Abstract
Purpose
Mental health and well-being trajectories are not expected to be homogeneous in diverse clinical populations. This exploratory study aims to identify subgroups of patients with cancer receiving radiation therapy who have different mental health and well-being trajectories, and examine which socio-demographic, physical symptoms, and clinical variables are associated with such trajectories.
Methods
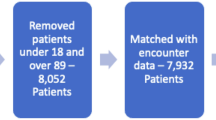
Retrospective analysis of radiation therapy patients diagnosed with cancer in 2017 was conducted using data from the Ontario Cancer Registry (Canada) and linked with administrative health data. Mental health and well-being were measured using items from the Edmonton Symptom Assessment System—revised questionnaire. Patients completed up to 6 repeated measurements. We used latent class growth mixture models to identify heterogeneous mental health trajectories of anxiety, depression, and well-being. Bivariate multinomial logistic regressions were conducted to explore variables associated with the latent classes (subgroups).
Results
The cohort (N = 3416) with a mean age of 64.5 years consisted of 51.7% females. Respiratory cancer was the most common diagnosis (30.4%) with moderate to severe comorbidity burden. Four latent classes with distinct anxiety, depression, and well-being trajectories were identified. Decreasing mental health and well-being trajectories are associated with being female; living in neighborhoods with lower income, greater population density, and higher proportion of foreign-born individuals; and having higher comorbidity burden.
Conclusions
The findings highlight the importance of considering social determinants of mental health and well-being, in addition to symptoms and clinical variables, when providing care for patients undergoing radiation therapy.



Similar content being viewed by others
Data availability
Data sharing agreements prohibit the dataset from being made publicly available. Access may be granted to those who meet pre-specified criteria for confidential access. The statistical analysis code is available from the corresponding author upon request.
References
Niedzwiedz, C. L., Knifton, L., Robb, K. A., Katikireddi, S. V., & Smith, D. J. (2019). Depression and anxiety among people living with and beyond cancer: A growing clinical and research priority. BMC Cancer, 19(1), 943. https://doi.org/10.1186/s12885-019-6181-4
Chen, A. M., Hsu, S., Felix, C., Garst, J., & Yoshizaki, T. (2018). Effect of psychosocial distress on outcome for head and neck cancer patients undergoing radiation. The Laryngoscope, 128(3), 641–645. https://doi.org/10.1002/lary.26751
Mols, F., Husson, O., Roukema, J.-A., & van de Poll-Franse, L. V. (2013). Depressive symptoms are a risk factor for all-cause mortality: Results from a prospective population-based study among 3080 cancer survivors from the PROFILES registry. Journal of Cancer Survivorship, 7(3), 484–492. https://doi.org/10.1007/s11764-013-0286-6
Mausbach, B. T., Decastro, G., Schwab, R. B., Tiamson-Kassab, M., & Irwin, S. A. (2020). Healthcare use and costs in adult cancer patients with anxiety and depression. Depression and Anxiety, 37(9), 908–915. https://doi.org/10.1002/da.23059
Mitchell, A. J., Chan, M., Bhatti, H., Halton, M., Grassi, L., Johansen, C., & Meader, N. (2011). Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. The Lancet Oncology, 12(2), 160–174. https://doi.org/10.1016/S1470-2045(11)70002-X
Rutherford, C., Müller, F., Faiz, N., King, M. T., & White, K. (2020). Patient-reported outcomes and experiences from the perspective of colorectal cancer survivors: Meta-synthesis of qualitative studies. Journal of Patient-Reported Outcomes, 4(1), 27. https://doi.org/10.1186/s41687-020-00195-9
Dinesh, A. A., Helena Pagani Soares Pinto, S., Brunckhorst, O., Dasgupta, P., & Ahmed, K. (2021). Anxiety, depression and urological cancer outcomes: A systematic review. Urologic Oncology: Seminars and Original Investigations. https://doi.org/10.1016/j.urolonc.2021.08.003
Goyal, N. G., Levine, B. J., Van Zee, K. J., Naftalis, E., & Avis, N. E. (2018). Trajectories of quality of life following breast cancer diagnosis. Breast Cancer Research and Treatment, 169(1), 163–173. https://doi.org/10.1007/s10549-018-4677-2
