Abstract
Purpose
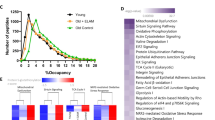
Aging contributes significantly to cardiovascular diseases and cardiac dysfunction, leading to the upregulation of matrix metalloproteinase-9 (MMP-9) in the heart and a significant decrease in hydrogen sulfide (H2S) content, coupled with impaired cardiac diastolic function. This study explores whether supplementing exogenous hydrogen sulfide during aging ameliorates the decline in H2S concentration in the heart, suppresses MMP-9 expression, and improves the age-associated impairment in cardiac morphology and function.
Methods
We collected plasma from healthy individuals of different ages to determine the relationship between aging and H2S and MMP-9 levels through Elisa detection and liquid chromatography-tandem mass spectrometry (LC/MC) detection of plasma H2S content. Three-month-old mice were selected as the young group, while 18-month-old mice were selected as the old group, and sodium hydrosulfide (NaHS) was injected intraperitoneally from 15 months old until 18 months old as the old + NaHS group. Plasma MMP-9 content was detected using Elisa, plasma H2S content, cardiac H2S content, and cystathionine gamma-lyase (CSE) activity were detected using LC/MC, and cardiac function was detected using echocardiography. Heart structure was assessed using hematoxylin and eosin staining, Masone staining was used to detect the degree of cardiac fibrosis, while western blot was used to detect the expression of MMP-9, CSE, and aging marker proteins. Knockdown of MMP-9 and CSE in H9c2 cells using small interfering RNA was carried out to determine the upstream–downstream relationship between MMP-9 and CSE.
Results
H2S content in the plasma of healthy individuals decreases with escalating age, whereas MMP-9 level rises with age progression. Aging leads to a decrease in H2S levels in the heart and plasma of mice, severe impairment of cardiac diastolic function, interstitial relaxation, and fibrosis of the heart. Supplementing with exogenous H2S can improve these phenomena.
Conclusion
H2S maintains the structure and function of the heart by inhibiting the expression of MMP-9 during the aging process.








Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code Availability
The code that support the findings of this study are available from the corresponding author upon reasonable request.
References
Pagan L, Gomes M, Gatto M, et al. The role of oxidative stress in the aging heart. Antioxid. 2022;11(2):336. https://doi.org/10.3390/antiox11020336.
Chiao Y, Ramirez T, Zamilpa R, et al. Matrix metalloproteinase-9 deletion attenuates myocardial fibrosis and diastolic dysfunction in ageing mice. Cardiovascular Res. 2012;96(3):444–55. https://doi.org/10.1093/cvr/cvs275.
Lindsey M, Goshorn D, Squires C, et al. Age-dependent changes in myocardial matrix metalloproteinase/tissue inhibitor of metalloproteinase profiles and fibroblast function. Cardiovascular Res. 2005;66(2):410–9. https://doi.org/10.1016/j.cardiores.2004.11.029.
Kwak H. Aging, exercise, and extracellular matrix in the heart. J Exerc rehabilitation. 2013;9(3):338–47. https://doi.org/10.12965/jer.130049.
Angelini A, Trial J, Ortiz-Urbina J, Cieslik K. Mechanosensing dysregulation in the fibroblast: a hallmark of the aging heart. Ageing Res Rev. 2020;63:101150. https://doi.org/10.1016/j.arr.2020.101150.
Huang Y, **a J, Zheng J, et al. Deficiency of cartilage oligomeric matrix protein causes dilated cardiomyopathy. Basic Res Cardiol. 2013;108(5):374. https://doi.org/10.1007/s00395-013-0374-9.
Ackers-Johnson M, Tan W, Foo R. Following hearts, one cell at a time: recent applications of single-cell RNA sequencing to the understanding of heart disease. Nat Commun. 2018;9(1):4434. https://doi.org/10.1038/s41467-018-06894-8.
Ringström N, Edling C, Nalesso G, Jeevaratnam K. Framing heartaches: the cardiac ECM and the effects of age. Int J Mol Sci. 2023;24(5):4713. https://doi.org/10.3390/ijms24054713.
Rabkin S. The role matrix metalloproteinases in the production of aortic aneurysm. Prog Mol Biol Transl Sci. 2017;147:239–65. https://doi.org/10.1016/bs.pmbts.2017.02.002.
