Abstract
Background
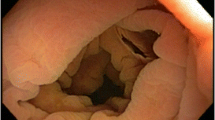
Insufflation of the colon allows for adequate visualization of the mucosal tissue and advancement of the endoscope during colonoscopy. Most colonoscopies are performed with sedation to mitigate discomfort and enhance the colonoscopy experience for both the patient and the endoscopist.
Aim
We aimed to evaluate factors associated with difficulty maintaining insufflation.
Methods
A cross-sectional study of individuals undergoing colonoscopy at the Oklahoma City Veterans Affairs Medical Center was performed. Experiencing difficulty maintaining air insufflation during colonoscopy was assessed with a questionnaire completed by the performing endoscopist at the end of procedure. Information regarding procedure times, sedation used, demographics, comorbidities, surgical history, and medications used was extracted from the medical record. A multivariate regression analysis was performed to identify factors associated with difficulty maintaining air insufflation. A P value < 0.05 was considered significant.
Results
996 Patients were included for the analysis. Difficulty with insufflation was reported in 240 (24%) colonoscopies; mean age of 63.8 ± 10.4 years old and 13% were female. Fellow trainees were involved in 669 (67%) colonoscopies. Older age (OR 1.02, P 0.03, CI [1.00–1.04]), diabetes (OR 1.5, 95% CI [1.03, 2.05]), fellow’s involvement (OR 2.6. (95% CI [1.68, 4.09]), total procedure time (OR 1.02, 95% CI [1.00, 1.03]), mean number of adenomas (OR 1.05, 95% CI [1.00, 1.09]), and MAC use (OR 2.6, 95% CI [1.80, 3.85]) were independent predictors for difficulty in maintaining air insufflation.
Conclusion
Our findings suggest that endoscopists should be cognizant of colon insufflation issues in older, diabetic patients undergoing colonoscopies under deep sedation, particularly if prolonged procedure is anticipated or encountered.

Similar content being viewed by others
Data availability
Study materials will not be made available.
Abbreviations
- CRC:
-
Colorectal cancer
- MAC:
-
Monitored anesthesia care
- ADR:
-
Adenoma detection rate
- BBPS:
-
Boston Bowel Preparation Scale
- VAMC:
-
Veterans Affairs Medical Center
- EMR:
-
Electronic medical record
- COPD:
-
Chronic obstructive pulmonary disease
- BMI:
-
Body mass index
- SD:
-
Standard deviation
References
Bevan R, Blanks RG, Nickerson C, et al. Factors affecting adenoma detection rate in a national flexible sigmoidoscopy screening programme: a retrospective analysis. Lancet Gastroenterol. Hepatol. 2019;4:239–247.
Kumar S, Thosani N, Ladabaum U, et al. Adenoma miss rates associated with a 3-minute versus 6-minute colonoscopy withdrawal time: a prospective, randomized trial. Gastrointest Endosc. 2017;85:1273–1280.
Castaneda D, Popov VB, Verheyen E, Wander P, Gross SA. New technologies improve adenoma detection rate, adenoma miss rate, and polyp detection rate: a systematic review and meta-analysis. Gastrointest Endosc. 2018;88:209-222.e211.
Keswani RN, Crockett SD, Calderwood AH. AGA Clinical Practice Update on Strategies to Improve Quality of Screening and Surveillance Colonoscopy: Expert Review. Gastroenterology. 2021;161:701–711.
Nemoto D, Suzuki S, Mori H, et al. Inhibitory effect of lidocaine on colonic spasm during colonoscopy: A multicenter double-blind, randomized controlled trial. Dig Endosc. 2019;31:173–179.
Horváth VJ, Putz Z, Izbéki F, et al. Diabetes-related dysfunction of the small intestine and the colon: focus on motility. Curr. Diabetes Rep. 2015;15:94.
Liu TT, Yi CH, Chen CL, Liu HT, Chen TY. Influence of intravenous propofol sedation on anorectal manometry in healthy adults. The American Journal of the Medical Sciences. 2009;337:429–431.
