Abstract
Purpose
Brugada syndrome (BrS) is a risk of sudden cardiac death due to polymorphic ventricular tachycardia and ventricular fibrillation with unusual monomorphic ventricular tachycardia (MVT). Detailed characteristics of MVT and long-term outcome of catheter ablation are still unknown. This study is aimed to identify the detailed characteristics and long-term follow-up of catheter ablation in BrS patients.
Methods
We evaluated 188 patients who were diagnosed with BrS from March 1999 to March 2018. Of those, patients who developed MVT and underwent catheter ablation were included. We identified eight MVTs in seven BrS patients.
Results
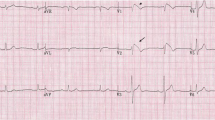
Three of them already had implantable cardioverter-defibrillator, and MVTs were terminated by cardioversion or anti-tachycardia pacing. Four patients presented with MVT originating from the right ventricular outflow tract, one patient had MVT arising from the LV septum, one patient had MVT arising from the tricuspid annulus, and one patient had bundle branch reentry ventricular tachycardia. All MVTs were successfully treated by catheter ablation in the acute phase, and seven of eight (87.5%) were free from ventricular tachyarrhythmia during the long-term follow-up (median, 7.2 years).
Conclusions
All MVT cases were successfully treated by catheter ablation. We observed high ventricular arrhythmia free rate following catheter ablation during the long-term follow-up period. BrS patients who developed MVT should consider catheter ablation.



Similar content being viewed by others
References
Rodriguez-Manero M, Sacher F, de Asmundis C, Maury P, Lambiase PD, Sarkozy A, et al. Monomorphic ventricular tachycardia in patients with Brugada syndrome: a multicenter retrospective study. Heart Rhythm. 2016;13:669–82.
Akbarzadeh M, Haghjoo M. Monomorphic ventricular tachycardia originating from right ventricular outflow tract as a trigger for the recurrent ventricular fibrillation in a patient with Brugada syndrome. Res Cardiovasc Med. 2014;3:e17113.
Ogawa M, Kumagai K, Saku K. Spontaneous right ventricular outflow tract tachycardia in a patient with Brugada syndrome. J Cardiovasc Electrophysiol. 2001;12:838–40.
Goto M, Sato M, Kitazawa H, Komatsu Y, Fuse K, Takahashi M, et al. Brugada syndrome combined with monomorphic ventricular tachycardia and atrioventricular nodal reentrant tachycardia. Intern Med. 2015;54:1223–6.
Ueyama T, Shimizu A, Esato M, Yoshiga S, Sawa A, Suzuki S, et al. Pilsicainide-induced Brugada-type ECG and ventricular arrhythmias originating from the left posterior fascicle in a case with Brugada syndrome associated with idiopathic left ventricular tachycardia. Europace. 2008;10:86–90.
Wilde AAM, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, et al. Proposed diagnostic criteria for the Brugada syndrome: consensus report. Eur Heart J. 2002;23:1648–54.
Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659–70.
Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10(12):1932–63.
Kitamura T, Fukamizu S, Kawamura I, Hojo R, Aoyama Y, Nishizaki M, et al. Clinical characteristics and long-term prognosis of senior patients with Brugada syndrome. JACC Clin Electrophysiol. 2017;3:57–67.
Kitamura T, Fukamizu S, Kawamura I, Hojo R, Aoyama Y, Komiyama K, et al. Long-term efficacy of catheter ablation for paroxysmal atrial fibrillation in patients with Brugada syndrome and an implantable cardioverter-defibrillator to prevent inappropriate shock therapy. Heart Rhythm. 2016;13:1455–9.
Mizusawa Y, Sakurada H, Nishizaki M, Hiraoka M. Effects of low-dose quinidine on ventricular tachyarrhythmias in patients with Brugada syndrome: low-dose quinidine therapy as an adjunctive treatment. J Cardiovasc Pharmacol. 2006;47:359–64.
Hutchinson MD, Gerstenfeld EP, Desjardins B, Bala R, Riley MP, Garcia FC, et al. Endocardial unipolar voltage map** to detect epicardial VT substrate in patients with nonischemic left ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2011;4(1):49–55.
Brodie OT, Michowitz Y, Belhassen B. Pharmacological therapy in Brugada syndrome. Arrhythm Electrophysiol Rev. 2018;7:135–42.
Roberts JD, Gollob MH, Young C, Connors SP, Gray C, Wilton SB, et al. Bundle branch re-entrant ventricular tachycardia: novel genetic mechanisms in a life-threatening arrhythmia. JACC Clin Electrophysiol. 2017;3:276–88.
Mazur A, Iakobishvili Z, Kusniec J, Strasberg B. Bundle branch reentrant ventricular tachycardia in a patient with the Brugada electrocardiographic pattern. Ann Noninvasive Electrocardiol. 2003;8:352–5.
Sideris S, Archontakis S, Gatzoulis KA, Anastasakis A, Sotiropoulos I, Arsenos P, et al. The subcutaneous ICD as an alternative to the conventional ICD system: initial experience in Greece and a review of the literature. Hell J Cardiol. 2017;58:4–16.
Kondo Y, Ueda M, Kobayashi Y, Schwab JO. New horizon for infection prevention technology and implantable device. J Arrhythm. 2016;32:297–302.
Nakashima T, Takasugi N, Sahashi Y, Suzuki K, Kubota T, Aoyama T, et al. Ventricular tachycardia sensitive to antitachycardia pacing in a patient with severely symptomatic Brugada syndrome. J Interv Card Electrophysiol. 2018;55:239. https://doi.org/10.1007/s10840-018-0464-6.
Bertomeu-Gonzalez V, Ruiz-Granell R, Garcia-Civera R, Morell-Cabedo S, Ferrero A. Syncopal monomorphic ventricular tachycardia with pleomorphism, sensitive to antitachycardia pacing in a patient with Brugada syndrome. Europace. 2006;8:1048–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This retrospective observational study was approved by the Institutional Review Board of Tokyo Metropolitan Hiroo Hospital, Tokyo, Japan.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tokioka, S., Fukamizu, S., Kitamura, T. et al. Catheter ablation for monomorphic ventricular tachycardia in Brugada syndrome patients: detailed characteristics and long-term follow-up. J Interv Card Electrophysiol 57, 97–103 (2020). https://doi.org/10.1007/s10840-019-00620-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00620-0