Cui N, Hu M, Khalil R. Biochemical and biological attributes of matrix metalloproteinases. Prog Mol Biol Transl Sci. 2017;147:1–73. https://doi.org/10.1016/bs.pmbts.2017.02.005.
Sternlicht M, Werb Z. How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol. 2001;17:463–516. https://doi.org/10.1146/annurev.cellbio.17.1.463.
Gottschall P, Deb S. Regulation of matrix metalloproteinase expressions in astrocytes, microglia and neurons. Neuroimmunomodulation. 1996;3:69–75. https://doi.org/10.1159/000097229.
Bond M, Fabunmi R, Baker A, Newby A. Synergistic upregulation of metalloproteinase-9 by growth factors and inflammatory cytokines: an absolute requirement for transcription factor NF-kappa B. FEBS Lett. 1998;435(1):29–34. https://doi.org/10.1016/s0014-5793(98)01034-5.
Kolluru G, Shackelford R, Shen X, Dominic P, Kevil C. Sulfide regulation of cardiovascular function in health and disease. Nat reviews Cardiol. 2023;20(2):109–25. https://doi.org/10.1038/s41569-022-00741-6.
Cirino G, Szabo C, Papapetropoulos A. Physiological roles of hydrogen sulfide in mammalian cells, tissues, and organs. Physiol Rev. 2023;103(1):31–276. https://doi.org/10.1152/physrev.00028.2021.
Perridon B, Leuvenink H, Hillebrands J, van Goor H, Bos E. The role of hydrogen sulfide in aging and age-related pathologies. Aging. 2016;8(10):2264–89. https://doi.org/10.18632/aging.101026.
Calabrese V, Scuto M, Salinaro A, et al. Hydrogen sulfide and carnosine: modulation of oxidative stress and inflammation in kidney and brain axis. Antioxid (Basel Switzerland). 2020;9(12):1303. https://doi.org/10.3390/antiox9121303.
Salloum F. Hydrogen sulfide and cardioprotection–mechanistic insights and clinical translatability. Pharmacol Ther. 2015;152:11–7. https://doi.org/10.1016/j.pharmthera.2015.04.004.
Hou C, Wang M, Sun C, et al. Protective effects of hydrogen sulfide in the ageing kidney. Oxidative Med Cell Longev. 2016;2016:7570489. https://doi.org/10.1155/2016/7570489.
Srilatha B, Muthulakshmi P, Adaikan P, Moore P. Endogenous hydrogen sulfide insufficiency as a predictor of sexual dysfunction in aging rats. Aging Male. 2012;15(3):153–8. https://doi.org/10.3109/13685538.2012.668722.
Zhu J, Wang Y, Rivett A, et al. Deficiency of cystathionine gamma-lyase promotes aortic elastolysis and medial degeneration in aged mice. J Mol Cell Cardiol. 2022;171:30–44. https://doi.org/10.1016/j.yjmcc.2022.06.011.
Tan B, ** S, Sun J, et al. New method for quantification of gasotransmitter hydrogen sulfide in biological matrices by LC-MS/MS. Sci Rep. 2017;7:46278. https://doi.org/10.1038/srep46278.
Liao L, Chen Z, Wang S, et al. NLRP3 inflammasome activation contributes to the pathogenesis of cardiocytes aging. Aging. 2021;13(16):20534–51. https://doi.org/10.18632/aging.203435.
Borisov V, Forte E. Terminal oxidase cytochrome bd protects bacteria against hydrogen sulfide toxicity. Biochem Biokhimiia. 2021;86(1):22–32. https://doi.org/10.1134/s000629792101003x.
Abe K, Kimura H. The possible role of hydrogen sulfide as an endogenous neuromodulator. J Neurosci. 1996;16(3):1066–71. https://doi.org/10.1523/jneurosci.16-03-01066.1996.
Malaeb H, Choucair I, Wang Z, et al. Stable isotope dilution mass spectrometry quantification of hydrogen sulfide and thiols in biological matrices. Redox Biol. 2022;55:102401. https://doi.org/10.1016/j.redox.2022.102401.
Zivanovic J, Kouroussis E, Kohl J, et al. Selective persulfide detection reveals evolutionarily conserved antiaging effects of S-sulfhydration. Cell Metabol. 2019;30(6):1152-e7013. https://doi.org/10.1016/j.cmet.2019.10.007.
