Abstract
Background
To investigate the effect of plasma-derived extracellular vesicles (EVs) or conventional medium in fertilization and early embryo development rate in mice.
Methods and results
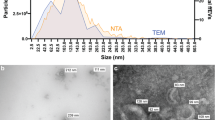
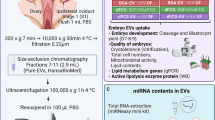
MII oocytes (matured in vivo or in vitro conditions) were obtained from female mice. The extracellular vesicles were isolated by ultracentrifugation of plasma and were analyzed and measured for size and morphology by dynamic light scattering (DLS) and transmission electron microscopy (TEM). By western blotting analysis, the EVs proteins markers such as CD82 protein and heat shock protein 90 (HSP90) were investigated. Incorporating DiI-labeled EVs within the oocyte cytoplasm was visible at 23 h in oocyte cytoplasm. Also, the effective proteins in the early reproductive process were determined in isolated EVs by western blotting. These EVs had a positive effect on the fertilization rate (P < 0.05). The early embryo development (8 cell, morula and blastocyst stages) was higher in groups supplemented with EVs (P < 0.01).
Conclusion
Our findings showed that supplementing in vitro maturation media with EVs derived- plasma was beneficial for mice’s embryo development.









Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Wolf P (1967) The nature and significance of platelet products in human plasma. Br J Haematol 13(3):269–288
Foster B, Balassa T, Benen T, Dominovic M, Elmadjian G, Florova V et al (2016) Extracellular vesicles in blood, milk and body fluids of the female and male urogenital tract and with special regard to reproduction. Crit Rev Clini Lab Sci 53(6):379–395
Gutjahr C, Parniske M (2013) Cell and developmental biology of arbuscular mycorrhiza symbiosis. Ann Rev cell Dev Biol 29:593–617
Lötvall J, Hill AF, Hochberg F, Buzás EI, Di Vizio D, Gardiner C et al (2014) Minimal experimental requirements for definition of extracellular vesicles and their functions: a position statement from the Int Soc for Extracell Vesicles. Taylor & Francis, p 26913
Kalra H, Drummen GP, Mathivanan S (2016) Focus on extracellular vesicles: introducing the next small big thing. Int J Mol Sci 17(2):170
Sitar S, Kejžar A, Pahovnik D, Kogej K, Tušek-Žnidarič M, Lenassi M et al (2015) Size characterization and quantification of exosomes by asymmetrical-flow field-flow fractionation. Anal Chem 87(18):9225–9233
Javadi M, Rad JS, Farashah MSG, Roshangar LJRS (2021) An insight on the role of altered function and expression of exosomes and microRNAs in female Reproductive desiease. Reprod Sci 6:1–13
Gholami Farashah MS, Javadi M, Mohammadi A, Soleimani Rad J, Shakouri SK, Roshangar LJMBR (2022) Bone marrow mesenchymal stem cell’s exosomes as key nanoparticles in osteogenesis and bone regeneration: Specific capacity based on cell type 49(12):12203-18
Rizos D, Clemente M, Bermejo-Alvarez P, de La Fuente J, Lonergan P, Gutiérrez‐Adán A (2008) Consequences of in vitro culture conditions on embryo development and quality. Reprod Domest Anim 43:44–50
Lonergan P, Fair TJT (2008) In vitro-produced bovine embryos—dealing with the warts. Thriogenol 69(1):17–22
Krisher RL (2013) In vivo and in vitro environmental effects on mammalian oocyte quality. Annu Rev Anim Bio Sci 1(1):393–417
Demyda S, Genero E (2011) Developmental competence of in vivo and in vitro matured oocytes: a review. Biotech Mol BiolRev 6(7):155–165
Hackney AC (2020) Hypogonadism in exercising males: dysfunction or adaptive-regulatory adjustment? Front in Endocrin 11
