Abstract
Background
Oxidative stress has a critical effect on both persistent pain states and periodontal disease. Voltage-gated sodium NaV1.7 (SCN9A), and transient receptor potential ankyrin 1 (TRPA1) are pain genes. The goal of this study was to investigate oxidative stress markers, periodontal status, SCN9A, and TRPA1 channel expression in periodontal tissues of rats with paclitaxel-induced neuropathic pain-like behavior (NPLB).
Methods and results
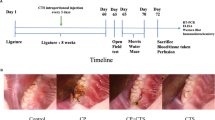
Totally 16 male Sprague Dawley rats were used: control (n = 8) and paclitaxel-induced pain (PTX) (n = 8). The alveolar bone loss and 8-hydroxy-2-deoxyguanosine (8-OHdG) levels were analyzed histometrically and immunohistochemically. Gingival superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx) activities (spectrophotometric assay) were measured. The relative TRPA1 and SCN9A genes expression levels were evaluated using quantitative real-time PCR (qPCR) in the tissues of gingiva and brain. The PTX group had significantly higher alveolar bone loss and 8-OHdG compared to the control. The PTX group had significantly lower gingival SOD, GPx and CAT activity than the control groups. The PTX group had significantly higher relative gene expression of SCN9A (p = 0.0002) and TRPA1 (p = 0.0002) than the control in gingival tissues. Increased nociceptive susceptibility may affect the increase in oxidative stress and periodontal destruction.
Conclusions
Chronic pain conditions may increase TRPA1 and SCN9A gene expression in the periodontium. The data of the current study may help develop novel approaches both to maintain periodontal health and alleviate pain in patients suffering from orofacial pain.




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- SCN9A:
-
Voltage-gated sodium channels, NaV1.7
- TRPA1:
-
Transient receptor potential ankyrin 1 channel
- 8-OHdG:
-
8-hydroxy-2-deoxyguanosine
- SOD:
-
Superoxide dismutase
- CAT:
-
Catalase
- GPx:
-
Glutathione peroxidase
- ROS:
-
Reactive oxygen
- RNS:
-
Nitrogen species
- NIH:
-
National Institute of Health
- PTX group:
-
Paclitaxel induced group
- i.p:
-
Intraperitoneal
- CEJ:
-
Cementoenamel junction
- qPCR:
-
quantitative real-time PCR
References
Kaye AD, Jones MR, Kaye AM et al (2017) Prescription opioid abuse in Chronic Pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician 20:S93–S109
Latremoliere A, Woolf CJ (2009) Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain 10:895–926. https://doi.org/10.1016/j.jpain.2009.06.012
Fornasari D (2012) Pain mechanisms in patients with chronic pain. Clin Drug Investig 32(Suppl 1):45–52. https://doi.org/10.2165/11630070-000000000-00000
Treede RD, Rief W, Barke A et al (2019) Chronic pain as a symptom or a disease: the IASP classification of Chronic Pain for the International classification of Diseases (ICD-11). Pain 160:19–27. https://doi.org/10.1097/j.pain.0000000000001384
Harper DE, Schrepf A, Clauw DJ (2016) Pain Mechanisms and Centralized Pain in Temporomandibular Disorders. J Dent Res 95:1102–1108. https://doi.org/10.1177/0022034516657070
Mannerak MA, Lashkarivand A, Eide PK (2021) Trigeminal neuralgia and genetics: a systematic review. Mol Pain 17:17448069211016139. https://doi.org/10.1177/17448069211016139
Shakouri SK, Dolatkhah N, Omidbakhsh S, Pishgahi A, Hashemian M (2020) Serum inflammatory and oxidative stress biomarkers levels are associated with pain intensity, pressure pain threshold and quality of life in myofascial pain syndrome. BMC Res Notes 13:510. https://doi.org/10.1186/s13104-020-05352-3
Salvemini D, Little JW, Doyle T, Neumann WL (2011) Roles of reactive oxygen and nitrogen species in pain. Free Radic Biol Med 51:951–966. https://doi.org/10.1016/j.freeradbiomed.2011.01.026
Park ES, Gao X, Chung JM, Chung K (2006) Levels of mitochondrial reactive oxygen species increase in rat neuropathic spinal dorsal horn neurons. Neurosci Lett 391:108–111. https://doi.org/10.1016/j.neulet.2005.08.055
Herzberg D, Strobel P, Chihuailaf R et al (2019) Spinal reactive oxygen species and oxidative damage Mediate Chronic Pain in Lame dairy cows. Anim (Basel) 9. https://doi.org/10.3390/ani9090693
