Abstract
Thalassemia is one of the most common monogenic hereditary disorders. Despite noticeable advances made in prevention strategies, it is still highly prevalent in the Iranian population. A key approach to management and early diagnosis of the disease is through revealing the regions with high prevalence and determining common genetic and phenotypic diversity. In the current study Hemoglobin H (HbH) disease patients were analyzed as the most common form of thalassemia intermedia in Iran. A total of 80 patients suspected of being thalassemic according to their mild to moderate anemia, microcytosis and normal iron levels were included in this study at the hemoglobinopathy and thalassemia center of Ahvaz University of Medical Science. Patients were analyzed for hematological parameters and HbH mutations using Multiplex Gap Polymerase Chain Reaction and Multiplex Amplification Refractory Mutation System. Twelve mutations were detected in the studied population. The most common genotype was -α3.7/--MED (45%) followed by Homozygote αPoly A2 (17.5%). A total of ten different alpha-globin (α-globin) mutations were observed in patients which --MED, being the most common mutation (26.27%), followed by -α3.7 (24.37%) and αpolyA2(A>G) (18.12%). Hematological parameters such as Hb, MCV, MCH and HbH were assessed and results showed that they varied significantly among genotypes, adjusted to age and gender. This study reveals a highly diverse range of HbH patients different from what was thought in terms of both genotype and phenotype in the Khuzestan region of Iran. These findings could contribute to improve the thalassemia managing policies in this province.



Similar content being viewed by others
References
Alkindi SS et al (2013) A stepwise α-thalassemia screening strategy in high-prevalence areas. Eur J Haematol 91(2):164–169
Karamzade A et al (2014) α-Globin gene mutations in Isfahan province. Iran Hemoglobin 38(3):161–164
Vichinsky EP (2009) Alpha thalassemia major—new mutations, intrauterine management, and outcomes. ASH Educ Program Book 2009(1):35–41
Chen FE et al (2000) Genetic and clinical features of hemoglobin H disease in Chinese patients. N Engl J Med 343(8):544–550
Waye JS et al (2001) Hemoglobin H (Hb H) disease in Canada: molecular diagnosis and review of 116 cases. Am J Hematol 68(1):11–15
Galanello R, Cao A (2011) Alpha-thalassemia. Genet Med 13(2):83
Chan AY-Y et al (2007) A laboratory strategy for genoty** haemoglobin H disease in the Chinese. J Clin Pathol 60(8):931–934
Laosombat V et al (2009) Clinical features and molecular analysis in Thai patients with HbH disease. Ann Hematol 88(12):1185–1192
Liu Y et al (2000) Rapid detection of alpha-thalassaemia deletions and alpha-globin gene triplication by multiplex polymerase chain reactions. Br J Haematol 108(2):295–299
Pornprasert S et al (2018) Hematological analysis in Thai samples with deletional and nondeletional HbH diseases. Lab Med 49(2):154–159
Origa R et al (2007) Clinical and molecular analysis of haemoglobin H disease in Sardinia: haematological, obstetric and cardiac aspects in patients with different genotypes. Br J Haematol 136(2):326–332
Chui DH, Fucharoen S, Chan V (2003) Hemoglobin H disease: not necessarily a benign disorder. Blood 101(3):791–800
Hafezi-Nejad N et al (2014) Characterizing a cohort of α-thalassemia couples collected during screening for hemoglobinopathies: 14 years of an iranian experience. Hemoglobin 38(3):153–157
Papassotiriou I et al (1999) Rapid and accurate quantitation of Hb Bart’s and Hb H using weak cation exchange high performance liquid chromatography: correlation with the α-thalassemia genotype. Hemoglobin 23(3):203–211
Eng B et al (2001) Detection of severe nondeletional α-thalassemia mutations using a single-tube multiplex ARMS assay. Genet Test 5(4):327–329
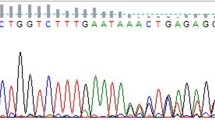
Sanger F (1992) DNA sequencing with chain-terminating inhibitors. Biotechnology 24:104–108
Farashi S, Harteveld CL (2018) Molecular basis of α-thalassemia. Blood Cells Mol Dis 70:43–53
Charoenkwan P et al (2005) Molecular and clinical features of Hb H disease in northern Thailand. Hemoglobin 29(2):133–140
Ebrahimkhani S et al (2011) Genotype-phenotype correlation in Iranian patients with Hb H disease. Hemoglobin 35(1):40–46
Baysal E et al (1995) α-Thalassaemia in the population of Cyprus. Br J Haematol 89(3):496–499
Fang J et al (2014) The Hb H disease genotypes in southern China. Hemoglobin 38(1):76–78
Öner C et al (1997) The molecular basis of Hb H disease in Turkey. Hemoglobin 21(1):41–51
Bozdogan ST et al (2015) Alpha-thalassemia mutations in Adana Province, southern Turkey: genotype-phenotype correlation. Indian J Hematol Blood Transfus 31(2):223–228
Sanchaisuriya K, Fucharoen G, Fucharoen S (2002) Hb Paksé [(α2) codon 142 (TA A → TA T or Term → Tyr)] in Thai patients with EAbart’s disease and Hb H disease. Hemoglobin 26(3):227–235
Liebhaber S, Cash FE, Ballas S (1986) Human alpha-globin gene expression. The dominant role of the alpha 2-locus in mRNA and protein synthesis. J Biol Chem 261(32):15327–15333
Farashi S et al (2015) Homozygosity for the AATA AA > AATA—polyadenylation site mutation on the α 2-globin gene causing transfusion-dependent Hb H disease in an iranian patient: a case report. Hemoglobin 39(5):355–358
Acknowledgements
We wish to thank all our colleagues in Shafa Hospital, Ahvaz, Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was signed prior to participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Paridar, M., Azizi, E., Keikhaei, B. et al. Iranian patients with hemoglobin H disease: genotype–phenotype correlation. Mol Biol Rep 46, 5041–5048 (2019). https://doi.org/10.1007/s11033-019-04955-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-019-04955-9