Chambers, S. K., Ng, S. K., Baade, P., Aitken, J. F., Hyde, M. K., Wittert, G., Frydenberg, M., & Dunn, J. (2017). Trajectories of quality of life, life satisfaction, and psychological adjustment after prostate cancer. Psycho-Oncology, 26(10), 1576–1585. https://doi.org/10.1002/pon.4342
Cai, T., Huang, Y., Huang, Q., **a, H., & Yuan, C. (2021). Symptom trajectories in patients with breast cancer: An integrative review. International Journal of Nursing Sciences, 9(1), 120–128. https://doi.org/10.1016/j.ijnss.2021.12.011
Sayani, A. (2019). Health equity in national cancer control plans: An analysis of the Ontario cancer plan. International Journal of Health Policy and Management, 8(9), 550–556. https://doi.org/10.15171/ijhpm.2019.40
Bubis, L. D., Davis, L., Mahar, A., Barbera, L., Li, Q., Moody, L., Karanicolas, P., Sutradhar, R., & Coburn, N. G. (2018). Symptom burden in the first year after cancer diagnosis: An analysis of patient-reported outcomes. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 36(11), 1103–1111. https://doi.org/10.1200/JCO.2017.76.0876
Kuluski, K., Peckham, A., Williams, A., & Upshur, R. (2016). What gets in the way of person-centred care for people with multimorbidity? Lessons from Ontario, Canada. Healthcare Quarterly (Toronto, Ontario), 19, 17–23. https://doi.org/10.12927/hcq.2016.24694
Cancer Care Ontario. (2018, June 28). Ontario Cancer Registry. Cancer Care Ontario. Retrieved November 9, 2021, from https://www.cancercareontario.ca/en/cancer-care-ontario/programs/data-research/ontario-cancer-registry
Barbera, L., Lee, F., & Sutradhar, R. (2019). Use of patient-reported outcomes in regional cancer centres over time: A retrospective study. Canadian Medical Association Open Access Journal, 7(1), E101–E108. https://doi.org/10.9778/cmajo.20180074
Bruera, E., Kuehn, N., Miller, M. J., Selmser, P., & Macmillan, K. (1991). The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. Journal of Palliative Care, 7(2), 6–9.
Watanabe, S. M., Nekolaichuk, C., Beaumont, C., Johnson, L., Myers, J., & Strasser, F. (2011). A multicenter study comparing two numerical versions of the Edmonton Symptom Assessment System in palliative care patients. Journal of Pain and Symptom Management, 41(2), 456–468. https://doi.org/10.1016/j.jpainsymman.2010.04.020
Noel, C. W., Forner, D., Chepeha, D. B., Baran, E., Chan, K. K. W., Parmar, A., Husain, Z., Karam, I., Hallet, J., Coburn, N. G., & Eskander, A. (2021). The Edmonton Symptom Assessment System: A narrative review of a standardized symptom assessment tool in head and neck oncology. Oral Oncology, 123, 105595. https://doi.org/10.1016/j.oraloncology.2021.105595
Chang, V. T., Hwang, S. S., & Feuerman, M. (2000). Validation of the Edmonton Symptom Assessment Scale. Cancer, 88(9), 2164–2171. https://doi.org/10.1002/(sici)1097-0142(20000501)88:9%3c2164::aid-cncr24%3e3.0.co;2-5
Saetra, P., Fossum, M., Svensson, E., & Cohen, M. Z. (2016). Evaluation of two instruments of perceived symptom intensity in palliative care patients in an outpatient clinic. Journal of Clinical Nursing, 25(5–6), 799–810. https://doi.org/10.1111/jocn.13100
Hannon, B., Dyck, M., Pope, A., Swami, N., Banerjee, S., Mak, E., Bryson, J., Rodin, G., Ridley, J., Lo, C., Le, L. W., & Zimmermann, C. (2015). Modified Edmonton Symptom Assessment System including constipation and sleep: Validation in outpatients with cancer. Journal of Pain and Symptom Management, 49(5), 945–952. https://doi.org/10.1016/j.jpainsymman.2014.10.013
Davison, S. N., Jhangri, G. S., & Johnson, J. A. (2006). Longitudinal validation of a modified Edmonton Symptom Assessment System (ESAS) in haemodialysis patients. Nephrology, Dialysis, Transplantation: Official Publication of the European Dialysis and Transplant Association - European Renal Association, 21(11), 3189–3195. https://doi.org/10.1093/ndt/gfl380
Vignaroli, E., Pace, E. A., Willey, J., Palmer, J. L., Zhang, T., & Bruera, E. (2006). The Edmonton Symptom Assessment System as a screening tool for depression and anxiety. Journal of Palliative Medicine, 9(2), 296–303. https://doi.org/10.1089/jpm.2006.9.296
Bagha, S. M., Macedo, A., Jacks, L. M., Lo, C., Zimmermann, C., Rodin, G., & Li, M. (2013). The utility of the Edmonton Symptom Assessment System in screening for anxiety and depression. European Journal of Cancer Care, 22(1), 60–69. https://doi.org/10.1111/j.1365-2354.2012.01369.x
Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383. https://doi.org/10.1016/0021-9681(87)90171-8