Babior BM (2000) Phagocytes and oxidative stress. Am J Med 109:33–44. https://doi.org/10.1016/s0002-9343(00)00481-2
Karaman M, Toraman E, Sulukan E et al (2023) Fluoride exposure causes behavioral, molecular and physiological changes in adult zebrafish (Danio rerio) and their offspring. Environ Toxicol Pharmacol 97:104044. https://doi.org/10.1016/j.etap.2022.104044
Chapple IL, Matthews JB (2007) The role of reactive oxygen and antioxidant species in periodontal tissue destruction. Periodontol 2000 43:160–232. https://doi.org/10.1111/j.1600-0757.2006.00178.x
Na HJ, Kim OS, Park BJ (2006) Expression of Superoxide dismutase isoforms in inflamed gingiva. J Korean Acad Periodontol 36:97–112
Akalin FA, Toklu E, Renda N (2005) Analysis of superoxide dismutase activity levels in gingiva and gingival crevicular fluid in patients with chronic periodontitis and periodontally healthy controls. J Clin Periodontol 32:238–243. https://doi.org/10.1111/j.1600-051X.2005.00669.x
Sczepanik FSC, Grossi ML, Casati M et al (2020) Periodontitis is an inflammatory disease of oxidative stress: we should treat it that way. Periodontol 2000 84:45–68. https://doi.org/10.1111/prd.12342
Garrett IR, Boyce BF, Oreffo RO, Bonewald L, Poser J, Mundy GR (1990) Oxygen-derived free radicals stimulate osteoclastic bone resorption in rodent bone in vitro and in vivo. J Clin Invest 85:632–639. https://doi.org/10.1172/JCI114485
Koori K, Maeda H, Fujii S et al (2014) The roles of calcium-sensing receptor and calcium channel in osteogenic differentiation of undifferentiated periodontal ligament cells. Cell Tissue Res 357:707–718. https://doi.org/10.1007/s00441-014-1918-5
Rifkin BR, Vernillo AT, Golub LM (1993) Blocking Periodontal Disease Progression by inhibiting tissue-destructive enzymes: a potential therapeutic role for tetracyclines and their chemically-modified analogs. J Periodontol 64:819–827. https://doi.org/10.1902/jop.1993.64.8s.819
Souza Monteiro de Araujo D, Nassini R, Geppetti P, De Logu F (2020) TRPA1 as a therapeutic target for nociceptive pain. Expert Opin Ther Targets 24:997–1008. https://doi.org/10.1080/14728222.2020.1815191
Kobayashi K, Fukuoka T, Obata K et al (2005) Distinct expression of TRPM8, TRPA1, and TRPV1 mRNAs in rat primary afferent neurons with adelta/c-fibers and colocalization with trk receptors. J Comp Neurol 493:596–606. https://doi.org/10.1002/cne.20794
Trevisani M, Siemens J, Materazzi S et al (2007) 4-Hydroxynonenal, an endogenous aldehyde, causes pain and neurogenic inflammation through activation of the irritant receptor TRPA1. Proc Natl Acad Sci U S A 104:13519–13524. https://doi.org/10.1073/pnas.0705923104
Sawada Y, Hosokawa H, Matsumura K, Kobayashi S (2008) Activation of transient receptor potential ankyrin 1 by hydrogen peroxide. Eur J Neurosci 27:1131–1142. https://doi.org/10.1111/j.1460-9568.2008.06093.x
Ito M, Ono K, Hitomi S et al (2017) Prostanoid-dependent spontaneous pain and PAR2-dependent mechanical allodynia following oral mucosal trauma: involvement of TRPV1, TRPA1 and TRPV4. Mol Pain 13:1744806917704138. https://doi.org/10.1177/1744806917704138
Nyman E, Franzen B, Nolting A et al (2013) In vitro pharmacological characterization of a novel TRPA1 antagonist and proof of mechanism in a human dental pulp model. J Pain Res 6:59–70. https://doi.org/10.2147/JPR.S37567
Pusztai L, Mendoza TR, Reuben JM et al (2004) Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine 25:94–102. https://doi.org/10.1016/j.cyto.2003.10.004
Fazekas A, Vindisch K, Posch E, Gyorfi A (1990) Experimentally-induced neurogenic inflammation in the rat oral mucosa. J Periodontal Res 25:276–282. https://doi.org/10.1111/j.1600-0765.1990.tb00916.x
Son DB, Choi W, Kim M et al (2021) Decursin alleviates mechanical Allodynia in a Paclitaxel-Induced Neuropathic Pain Mouse Model. Cells 10. https://doi.org/10.3390/cells10030547
Yam MF, Loh YC, Oo CW, Basir R (2020) Overview of neurological mechanism of Pain Profile used for Animal Pain-Like behavioral study with proposed analgesic pathways. Int J Mol Sci 21. https://doi.org/10.3390/ijms21124355
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254. https://doi.org/10.1006/abio.1976.9999