Lange-Consiglio A, Perrini C, Albini G, Modina S, Lodde V, Orsini E et al (2017) Oviductal microvesicles and their effect on in vitro maturation of canine oocytes. Reprod 154(2):167–180
DANG-NGUYEN TQ, Somfai T, Haraguchi S, Kikuchi K, Tajima A, Kanai Y et al (2011) In vitro production of porcine embryos: current status, future perspectives and alternative applications. Anim Sci J 82(3):374–382
Gervasi MG, Soler AJ, González-Fernández L, Alves MG, Oliveira PF, Martín-Hidalgo D (2020) Extracellular vesicles, the road toward the improvement of ART outcomes. Anim 10(11):2171
Avilés M, Coy P, Rizos D (2015) The oviduct: a key organ for the success of early reproductive events. Anim Front 5(1):25–31
Tannetta D, Dragovic R, Alyahyaei Z, Southcombe J (2014) Extracellular vesicles and reproduction–promotion of successful pregnancy. Cell Mol Immun 11(6):548–563
Alminana C, Tsikis G, Labas V, Uzbekov R, da Silveira JC, Bauersachs S et al (2018) Deciphering the oviductal extracellular vesicles content across the estrous cycle: implications for the gametes-oviduct interactions and the environment of the potential embryo. BMC Genom 19(1):1–27
Javadi M, Rad JS, Pashaiasl M, Farashah MSG, Roshangar L (2022) The effects of plasma-derived extracellular vesicles on cumulus expansion and oocyte maturation in mice. Reprod Biol 22(1):100593
Machtinger R, Laurent LC, Baccarelli AA (2016) Extracellular vesicles: roles in gamete maturation, fertilization and embryo implantation. Hum Reprod Update 22(2):182–193
Eitan E, Green J, Bodogai M, Mode NA, Bæk R, Jørgensen MM et al (2017) Age-related changes in plasma extracellular vesicle characteristics and internalization by leukocytes. Sci Rep 7(1):1–14
Colombo M, Raposo G, Théry C (2014) Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Ann Rev cell Dev Biol 30:255–289
Vicencio JM, Yellon DM, Sivaraman V, Das D, Boi-Doku C, Arjun S et al (2015) Plasma exosomes protect the myocardium from ischemia-reperfusion injury. J Am Coll Cardio 65(15):1525–1536
Farashah MSG, Javadi M, Rad JS, Shakouri SK, Dastmalchi SAS, Roshangar SNL (2023) Article Title: 17β-Estradiol-loaded exosomes for targeted drug delivery in osteoporosis: a comparative study of two loading methods running title: drug delivery with 17β-Estradiol-loaded exosomes. Ad Pharm Bullet 13:736
Noferesti SS, Sohel M, Hasan M, Hoelker M, Salilew-Wondim D, Tholen E et al (2015) Controlled ovarian hyperstimulation induced changes in the expression of circulatory miRNA in bovine follicular fluid and blood plasma. J Ovarian Res 8(1):1–16
Otani K, Yokoya M, Kodama T, Hori K, Matsumoto K, Okada M et al (2018) Plasma exosomes regulate systemic blood pressure in rats. Biochem Biophys Res Commun 503(2):776–783
Montecalvo A, Larregina AT, Shufesky WJ, Beer Stolz D, Sullivan ML, Karlsson JM et al (2012) Mechanism of transfer of functional microRNAs between mouse dendritic cells via exosomes. Blood J Am Soc Hematol 119(3):756–766
Yang PC (2018) Induced pluripotent stem cell (iPSC)–derived exosomes for precision medicine in heart failure. Circ Res 122(5):661–663
Cebrian-Serrano A, Salvador I, García‐Roselló E, Pericuesta E, Pérez‐Cerezales S, Gutierrez‐Adán A et al (2013) Effect of the bovine oviductal fluid on in vitro fertilization, development and gene expression of in vitro‐produced bovine blastocysts. Reprod Dom Anim 48(2):331–338
