Abstract
Background
Recently, endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) procedures have been gradually established; nonetheless, some adverse events (AEs) have been reported. Dilation procedures using a non-cautery or cautery device increase the incidence of AEs in EUS-HGS.
Aims
We evaluated EUS-HGS procedures without dilation and the factors associated with dilation.
Methods
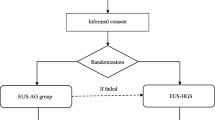
We enrolled 79 patients who underwent EUS-HGS between July 2015 and March 2021 at two centers, 72 of whom had technical success (72/79, 91%). During the EUS-HGS procedures, we defined patients without dilation procedures as the dilation (−) group. We divided the patients into two groups: the dilation (+) (35 patients) and dilation (−) (37 patients) groups. We performed a propensity score matching analysis to adjust for confounding bias between the two groups. Multivariable logistic regression analysis was conducted to identify factors associated with dilation.
Results
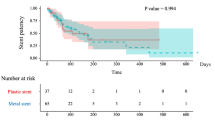
There was no difference in clinical success rate between the dilation (+) and dilation (−) groups (91% vs. 95%, P = 0.545). The AE rate (P = 0.013) and long procedure time (P = 0.017) were significantly higher in the dilation (+) group than in the dilation (−) group before and after propensity score matching. Factors associated with dilation were plastic stent placement (odds ratio [OR], 6.96; 95% confidence interval [CI], 1.68–28.7; P = 0.007) and puncture angle of ≤ 90° (OR, 44.6; 95% CI, 5.1–390; P < 0.001).
Conclusions
A dilation procedure in EUS-HGS may not always be necessary. However, patients with an angle of ≤ 90° between the needle and intrahepatic biliary tract or plastic stent deployment require dilation procedures.





Similar content being viewed by others
References
Isayama H, Nakai Y, Itoi T et al. Clinical practice guidelines for safe performance of endoscopic ultrasound/ultrasonography-guided biliary drainage: 2018. J Hepatobiliary Pancreat Sci. 2019;26:249–269.
Teoh AYB, Dhir V, Kida M et al. Consensus guidelines on the optimal management in interventional EUS procedures: results from the Asian EUS group RAND/UCLA expert panel. Gut. 2018;67:1209–1228.
Artifon EL, Marson FP, Gaidhane M, Kahaleh M, Otoch JP. Hepaticogastrostomy or choledochoduodenostomy for distal malignant biliary obstruction after failed ERCP: is there any difference? Gastrointest Endosc. 2015;81:950–959.
Uemura RS, Khan MA, Otoch JP, Kahaleh M, Montero EF, Artifon ELA. EUS-guided choledochoduodenostomy versus hepaticogastrostomy: a systematic review and meta-analysis. J Clin Gastroenterol. 2018;52:123–130.
Wang K, Zhu J, **ng L, Wang Y, ** Z, Li Z. Assessment of efficacy and safety of EUS-guided biliary drainage: a systematic review. Gastrointest Endosc. 2016;83:1218–1227.
Khan MA, Akbar A, Baron TH et al. Endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. Dig Dis Sci. 2016;61:684–703. https://doi.org/10.1007/s10620-015-3933-0.
Moole H, Bechtold ML, Forcione D, Puli SR. A meta-analysis and systematic review: success of endoscopic ultrasound guided biliary stenting in patients with inoperable malignant biliary strictures and a failed ERCP. Medicine (Baltimore). 2017;96:e5154.
Park DH, Lee TH, Paik WH et al. Feasibility and safety of a novel dedicated device for one-step EUS-guided biliary drainage: a randomized trial. J Gastroenterol Hepatol. 2015;30:1461–1466.
Ogura T, Higuchi K. Endoscopic ultrasound-guided hepaticogastrostomy: technical review and tips to prevent adverse events. Gut Liver. 2021;15:196–205.
Lee TH, Choi JH, Lee SS et al. A pilot proof-of-concept study of a modified device for one-step endoscopic ultrasound-guided biliary drainage in a new experimental biliary dilatation animal model. World J Gastroenterol. 2014;20:5859–5866.
Paik WH, Lee TH, Park DH et al. EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: a multicenter randomized clinical trial. Am J Gastroenterol. 2018;113:987–997.
Maehara K, Hijioka S, Nagashio Y et al. Endoscopic ultrasound-guided hepaticogastrostomy or hepaticojejunostomy without dilation using a stent with a thinner delivery system. Endosc Int Open. 2020;8:E1034–E1038.
Ogura T, Masuda D, Takeuchi T, Fukunishi S, Higuchi K. Liver impaction technique to prevent shearing of the guidewire during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2015;47:E583–E584.
Kawakami H, Kubota Y, Makiyama H, Sato S, Ban T. Uneven double-lumen cannula for rescue guidewire technique in endoscopic ultrasonography-guided hepaticogastrostomy. Endosopy. 2017;49:E264–E265.
Isayama H, Hamada T, Yasuda I et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015;27:259–264.
Cotton PB, Eisen GM, Aabakken L et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454.
Yamamoto Y, Ogura T, Nishioka N et al. Risk factors for adverse events associated with bile leak during EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2020;9:110–115.
Nakai Y, Oyama H, Kanai S et al. Double guidewire technique using an uneven double lumen catheter for endoscopic ultrasound-guided interventions. Dig Dis Sci. 2021;66:1540–1547. https://doi.org/10.1007/s10620-020-06345-9.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–3107.
Hathorn KE, Bazarbashi AN, Sack JS et al. EUS-guided biliary drainage is equivalent to ERCP for primary treatment of malignant distal biliary obstruction: a systematic review and meta-analysis. Endosc Int Open. 2019;7:E1432–E1441.
Ogura T, Nishioka N, Ueno S et al. Effect of echoendoscope angle on success of guidewire manipulation during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2021;53:369–375.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported in part by JSPS KAKENHI (Grant Number: JP18K09945).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An editorial commenting on this article is available at https://doi.org/10.1007/s10620-022-07560-2.
Rights and permissions
About this article
Cite this article
Ohno, A., Fujimori, N., Kaku, T. et al. Feasibility and Efficacy of Endoscopic Ultrasound-Guided Hepaticogastrostomy Without Dilation: A Propensity Score Matching Analysis. Dig Dis Sci 67, 5676–5684 (2022). https://doi.org/10.1007/s10620-022-07555-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07555-z