Sun Y, Oberley LW, Li Y (1988) A simple method for clinical assay of superoxide dismutase. Clin Chem 34:497–500
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126. https://doi.org/10.1016/s0076-6879(84)05016-3
Beutler E (1975) Red cell metabolism. A manual of biochemical methods: 11–12
Kocpinar EF, Gonul Baltaci N, Ceylan H, Kalin SN, Erdogan O, Budak H (2020) Effect of a prolonged Dietary Iron Intake on the Gene expression and activity of the testicular antioxidant defense system in rats. Biol Trace Elem Res 195:135–141. https://doi.org/10.1007/s12011-019-01817-0
Carrasco C, Naziroglu M, Rodriguez AB, Pariente JA (2018) Neuropathic Pain: delving into the oxidative origin and the possible implication of transient receptor potential channels. Front Physiol 9:95. https://doi.org/10.3389/fphys.2018.00095
Zhao M, Zhang X, Tao X et al (2021) Sirt2 in the spinal cord regulates Chronic Neuropathic Pain through Nrf2-Mediated oxidative stress pathway in rats. Front Pharmacol 12:646477. https://doi.org/10.3389/fphar.2021.646477
Komirishetty P, Areti A, Yerra VG et al (2016) PARP inhibition attenuates neuroinflammation and oxidative stress in chronic constriction injury induced peripheral neuropathy. Life Sci 150:50–60. https://doi.org/10.1016/j.lfs.2016.02.085
Guedes RP, Dal Bosco L, Araujo AS, Bello-Klein A, Ribeiro MF, Partata WA (2009) Sciatic nerve transection increases gluthatione antioxidant system activity and neuronal nitric oxide synthase expression in the spinal cord. Brain Res Bull 80:422–427. https://doi.org/10.1016/j.brainresbull.2009.08.007
Kerckhove N, Collin A, Conde S, Chaleteix C, Pezet D, Balayssac D (2017) Long-Term Effects, pathophysiological mechanisms, and risk factors of Chemotherapy-Induced Peripheral Neuropathies: a Comprehensive Literature Review. Front Pharmacol 8:86. https://doi.org/10.3389/fphar.2017.00086
Ogawa N, Kurokawa T, Mori Y (2016) Sensing of redox status by TRP channels. Cell Calcium 60:115–122. https://doi.org/10.1016/j.ceca.2016.02.009
Materazzi S, Fusi C, Benemei S et al (2012) TRPA1 and TRPV4 mediate paclitaxel-induced peripheral neuropathy in mice via a glutathione-sensitive mechanism. Pflugers Arch 463:561–569. https://doi.org/10.1007/s00424-011-1071-x
Markowitz K (2010) Pretty painful: why does tooth bleaching hurt? Med Hypotheses 74:835–840. https://doi.org/10.1016/j.mehy.2009.11.044
Kim YS, Jung HK, Kwon TK et al (2012) Expression of transient receptor potential ankyrin 1 in human dental pulp. J Endod 38:1087–1092. https://doi.org/10.1016/j.joen.2012.04.024
Siqueira SR, Alves B, Malpartida HM, Teixeira MJ, Siqueira JT (2009) Abnormal expression of voltage-gated sodium channels Nav1.7, Nav1.3 and Nav1.8 in trigeminal neuralgia. Neuroscience 164:573–577. https://doi.org/10.1016/j.neuroscience.2009.08.037
Costa GMF, Rocha LPC, Siqueira S, Moreira PR, Almeida-Leite CM (2019) No association of polymorphisms in Nav1.7 or nerve growth factor receptor genes with trigeminal Neuralgia. Pain Med 20:1362–1369. https://doi.org/10.1093/pm/pny191
Korczeniewska OA, Husain S, Khan J, Eliav E, Soteropoulos P, Benoliel R (2018) Differential gene expression in trigeminal ganglia of male and female rats following chronic constriction of the infraorbital nerve. Eur J Pain 22:875–888. https://doi.org/10.1002/ejp.1174
Hong SS, Morrow TJ, Paulson PE, Isom LL, Wiley JW (2004) Early painful diabetic neuropathy is associated with differential changes in tetrodotoxin-sensitive and -resistant sodium channels in dorsal root ganglion neurons in the rat. J Biol Chem 279:29341–29350. https://doi.org/10.1074/jbc.M404167200
Chattopadhyay M, Mata M, Fink DJ (2008) Continuous delta-opioid receptor activation reduces neuronal voltage-gated sodium channel (na(V)1.7) levels through activation of protein kinase C in painful diabetic neuropathy. J Neurosci 28:6652–6658. https://doi.org/10.1523/Jneurosci.5530-07.2008
Huang YL, Zang Y, Zhou LJ, Gui WS, Liu XG, Zhong Y (2014) The role of TNF-alpha/NF-kappa B pathway on the up-regulation of voltage-gated sodium channel Nav1.7 in DRG neurons of rats with diabetic neuropathy. Neurochem Int 75:112–119. https://doi.org/10.1016/j.neuint.2014.05.012
