044
Shriki J, Johnson L, Patel P et al (2020) Transport blood pressures and outcomes in stroke patients requiring thrombectomy. Air Med J 39(3):166–172. https://doi.org/10.1016/j.amj.2020.03.002
Tsoi KKF, Chan NB, Yiu KKL, Poon SKS, Lin B, Ho K (2020) Machine learning clustering for blood pressure variability applied to systolic blood pressure intervention trial (SPRINT) and the Hong Kong community cohort. Hypertension 76(2):569–576. https://doi.org/10.1161/HYPERTENSIONAHA.119.14213
Abedi V, Razavi SM, Khan A et al (2021) Artificial intelligence: a shifting paradigm in cardio-cerebrovascular medicine. J Clin Med. https://doi.org/10.3390/jcm10235710
Koshimizu H, Kojima R, Kario K, Okuno Y (2020) Prediction of blood pressure variability using deep neural networks. Int J Med Inform 136:104067. https://doi.org/10.1016/j.ijmedinf.2019.104067
Goh KH, Wang L, Yeow AYK et al (2021) Artificial intelligence in sepsis early prediction and diagnosis using unstructured data in healthcare. Nat Commun 12(1):711. https://doi.org/10.1038/s41467-021-20910-4
Wei C, Zhang L, Feng Y, Ma A, Kang Y (2022) Machine learning model for predicting acute kidney injury progression in critically ill patients. BMC Med Inform Decis Mak 22(1):17. https://doi.org/10.1186/s12911-021-01740-2
Maier B, Fahed R, Khoury N et al (2019) Association of blood pressure during thrombectomy for acute ischemic stroke with functional outcome: a systematic review. Stroke 50(10):2805–2812. https://doi.org/10.1161/STROKEAHA.119.024915
Anadani M, Orabi MY, Alawieh A et al (2019) Blood pressure and outcome after mechanical thrombectomy with successful revascularization. Stroke 50(9):2448–2454. https://doi.org/10.1161/STROKEAHA.118.024687
de Havenon A, Stoddard G, Saini M et al (2019) Increased blood pressure variability after acute ischemic stroke increases the risk of death: a secondary analysis of the virtual international stroke trial archive. JRSM Cardiovasc Dis 8:2048004019856496. https://doi.org/10.1177/2048004019856496
Valent A, Sajadhoussen A, Maier B et al (2020) A 10% blood pressure drop from baseline during mechanical thrombectomy for stroke is strongly associated with worse neurological outcomes. J Neurointerv Surg 12(4):363–369. https://doi.org/10.1136/neurintsurg-2019-015247
Chang JY, Jeon SB, Jung C, Gwak DS, Han MK (2019) Postreperfusion blood pressure variability after endovascular thrombectomy affects outcomes in acute ischemic stroke patients with poor collateral circulation. Front Neurol 10:346. https://doi.org/10.3389/fneur.2019.00346
Mattle HP, Kappeler L, Arnold M et al (2005) Blood pressure and vessel recanalization in the first hours after ischemic stroke. Stroke 36(2):264–268. https://doi.org/10.1161/01.STR.0000153052.59113.89
Schonenberger S, Uhlmann L, Hacke W et al (2016) Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA 316(19):1986–1996. https://doi.org/10.1001/jama.2016.16623
Lowhagen Henden P, Rentzos A, Karlsson JE et al (2017) General anesthesia versus conscious sedation for endovascular treatment of acute ischemic stroke: the anstroke trial (anesthesia during stroke). Stroke 48(6):1601–1607. https://doi.org/10.1161/STROKEAHA.117.016554
Simonsen CZ, Yoo AJ, Sorensen LH et al (2018) Effect of general anesthesia and conscious sedation during endovascular therapy on infarct growth and clinical outcomes in acute ischemic stroke: a randomized clinical trial. JAMA Neurol 75(4):470–477. https://doi.org/10.1001/jamaneurol.2017.4474
Acknowledgements
The authors would like to thank Professor Ruoqing Zhu, Ph.D. from the University of Illinois Urbana-Champaign for his assistance with R.
Funding
The authors received no funding for data collection or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
DN: Conceptualization, Data Analysis, Data Curation, Writing—Original Draft Preparation, Writing—Reviewing and Editing. TJ: Conceptualization, Data Analysis, Writing—Original Draft Preparation, Writing—Reviewing and Editing. MP: Conceptualization, Data Curation, Writing—Reviewing and Editing. AB: Conceptualization, Data Curation, Writing—Reviewing and Editing. MU: Data Curation, Writing—Reviewing and Editing. KV: Data Curation, Writing—Reviewing and Editing. BP: Data Curation, Writing—Reviewing and Editing. MS: Writing—Reviewing and Editing. KLY: Conceptualization, Data Curation, Writing—Reviewing and Editing. MSP: Conceptualization, Data Curation, Writing—Reviewing and Editing. GJ: Conceptualization, Data Curation, Writing—Reviewing and Editing. QKT: Conceptualization, Supervision, Data Curation, Data Curation, Writing—Original Draft Preparation, Writing—Reviewing and Editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the University of Maryland Baltimore’s IRB (IRB number: HP-00084554).
Informed consent
Our study was exempt from formal consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data from this article were presented virtually in part at the 2021 Annual Congress of the Society of Critical Care Medicine.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Najafali, D., Johnstone, T., Pergakis, M. et al. Prediction of blood pressure variability during thrombectomy using supervised machine learning and outcomes of patients with ischemic stroke from large vessel occlusion. J Thromb Thrombolysis 56, 12–26 (2023). https://doi.org/10.1007/s11239-023-02796-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02796-9