Abstract
Background and Aims
Guidelines cite extensive gastric intestinal metaplasia (GIM) as a bigger risk factor for gastric cancer (GC) than limited GIM and an indication for endoscopic surveillance. Data on progression of extensive GIM to GC in the USA are limited. This study aimed to estimate the prevalence and progression rates of extensive GIM in a US cohort.
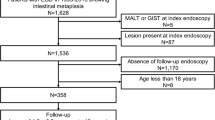
Methods
This retrospective study assessed the prevalence of extensive GIM between 1/1/1990 and 8/1/2019 at a large academic medical center. Multivariable regression was used to identify predictors of extensive GIM. Incidence of GC on follow-up was calculated as number of new diagnoses divided by person-years of follow-up. Presence of GIM on subsequent follow-up endoscopy was assessed.
Results
Of 1256 individuals with GIM, 352 (28%) had extensive GIM and 904 (72%) had limited GIM. On multivariable analysis, older age (OR 1.01, 95% CI 1.00–1.02) and Hispanic ethnicity (OR 1.55, 95% CI 1.11–2.16) were predictive of extensive GIM. The annual incidence of GC for GIM overall was 0.09%. There was no difference in progression to GC between extensive or limited GIM (IRR 0, 95% CI 0–2.6), or to advanced lesions overall (IRR 0.37, 95% CI 0.04–1.62). 70% of individuals had persistent GIM on follow-up biopsy, and 22% with limited GIM had extensive GIM on follow-up biopsy.
Conclusions
28% of individuals with GIM have the extensive subtype, and are more likely to be older and of Hispanic ethnicity. There was no difference in progression to GC between extensive and limited GIM. Further research is needed to better assess risk of GIM in the US context.
Similar content being viewed by others
Abbreviations
- US:
-
United States
- GIM:
-
Gastric intestinal metaplasia
- GC:
-
Gastric cancer
- LGD:
-
Low grade dysplasia
- HGD:
-
High grade dysplasia
- AGA:
-
American Gastroenterological Association
- MAPS:
-
Management of Epithelial Precancerous Conditions in the Stomach
References
Cronin KA, Lake AJ, Scott S et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer. 2018;124:2785–2800.
SEER Cancer Stat Facts: Stomach Cancer. National Cancer Institute.
Choi KS, Jun JK, Suh M et al. Effect of endoscopy screening on stage at gastric cancer diagnosis: results of the National Cancer Screening Programme in Korea. Br J Cancer. 2015;112:608–612.
Altayar O, Davitkov P, Shah SC et al. AGA technical review on gastric intestinal metaplasia—epidemiology and risk factors. Gastroenterology. 2020;158:732.e16-744.e16.
Correa P, Piazuelo MB, Wilson KT. Pathology of gastric intestinal metaplasia: clinical implications. Am J Gastroenterol. 2010;105:493–498.
Zhang X, Li M, Chen S et al. Endoscopic screening in Asian countries is associated with reduced gastric cancer mortality: A meta-analysis and systematic review. Gastroenterology. 2018;155:347-354.e9.
Shah SC, Gawron AJ, Li D. Surveillance of gastric intestinal metaplasia. Am J Gastroenterol. 2020;115:641–644.
Shah SC, Gawron AJ, Mustafa RA et al. Histologic subty** of gastric intestinal metaplasia: Overview and considerations for clinical practice. Gastroenterology. 2020;158:745–750.
Marcos P, Brito-Gonçalves G, Libânio D et al. Endoscopic grading of gastric intestinal metaplasia on risk assessment for early gastric neoplasia: can we replace histology assessment also in the West? Gut. 2020;69:1762–1768.
Bisschops R, Areia M, Coron E et al. Performance measures for upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2016;48:843–864.
Park WG, Shaheen NJ, Cohen J et al. Quality indicators for EGD. Gastrointest Endosc. 2015;81:17–30.
Sharma P, Parasa S, Shaheen N. Develo** quality metrics for upper endoscopy. Gastroenterology. 2020;158:9–13.
Song H, Ekheden IG, Zheng Z et al. Incidence of gastric cancer among patients with gastric precancerous lesions: observational cohort study in a low risk Western population. BMJ Br Med J. 2015;351:h3867.
Huang RJ, Ende AR, Singla A et al. Prevalence, risk factors, and surveillance patterns for gastric intestinal metaplasia among patients undergoing upper endoscopy with biopsy. Gastrointest Endosc. 2020;91:70-77.e1.