de Ferraz AMM, Carothers M, Dahal A, Noonan R, Songsasen M N (2019) Oviductal extracellular vesicles interact with the spermatozoon’s head and mid-piece and improves its motility and fertilizing ability in the domestic cat. Sci Rep 9(1):1–12
Alcântara-Neto A, Fernandez-Rufete M, Corbin E, Tsikis G, Uzbekov R, Garanina A et al (2020) Oviduct fluid extracellular vesicles regulate polyspermy during porcine in vitro fertilisation. Reprod Fertil Dev 32(4):409–418
Qu P, Zhao Y, Wang R, Zhang Y, Li L, Fan J et al (2019) Extracellular vesicles derived from donor oviduct fluid improved birth rates after embryo transfer in mice. Reprod Fertil Dev 31(2):324–332
Teijeiro JM, Munuce MJ, Caille AM, Zumoffen C, Marini PE (2017) Use of annexin V based sperm selection in assisted reproduction
Toshimori K (2011) Dynamics of the mammalian sperm membrane modification leading to fertilization: a cytological study. J Elec Micros 60(suppl1):S31–S42
Moein-Vaziri N, Phillips I, Smith S, Alminana C, Maside C, Gil MA et al (2014) Heat-shock protein A8 restores sperm membrane integrity by increasing plasma membrane fluidity. Reprod 147(5):719–732
Greenstein D (2005) Control of oocyte meiotic maturation and fertilization. The Online Rev of Elegans Biol, WormBook
Combelles CM, Fissore RA, Albertini DF, Racowsky C (2005) In vitro maturation of human oocytes and cumulus cells using a co-culture three-dimensional collagen gel system. Hum Reprod 20(5):1349–1358
Albuz F, Sasseville M, Lane M, Armstrong D, Thompson J, Gilchrist R (2010) Simulated physiological oocyte maturation (SPOM): a novel in vitro maturation system that substantially improves embryo yield and pregnancy outcomes. Hum Reprod 25(12):2999–3011
Zhang H-L, Xu Y, Ju J-Q, Pan Z-N, Liu J-C, Sun S-C (2021) Increased environment-related metabolism and genetic expression in the in vitro matured mouse oocytes by Transcriptome Analysis. Front Cell Dev Biol 9:171
Vanhoutte L, De Sutter P, Van der Elst J, Dhont M (2005) Clinical benefit of metaphase I oocytes. Reprod Biol Endocrin 3(1):1–6
Jones GM, Cram DS, Song B, Magli MC, Gianaroli L, Lacham-Kaplan O et al (2008) Gene expression profiling of human oocytes following in vivo or in vitro maturation. Hum Reprod 23(5):1138–1144
Pioltine EM, Machado MF, da Silveira JC, Fontes PK, Botigelli RC, Quaglio AEV et al (2020) Can extracellular vesicles from bovine ovarian follicular fluid modulate the in-vitro oocyte meiosis progression similarly to the CNP-NPR2 system? Theriogenol 157:210–217
Funding
This study was supported by grants from the Stem Cell Research Center, Tabriz University of Medical Sciences, Tabriz, Iran (Grant Number: 63134).
Author information
Authors and Affiliations
Contributions
Maryam Javadi and Leila Roshangar designed this study. Maryam Javadi and Mohammad Sadegh Gholami Farashah wrote the main manuscript text. Maryam Javadi prepared figures and analyzed the collected data. Jafar Soleimani Rad and Leila Roshangar edited the main text. All authors reviewed the manuscript and replied to revise.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in present study were approved by Tabriz University of Medical Sciences’ Committee on Animal Experimentation, ethical approval number: IR.TBZMED.VCR.REC.1398.289.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Javadi, M., Gholami Farashah, M., Roshangar, L. et al. Plasma-derived extracellular vesicles improve mice embryo development. Mol Biol Rep 51, 621 (2024). https://doi.org/10.1007/s11033-024-09500-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09500-x