Toraman E, Bayram C, Sezen S, Ozkaraca M, Hacimuftuoglu A, Budak H (2023) Parthenolide as a potential analgesic in the treatment of paclitaxel-induced neuropathic pain: the rat modeling. https://doi.org/10.1007/s00210-023-02568-5. Naunyn-Schmiedebergs Archives of Pharmacology
Zhang H, Dougherty PM (2014) Enhanced excitability of primary sensory neurons and altered gene expression of neuronal ion channels in dorsal root ganglion in paclitaxel-induced peripheral neuropathy. Anesthesiology 120:1463–1475. https://doi.org/10.1097/ALN.0000000000000176
Li Y, North RY, Rhines LD et al (2018) DRG voltage-gated Sodium Channel 1.7 is upregulated in Paclitaxel-Induced Neuropathy in rats and in humans with Neuropathic Pain. J Neurosci 38:1124–1136. https://doi.org/10.1523/Jneurosci.0899-17.2017
Huang Y, Zang Y, Zhou L, Gui W, Liu X, Zhong Y (2014) The role of TNF-alpha/NF-kappa B pathway on the up-regulation of voltage-gated sodium channel Nav1.7 in DRG neurons of rats with diabetic neuropathy. Neurochem Int 75:112–119. https://doi.org/10.1016/j.neuint.2014.05.012
Zhang P, Gan YH (2017) Prostaglandin E2 upregulated trigeminal Ganglionic Sodium Channel 1.7 Involving Temporomandibular Joint Inflammatory Pain in rats. Inflammation 40:1102–1109. https://doi.org/10.1007/s10753-017-0552-2
Borges I, Moreira EAM, Wilhem D, de Oliveira TB, da Silva MBS, Froede AS (2007) Proinflammatory and oxidative stress markers in patients with periodontal disease. Mediators of Inflammation 2007https://doi.org/Artn 4579410.1155/2007/45794
Ying SQ, Tan MM, Feng G et al (2020) Low-intensity pulsed Ultrasound regulates alveolar bone homeostasis in experimental Periodontitis by diminishing oxidative stress. Theranostics 10:9789–9807. https://doi.org/10.7150/thno.42508
Carvalho JS, Ramadan D, de Paiva Goncalves V et al (2021) Impact of citrus flavonoid supplementation on inflammation in lipopolysaccharide-induced periodontal disease in mice. Food Funct 12:5007–5017. https://doi.org/10.1039/d0fo03338c
Akalin FA, Isiksal E, Baltacioglu E, Renda N, Karabulut E (2008) Superoxide dismutase activity in gingiva in type-2 diabetes mellitus patients with chronic periodontitis. Arch Oral Biol 53:44–52. https://doi.org/10.1016/j.archoralbio.2007.07.009
Toraman A, Arabaci T, Aytekin Z, Albayrak M, Bayir Y (2020) Effects of vitamin C local application on ligature-induced periodontitis in diabetic rats. J Appl Oral Sci 28:e20200444. https://doi.org/10.1590/1678-7757-2020-0444
DeLeo JA, Rutkowski MD (2000) Gender differences in rat neuropathic pain sensitivity is dependent on strain. Neurosci Lett 282:197–199. https://doi.org/10.1016/s0304-3940(00)00880-6
Dominguez CA, Strom M, Gao T et al (2012) Genetic and sex influence on neuropathic pain-like behaviour after spinal cord injury in the rat. Eur J Pain 16:1368–1377. https://doi.org/10.1002/j.1532-2149.2012.00144.x
Acknowledgements
We thank all the people who helped during performing all the experiments.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Ayşe Toraman: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Data Curation, Writing - Original Draft, Writing - Review & Editing, Visualization, Final approval of the version to be submittedEmine Toraman: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing - Original Draft, Visualization, Final approval of the version to be submittedMustafa Özkaraca: Methodology, Formal analysis, Investigation, Writing - Original Draft, Visualization, Final approval of the version to be submittedHarun Budak: Conceptualization, Methodology, Writing - Original Draft, Visualization, Final approval of the version to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was performed according to the University of Atatürk University Animal Experiments Local Ethics Committee protocol (HADYEK protocol number 2019 − 193). All experiments were consistent with the National Institute of Health (NIH) Guide for the care and use of animals.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Toraman, A., Toraman, E., Özkaraca, M. et al. Evaluated periodontal tissues and oxidative stress in rats with neuropathic pain-like behavior. Mol Biol Rep 50, 9315–9322 (2023). https://doi.org/10.1007/s11033-023-08829-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08829-z