Fennerty MB, Emerson JC, Sampliner RE et al. Gastric intestinal metaplasia in ethnic groups in the southwestern United States. Cancer Epidemiol Biomark Prev. 1992;1:293–296.
Sonnenberg A, Genta RM. Changes in the gastric mucosa with aging. Clin Gastroenterol Hepatol. 2015;13:2276–2281.
Choi CE, Sonnenberg A, Turner K et al. High prevalence of gastric preneoplastic lesions in East Asians and Hispanics in the USA. Dig Dis Sci. 2015;60:2070–2076. https://doi.org/10.1007/s10620-015-3591-2.
Gupta S, Li D, El Serag HB et al. AGA clinical practice guidelines on management of gastric intestinal metaplasia. Gastroenterology. 2020;158:693–702.
Pimentel-Nunes P, Libanio D, Marcos-Pinto R et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51:365–388.
Banks M, Graham D, Jansen M et al. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;68:1545–1575.
Reddy KM, Chang JI, Shi JM et al. Risk of gastric cancer among patients with intestinal metaplasia of the stomach in a US integrated health care system. Clin Gastroenterol Hepatol. 2016;14:1420–1425.
Dhingra R, Natov NS, Daaboul Y et al. Increased risk of progression to gastric adenocarcinoma in patients with non-dysplastic gastric intestinal metaplasia versus a control population. Dig Dis Sci. 2020;65:3316–3323. https://doi.org/10.1007/s10620-019-06031-5.
Li D, Bautista MC, Jiang SF et al. Risks and predictors of gastric adenocarcinoma in patients with gastric intestinal metaplasia and dysplasia: a population-based study. Am J Gastroenterol. 2016;111:1104–1113.
Tan MC, Mallepally N, Liu Y et al. Demographic and lifestyle risk factors for gastric intestinal metaplasia among US veterans. Am J Gastroenterol. 2020;115:381–387.
Nguyen TH, Tan MC, Liu Y et al. Prevalence of gastric intestinal metaplasia in a multiethnic US veterans population. Clin Gastroenterol Hepatol. 2020;19:269–276.
Shichijo S, Hirata Y, Niikura R et al. Histologic intestinal metaplasia and endoscopic atrophy are predictors of gastric cancer development after Helicobacter pylori eradication. Gastrointest Endosc. 2016;84:618–624.
Gawron AJ, Shah SC, Altayar O et al. AGA technical review on gastric intestinal metaplasia—natural history and clinical outcomes. Gastroenterology. 2020;158:705.e5-731.e5.
Tsubono Y, Hisamichi S. Screening for gastric cancer in Japan. Gastric Cancer. 2000;3:9–18.
Mizoue T, Yoshimura T, Tokui N et al. Prospective study of screening for stomach cancer in Japan. Int J Cancer. 2003;106:103–107.
Choi KS, Jun JK, Park E-C et al. Performance of different gastric cancer screening methods in Korea: a population-based study. PLoS One. 2012;7:e50041–e50041.
Jung KW, Won YJ, Kong HJ et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat. 2014;46:109–123.
Kim GH, Bang SJ, Ende AR et al. Is screening and surveillance for early detection of gastric cancer needed in Korean Americans? Korean J Intern Med. 2015;30:747–758.
Cho E, Kang MH, Choi KS et al. Cost-effectiveness outcomes of the national gastric cancer screening program in South Korea. Asian Pac J Cancer Prev. 2013;14:2533–2540.
Kobayashi K, Mine T. Cost-effective analysis of gastric cancer screening in Japan. Gastrointest Endosc. 2004;59:P137.
Funding
ML—NIH K08 DK125876-01A1 and MSKCC Department of Subspecialty Medicine Award. ASF—NIH T32DK083256.
Author information
Authors and Affiliations
Contributions
Study concept and design: ML, HT, JK, JAA, CH. Acquisition of data: ML, HT, ST, FL. Analysis and interpretation of data: ML, HT, ASF, JK, JAA, CH. Drafting of the manuscript: ML. Critical revision of the manuscript for important intellectual content: ML, HT, ASF, JK, ST, FL, JAA, CH.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Columbia University Irving Medical Center approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Laszkowska, M., Truong, H., Faye, A.S. et al. Prevalence of Extensive and Limited Gastric Intestinal Metaplasia and Progression to Dysplasia and Gastric Cancer. Dig Dis Sci 67, 3693–3701 (2022). https://doi.org/10.1007/s10620-021-07276-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07276-9