Abstract
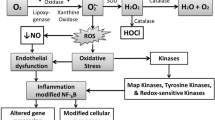
Nowadays, as a type of orderly and active death determined by genes, programmed cell death (PCD), including apoptosis, pyroptosis, ferroptosis, and necroptosis, has attracted much attention owing to its participation in numerous chronic cardiovascular diseases, especially atherosclerosis (AS), a canonical chronic inflammatory disease featured by lipid metabolism disturbance. Abundant researches have reported that PCD under distinct internal conditions fulfills different roles of atherosclerotic pathological processes, including lipid core expansion, leukocyte adhesion, and infiltration. Noteworthy, emerging evidence recently has also suggested that oxidative stress (OS), an imbalance of antioxidants and oxygen free radicals, has the potential to mediate PCD occurrence via multiple ways, including oxidization and deubiquitination. Interestingly, more recently, several studies have proposed that the mediating mechanisms could effect on the atherosclerotic initiation and progression significantly from variable aspects, so it is of great clinical importance to clarify how OS-mediated PCD and AS interact. Herein, with the aim of summarizing potential and sufficient atherosclerotic therapy targets, we seek to provide extensive analysis of the specific regulatory mechanisms of PCD mediated by OS and their multifaceted effects on the entire pathological atherosclerotic progression.



Similar content being viewed by others
References
Libby P. The changing landscape of atherosclerosis. Nature. 2021;592(7855):524–33.
Tabares-Guevara JH, Villa-Pulgarin JA, Hernandez JC. Atherosclerosis: immunopathogenesis and strategies for immunotherapy. Immunotherapy. 2021;13(14):1231–44.
Vallejo J, et al. Heterogeneity of immune cells in human atherosclerosis revealed by scRNA-Seq. Cardiovasc Res. 2021;117(13):2537–43.
Gupta M, et al. Novel emerging therapies in atherosclerosis targeting lipid metabolism. Expert Opin Investig Drugs. 2020;29(6):611–22.
Poznyak AV, et al. Anti-inflammatory therapy for atherosclerosis: focusing on cytokines. Int J Mol Sci. 2021;22(13):7061.
Li M, et al. Programmed cell death in atherosclerosis and vascular calcification. Cell Death Dis. 2022;13(5):467.
He X, et al. Pyroptosis is a critical immune-inflammatory response involved in atherosclerosis. Pharmacol Res. 2021;165:105447.
Shan R, et al. Apoptosis, autophagy and atherosclerosis: relationships and the role of Hsp27. Pharmacol Res. 2021;166:105169.
Chen X, et al. Ferroptosis and cardiovascular disease: role of free radical-induced lipid peroxidation. Free Radic Res. 2021;55(4):405–15.
Zhao Y, et al. ROS-mediated programmed cell death (PCD) of Thalassiosira pseudonana under the stress of BDE-47. Environ Pollut. 2020;262:114342.
Wang L, et al. Oxidative stress in oocyte aging and female reproduction. J Cell Physiol. 2021;236(12):7966–83.
Castellini C, et al. Pathophysiology of mitochondrial dysfunction in human spermatozoa: focus on energetic metabolism, oxidative stress and apoptosis. Antioxidants (Basel). 2021;10(5):695.
Boz Z, et al. N-acetylcysteine prevents olanzapine-induced oxidative stress in mHypoA-59 hypothalamic neurons. Sci Rep. 2020;10(1):19185.
Sun H, et al. Harnessing C/N balance of Chromochloris zofingiensis to overcome the potential conflict in microalgal production. Commun Biol. 2020;3(1):186.
Prasad AS, Bao B. Molecular mechanisms of zinc as a pro-antioxidant mediator: clinical therapeutic implications. Antioxidants (Basel). 2019;8(6):164.
Blanter M, Gouwy M, Struyf S. Studying neutrophil function in vitro: cell models and environmental factors. J Inflamm Res. 2021;14:141–62.