Li Y, Liu M, Song X, et al. Exogenous hydrogen sulfide ameliorates diabetic myocardial fibrosis by inhibiting cell aging through SIRT6/AMPK autophagy. Front Pharmacol. 2020;11:1150. https://doi.org/10.3389/fphar.2020.01150.
Pan L, Liu X, Gong Q, Yang H, Zhu Y. Role of cystathionine γ-lyase/hydrogen sulfide pathway in cardiovascular disease: a novel therapeutic strategy? Antioxid Redox Signal. 2012;17(1):106–18. https://doi.org/10.1089/ars.2011.4349.
Yang G, Pei Y, Teng H, Cao Q, Wang R. Specificity protein-1 as a critical regulator of human cystathionine gamma-lyase in smooth muscle cells. J Biol Chem. 2011;286(30):26450–60. https://doi.org/10.1074/jbc.M111.266643.
Zhang L, Yang G, Tang G, Wu L, Wang R. Rat pancreatic level of cystathionine γ-lyase is regulated by glucose level via specificity protein 1 (SP1) phosphorylation. Diabetologia. 2011;54(10):2615–25. https://doi.org/10.1007/s00125-011-2187-4.
Gonzalez Bosc L, Osmond J, Giermakowska W, et al. NFAT regulation of cystathionine γ-lyase expression in endothelial cells is impaired in rats exposed to intermittent hypoxia. Am J Physiol Heart Circ Physiol. 2017;312(4):H791–9. https://doi.org/10.1152/ajpheart.00952.2015.
Fan K, Li N, Qi J, et al. Wnt/β-catenin signaling induces the transcription of cystathionine-γ-lyase, a stimulator of tumor in colon cancer. Cell Signal. 2014;26(12):2801–8. https://doi.org/10.1016/j.cellsig.2014.08.023.
Sen N, Paul B, Gadalla M, et al. Hydrogen sulfide-linked sulfhydration of NF-κB mediates its antiapoptotic actions. Mol Cell. 2012;45(1):13–24. https://doi.org/10.1016/j.molcel.2011.10.021.
Kabil O, Yadav V, Banerjee R. Heme-dependent metabolite switching regulates H2S synthesis in response to endoplasmic reticulum (ER) stress. J Biol Chem. 2016;291(32):16418–23. https://doi.org/10.1074/jbc.C116.742213.
Hine C, Harputlugil E, Zhang Y, et al. Endogenous hydrogen sulfide production is essential for dietary restriction benefits. Cell. 2015;160:132–44. https://doi.org/10.1016/j.cell.2014.11.048.
Kandil S, Brennan L, McBean G. Glutathione depletion causes a JNK and p38MAPK-mediated increase in expression of cystathionine-gamma-lyase and upregulation of the transsulfuration pathway in C6 glioma cells. Neurochem Int. 2010;56(4):611–9. https://doi.org/10.1016/j.neuint.2010.01.004.
van Loo G, Bertrand M. Death by TNF: a road to inflammation. Nat Rev Immunol. 2023;23(5):289–303. https://doi.org/10.1038/s41577-022-00792-3.
Saha S, Chakraborty P, **ong X, et al. Cystathionine β-synthase regulates endothelial function via protein S-sulfhydration. FASEB J. 2016;30(1):441–56. https://doi.org/10.1096/fj.15-278648.
Ijaz N, Buta B, Xue Q, et al. Interventions for frailty among older adults with cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(5):482–503. https://doi.org/10.1016/j.jacc.2021.11.029.
Lazzeroni D, Villatore A, Souryal G, Pili G, Peretto G. The aging heart: a molecular and clinical challenge. Int J Mol Sci. 2022;23(24):16033. https://doi.org/10.3390/ijms232416033.
Li H, Hastings M, Rhee J, et al. Targeting age-related pathways in heart failure. Circul Res. 2020;126(4):533–51. https://doi.org/10.1161/circresaha.119.315889.
Ribeiro A, Zerolo B, López-Espuela F, Sánchez R, Fernandes V. Cardiac system during the aging process. Aging Dis. 2023;14(4):1105–22. https://doi.org/10.14336/ad.2023.0115.