World Health Organization. (2020). IACR—International Classification of Diseases for Oncology (ICD-O). Retrieved November 9, 2021, from http://www.iacr.com.fr/index.php?option=com_content&view=category&layout=blog&id=100&Itemid=577
R Core Team. (2019). R: A language and environment for statistical computing (3.6.1.). Vienna. Retrieved from http://www.R-project.org
Muthén, L. K., & Muthén, B. O. (2017). Mplus user’s guide (8th ed.). Los Angeles, CA
Kwon, J.-Y., Sawatzky, R., Baumbusch, J., Lauck, S., & Ratner, P. A. (2021). Growth mixture models: A case example of the longitudinal analysis of patient-reported outcomes data captured by a clinical registry. BMC Medical Research Methodology, 21(1), 79. https://doi.org/10.1186/s12874-021-01276-z
Berlin, K. S., Parra, G. R., & Williams, N. A. (2014). An introduction to latent variable mixture modeling (part 2): Longitudinal latent class growth analysis and growth mixture models. Journal of Pediatric Psychology, 39(2), 188–203. https://doi.org/10.1093/jpepsy/jst085
Burant, C. J. (2016). Latent growth curve models: Tracking changes over time. The International Journal of Aging and Human Development, 82(4), 336–350. https://doi.org/10.1177/0091415016641692
Enders, C. K. (2010). Applied missing data analysis. Guilford Press.
Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. https://doi.org/10.1080/10705510701575396
Asparouhov, T., & Muthén, B. (2014). Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Retrieved from https://www.statmodel.com/examples/webnotes/webnote21.pdf
Elsner, K., Naehrig, D., Halkett, G. K. B., & Dhillon, H. M. (2017). Reduced patient anxiety as a result of radiation therapist-led psychosocial support: A systematic review. Journal of Medical Radiation Sciences, 64(3), 220–231. https://doi.org/10.1002/jmrs.208
Whitaker, K. L., Scott, S. E., & Wardle, J. (2015). Applying symptom appraisal models to understand sociodemographic differences in responses to possible cancer symptoms: A research agenda. British Journal of Cancer, 112(1), S27–S34. https://doi.org/10.1038/bjc.2015.39
Shi, Q., Smith, T. G., Michonski, J. D., Stein, K. D., Kaw, C., & Cleeland, C. S. (2011). Symptom burden in cancer survivors 1 year after diagnosis: A report from the American Cancer Society’s Studies of Cancer Survivors. Cancer, 117(12), 2779–2790. https://doi.org/10.1002/cncr.26146
Agénor, M. (2020). Future directions for incorporating intersectionality into quantitative population health research. American Journal of Public Health, 110(6), 803–806. https://doi.org/10.2105/AJPH.2020.305610
Pinto, A. D., Glattstein-Young, G., Mohamed, A., Bloch, G., Leung, F.-H., & Glazier, R. H. (2016). Building a foundation to reduce health inequities: Routine collection of sociodemographic data in primary care. Journal of the American Board of Family Medicine: JABFM, 29(3), 348–355. https://doi.org/10.3122/jabfm.2016.03.150280
Wagenmakers, E.-J., Sarafoglou, A., & Aczel, B. (2022). One statistical analysis must not rule them all. Nature, 605(7910), 423–425. https://doi.org/10.1038/d41586-022-01332-8
Acknowledgements
This research was undertaken, in part, thanks to funding from the Centre for Health Evaluation and Outcome Sciences at Providence Health Care (“http://www.cheos.ubc.ca”) and the Canada Research Chairs program in support of RS’s Chair in Person-Centered Outcomes. The funding bodies had no role in the design, analysis, and interpretation of the data, and in writing the manuscript.
Funding
The study was supported by the Centre for Health Evaluation and Outcome Sciences at Providence Health Care and the Canada Research Chairs program in support of Richard Sawatzky’s Chair in Person-Centred Outcomes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the institutional ethics review board [Health Research Ethics Board of the Trinity Western University and the University of British Columbia-Providence Health Care (H18-01947)].
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwon, JY., Kopec, J., Sutherland, J.M. et al. Patient-reported mental health and well-being trajectories in oncology patients during radiation therapy: an exploratory retrospective cohort analysis using the Ontario Cancer Registry. Qual Life Res 32, 2899–2909 (2023). https://doi.org/10.1007/s11136-023-03430-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03430-0