Abstract
Purpose
Although numerous studies have established advanced patient age as a risk factor for poor outcomes following intracranial meningioma resection, large-scale evaluation of frailty for preoperative risk assessment has yet to be examined.
Methods
Weighted discharge data from the National Inpatient Sample were queried for adult patients undergoing benign intracranial meningioma resection from 2015 to 2018. Complex samples multivariable logistic regression models and receiver operating characteristic curve analysis were performed to evaluate adjusted associations and discrimination of frailty, quantified using the 11-factor modified frailty index (mFI), for clinical endpoints.
Results
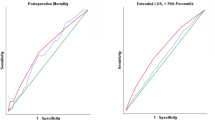
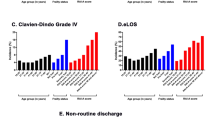
Among 20,250 patients identified (mean age 60.6 years), 35.4% (n = 7170) were robust (mFI = 0), 34.5% (n = 6985) pre-frail (mFI = 1), 20.1% (n = 4075) frail (mFI = 2), and 10.0% (n = 2020) severely frail (mFI ≥ 3). On univariable analysis, these sub-cohorts stratified by increasing frailty were significantly associated with the development of Clavien–Dindo grade IV (life-threatening) complications (inclusive of those resulting in mortality) (1.3% vs. 3.1% vs. 6.5% vs. 9.4%, p < 0.001) and extended length of stay (eLOS) (15.4% vs. 22.5% vs. 29.3% vs. 37.4%, p < 0.001). Following multivariable analysis, increasing frailty (aOR 1.40, 95% CI 1.17, 1.68, p < 0.001) and age (aOR 1.20, 95% CI 1.05, 1.38, p = 0.009) were both independently associated with development of life-threatening complications or mortality, whereas increasing frailty (aOR 1.20, 95% CI 1.10, 1.32, p < 0.001), but not age, was associated with eLOS. Frailty (by mFI-11) achieved superior discrimination in comparison to age for both endpoints (AUC 0.69 and 0.61, respectively).
Conclusion
Frailty may be more accurate than advanced patient age alone for prognostication of adverse events and outcomes following intracranial meningioma resection.

Similar content being viewed by others
Data availability
All data utilized in this analysis are available upon reasonable request of the corresponding author following completion of necessary onboarding and verification procedures specified by the Healthcare Cost and Utilization Project.
Code availability
Billing codes utilized in this analysis are available upon reasonable request of the corresponding author. Those used for identification of primary clinical endpoints are defined in the manuscript supplement.
References
Marosi C, Hassler M, Roessler K et al (2008) Meningioma. Crit Rev Oncol Hematol 67(2):153–171
Poon MT, Fung LH, Pu JK, Leung GK (2013) Outcome comparison between younger and older patients undergoing intracranial meningioma resections. J Neurooncol 114(2):219–227
Ekşi M, Canbolat Ç, Akbaş A et al (2019) Elderly patients with intracranial meningioma: surgical considerations in 228 patients with a comprehensive analysis of the literature. World Neurosurg 132:e350–e365
Rijnen SJM, Meskal I, Bakker M et al (2019) Cognitive outcomes in meningioma patients undergoing surgery: individual changes over time and predictors of late cognitive functioning. Neuro Oncol 21(7):911–922
Runner RP, Bellamy JL, Vu CCL, Erens GA, Schenker ML, Guild GN 3rd (2017) Modified frailty index is an effective risk assessment tool in primary total knee arthroplasty. J Arthroplasty 32:S177–S182
Mogal H, Vermilion SA, Dodson R et al (2017) Modified frailty index predicts morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol 24(6):1714–1721
Karam J, Tsiouris A, Shepard A, Velanovich V, Rubinfeld I (2013) Simplified frailty index to predict adverse outcomes and mortality in vascular surgery patients. Ann Vasc Surg 27(7):904–908
Fried LP, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A: Biol Sci Med Sci 56(3):M146-156
Bonney PA, Chartrain AG, Briggs RG et al (2021) Frailty is associated with in-hospital morbidity and nonroutine disposition in brain tumor patients undergoing craniotomy. World Neurosurg 146:e1045–e1053
Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183(1):104–110
Rockwood K, Song X, MacKnight C et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495
Dicpinigaitis AJ, Kalakoti P, Schmidt M et al (2021) Associations of baseline frailty status and age with outcomes in patients undergoing vestibular schwannoma resection. JAMA Otolaryngol Head Neck Surg 147:608
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Adams P, Ghanem T, Stachler R, Hall F, Velanovich V, Rubinfeld I (2013) Frailty as a predictor of morbidity and mortality in inpatient head and neck surgery. JAMA Otolaryngol Head Neck Surg 139(8):783–789
Abt NB, Richmon JD, Koch WM, Eisele DW, Agrawal N (2016) Assessment of the predictive value of the modified frailty index for Clavien–Dindo grade IV critical care complications in major head and neck cancer operations. JAMA Otolaryngol Head Neck Surg 142(7):658–664
Hall EC, Boyarsky BJ, Deshpande NA et al (2014) Perioperative complications after live-donor hepatectomy. JAMA Surg 149(3):288–291
Meyer CP, Sun M, Karam JA et al (2017) Complications after metastasectomy for renal cell carcinoma-a population-based assessment. Eur Urol 72(2):171–174
Khera R, Angraal S, Couch T et al (2017) Adherence to methodological standards in research using the national inpatient sample. JAMA 318(20):2011–2018
Sastry RA, Pertsch NJ, Tang O, Shao B, Toms SA, Weil RJ (2020) Frailty and outcomes after craniotomy for brain tumor. J Clin Neurosci 81:95–100
Shahrestani S, Lehrich BM, Tafreshi AR et al (2020) The role of frailty in geriatric cranial neurosurgery for primary central nervous system neoplasms. Neurosurg Focus 49(4):E15
Theriault BC, Pazniokas J, Adkoli AS et al (2020) Frailty predicts worse outcomes after intracranial meningioma surgery irrespective of existing prognostic factors. Neurosurg Focus 49(4):E16
Jimenez AE, Khalafallah AM, Huq S et al (2020) Predictors of nonroutine discharge disposition among patients with parasagittal/parafalcine meningioma. World Neurosurg 142:e344–e349
McIntyre MK, Gandhi C, Long A et al (2019) Age predicts outcomes better than frailty following aneurysmal subarachnoid hemorrhage: a retrospective cohort analysis. Clin Neurol Neurosurg 187:105558
Author information
Authors and Affiliations
Contributions
CAB and AJD conceived of the project and methodology. CAB, SFK, BCT, SFK, and SH composed the manuscript. AJD and SFK queried the database and completed statistical analysis. All authors interpreted the data and provided input on analysis and manuscript revision. All authors read and approved the final manuscript. CAB, FAM, WTC, MHS, and CDG provided supervision for the project.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Given the public accessibility and de-identified nature of the information in this database, this study did not meet the requirements for institutional review board approval. For the same reason, patient consent was neither sought nor required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dicpinigaitis, A.J., Kazim, S.F., Schmidt, M.H. et al. Association of baseline frailty status and age with postoperative morbidity and mortality following intracranial meningioma resection. J Neurooncol 155, 45–52 (2021). https://doi.org/10.1007/s11060-021-03841-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03841-4