Chen K, Wang S, Sun Q, et al. Klotho deficiency causes heart aging via impairing the Nrf2-GR pathway. Circul Res. 2021;128(4):492–507. https://doi.org/10.1161/circresaha.120.317348.
de Almeida L, Thode H, Eslambolchi Y, et al. Matrix metalloproteinases: from molecular mechanisms to physiology, pathophysiology, and pharmacology. Pharmacol Rev. 2022;74(3):712–68. https://doi.org/10.1124/pharmrev.121.000349.
Kollarova M, Puzserova A, Balis P, et al. Age- and phenotype-dependent changes in circulating MMP-2 and MMP-9 activities in normotensive and hypertensive rats. Int J Mol Sci. 2020;21(19):7286. https://doi.org/10.3390/ijms21197286.
Yabluchanskiy A, Ma Y, Iyer R, Hall M, Lindsey M. Matrix metalloproteinase-9: many shades of function in cardiovascular disease. Physiology. 2013;28(6):391–403. https://doi.org/10.1152/physiol.00029.2013.
Dowery R, Benhamou D, Benchetrit E, et al. Peripheral B cells repress B-cell regeneration in aging through a TNF-α/IGFBP-1/IGF-1 immune-endocrine axis. Blood. 2021;138(19):1817–29. https://doi.org/10.1182/blood.2021012428.
Gendrisch F, Esser P, Schempp C, Wölfle U. Luteolin as a modulator of skin aging and inflammation. Biofactors. 2021;47(2):170–80. https://doi.org/10.1002/biof.1699.
Padmanabhan Iyer R, Chiao Y, Flynn E, et al. Matrix metalloproteinase-9-dependent mechanisms of reduced contractility and increased stiffness in the aging heart. Proteom Clin Appl. 2016;10(1):92–107. https://doi.org/10.1002/prca.201500038.
Wilkie S, Borland G, Carter R, Morton N, Selman C. Hydrogen sulfide in ageing, longevity and disease. Biochem J. 2021;478(19):3485–504. https://doi.org/10.1042/bcj20210517.
Sokolov A, Nekrasov P, Shaposhnikov M, Moskalev A. Hydrogen sulfide in longevity and pathologies: inconsistency is malodorous. Ageing Res Rev. 2021;67:101262. https://doi.org/10.1016/j.arr.2021.101262.
Llarena N, Hine C. Reproductive longevity and aging: geroscience approaches to maintain long-term ovarian fitness. J Gerontol Series A, Biol Sci Med Sci. 2021;76(9):1551–60. https://doi.org/10.1093/gerona/glaa204.
Blackwood E, Glembotski C. Hydrogen sulfide: the gas that fuels longevity. J Cardiovasc Aging. 2022;2:26. https://doi.org/10.20517/jca.2022.16.
Éva Sikura K, Combi Z, Potor L, et al. Hydrogen sulfide inhibits aortic valve calcification in heart via regulating RUNX2 by NF-κB, a link between inflammation and mineralization. J Adv Res. 2021;27:165–76. https://doi.org/10.1016/j.jare.2020.07.005.
Funding
This study was supported by the National Natural Science Foundation of China (32271155, 91849120, and 31871154), the Natural Science Foundation of Hebei Province of China (C2020206025), and the University level Graduate Innovation Funding Project of Hebei Medical University in 2023 (XCXZZB202303).
Author information
Authors and Affiliations
Contributions
Conceptualization, CXA and YMW; methodology, KCH; software, HXZ; validation, BT, CQS, and ZHL; formal analysis, LXZ; investigation, DYT; resources, LX; data curation, HMX; writing—original draft preparation, QG; writing—review and editing, XT; visualization, SJ; supervision, YMW; project administration, CXA; funding acquisition, YMW All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflicts of Interest
The authors declare no conflict of interest.
Ethics approval
This study was conducted in accordance with the Helsinki Declaration and was approved by the Ethics Committee of Hebei Medical University, No.2018045.
Consent to Participate
All authors are involved and aware of the study.
Consent to Publication
All authors agree to the publication of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
He, K., Zhang, H., Tan, B. et al. Hydrogen Sulfide Ameliorates Heart Aging by Downregulating Matrix Metalloproteinase-9. Cardiovasc Drugs Ther (2024). https://doi.org/10.1007/s10557-024-07586-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-024-07586-w