Tran K, Kuo B, Zibaitis A, Bhattacharya S, Cote C, Belkind-Gerson J. Effect of propofol on anal sphincter pressure during anorectal manometry. J Pediatr Gastroenterol Nutr. 2014;58:495–497.
Wernli KJ, Brenner AT, Rutter CM, Inadomi JM. Risks Associated With Anesthesia Services During Colonoscopy. Gastroenterology. 2016;150:888–894; quiz e818.
Aziz M, Weissman S, Fatima R, et al. Impact of propofol sedation versus opioid/benzodiazepine sedation on colonoscopy outcomes: a systematic review with meta-analysis. Endosc. Int. Open. 2020;8:E701–E707.
Pace D, Borgaonkar M. Deep sedation for colonoscopy is unnecessary and wasteful. CMAJ. 2018;190:E153–E154.
Rex DK, Imperiale TF, Latinovich DR, Bratcher LL. Impact of bowel preparation on efficiency and cost of colonoscopy. The American Journal of Gastroenterology. 2002;97:1696–1700.
Kang H, Thoufeeq MH. Size of colorectal polyps determines time taken to remove them endoscopically. Endoscopy International Open. 2018;6:E610–E615.
Bitar H, Zia H, Bashir M, et al. Impact of fellowship training level on colonoscopy quality and efficiency metrics. Gastrointest. Endosc. 2018;88:378–387.
Spier BJ, Benson M, Pfau PR, Nelligan G, Lucey MR, Gaumnitz EA. Colonoscopy training in gastroenterology fellowships: determining competence. Gastrointestinal Endoscopy. 2010;71:319–324.
He W, Bryns S, Kroeker K, Basu A, Birch D, Zheng B. Eye gaze of endoscopists during simulated colonoscopy. J Robot Surg. 2020;14:137–143.
Bassotti G, Gaburri M, Imbimbo BP, Morelli A, Whitehead WE. Distension-stimulated propagated contractions in human colon. Dig Dis Sci. 1994;39:1955–1960.
Schiller LR, Santa Ana CA, Schmulen AC, Hendler RS, Harford WV, Fordtran JS. Pathogenesis of fecal incontinence in diabetes mellitus: evidence for internal-anal-sphincter dysfunction. The New England Journal of Medicine. 1982;307:1666–1671.
Frudinger A, Halligan S, Bartram CI, Price AB, Kamm MA, Winter R. Female Anal Sphincter: Age-related Differences in Asymptomatic Volunteers with High-Frequency Endoanal US. Radiology. 2002;224:417–423.
Huebner M, Margulies RU, Fenner DE, Ashton-Miller JA, Bitar KN, DeLancey JO. Age effects on internal anal sphincter thickness and diameter in nulliparous females. Dis Colon Rectum. 2007;50:1405–1411.
Funding
None.
Author information
Authors and Affiliations
Contributions
MFM was involved in study design, statistical analyses, and drafting and final approval of the manuscript; NB was involved in study design, data collection, and drafting the manuscript; IA was involved in data analyses and drafting the manuscript; BY, AG, and MN were involved in data collection; TJC was involved in study design and data collection; RH was involved in critical revision of the article, and final approval. Writing Assistance: none.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
The study was approved by the University of Oklahoma Health Sciences Institutional Review Board (IRB), which complies with acceptable international standards (such as the Treaty of Helsinki).
Informed consent
A waiver of informed consent was obtained from the University of Oklahoma Institutional Review Board, as the study was deemed no more than minimal risk, given its retrospective nature.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An editorial commenting on this article is available at https://doi.org/10.1007/s10620-022-07594-6.
Rights and permissions
About this article
Cite this article
Madhoun, M.F., Bader, N., Ali, I. et al. Factors Associated with Difficulty Maintaining Insufflation of the Colon During Endoscopy. Dig Dis Sci 68, 202–207 (2023). https://doi.org/10.1007/s10620-022-07592-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07592-8