Sharma A, et al. Modulation of Nrf2 by quercetin in doxorubicin-treated rats. Heliyon. 2020;6(4):e03803.
Lee DY, Song MY, and Kim EH. Role of oxidative stress and Nrf2/KEAP1 signaling in colorectal cancer: mechanisms and therapeutic perspectives with phytochemicals. Antioxidants (Basel). 2021;10(5):743.
Franco R, Navarro G, and Martínez-Pinilla E. Antioxidant defense mechanisms in erythrocytes and in the central nervous system. Antioxidants (Basel). 2019;8(2):46.
Li H, et al. Nrf2 deficiency attenuates atherosclerosis by reducing LOX-1-mediated proliferation and migration of vascular smooth muscle cells. Atherosclerosis. 2022;347:1–16.
Ying Z, et al. Lipoicmethylenedioxyphenol reduces experimental atherosclerosis through activation of Nrf2 signaling. PLoS ONE. 2016;11(2):e0148305.
Chen Y, et al. A small molecule NRF2 activator BC-1901S ameliorates inflammation through DCAF1/NRF2 axis. Redox Biol. 2020;32:101485.
Qiao Q, et al. Roles of dietary bioactive peptides in redox balance and metabolic disorders. Oxid Med Cell Longev. 2021;2021:5582245.
Li D, et al. The role of Nrf2 in hearing loss. Front Pharmacol. 2021;12:620921.
Ghanim BY, Qinna NA. Nrf2/ARE axis signalling in hepatocyte cellular death. Mol Biol Rep. 2022;49:4039–53.
Yu X, Li Y, Mu X. Effect of quercetin on PC12 Alzheimer’s disease cell model induced by Aβ (25–35) and its mechanism based on sirtuin1/Nrf2/HO-1 pathway. Biomed Res Int. 2020;2020:8210578.
Zhang Q, et al. Activation of Nrf2/HO-1 signaling: an important molecular mechanism of herbal medicine in the treatment of atherosclerosis via the protection of vascular endothelial cells from oxidative stress. J Adv Res. 2021;34:43–63.
Wang Y, et al. Circular RNAs: novel players in the oxidative stress-mediated pathologies, biomarkers, and therapeutic targets. Oxid Med Cell Longev. 2021;2021:6634601.
Song L, et al. Chinese herbal medicines and active metabolites: potential antioxidant treatments for atherosclerosis. Front Pharmacol. 2021;12:675999.
Buchmann GK, et al. Deletion of NoxO1 limits atherosclerosis development in female mice. Redox Biol. 2020;37:101713.
Trum M, Riechel J, and Wagner S. Cardioprotection by SGLT2 inhibitors-does it all come down to Na(+)? Int J Mol Sci. 2021;22(15):7976.
Trum M, et al. Inhibition of cardiac potassium currents by oxidation-activated protein kinase A contributes to early afterdepolarizations in the heart. Am J Physiol Heart Circ Physiol. 2020;319(6):H1347-h1357.
Matilla AJ. Cellular oxidative stress in programmed cell death: focusing on chloroplastic (1)O(2) and mitochondrial cytochrome-c release. J Plant Res. 2021;134(2):179–94.
Obeng E. Apoptosis (programmed cell death) and its signals - a review. Braz J Biol. 2021;81(4):1133–43.
Goldblatt ZE, Cirka HA, Billiar KL. Mechanical regulation of apoptosis in the cardiovascular system. Ann Biomed Eng. 2021;49(1):75–97.
Dou Z, et al. Aberrant Bcl-x splicing in cancer: from molecular mechanism to therapeutic modulation. J Exp Clin Cancer Res. 2021;40(1):194.
Carneiro BA, El-Deiry WS. Targeting apoptosis in cancer therapy. Nat Rev Clin Oncol. 2020;17(7):395–417.
Cheng Q, et al. Long non-coding RNA LOC285194 regulates vascular smooth muscle cell apoptosis in atherosclerosis. Bioengineered. 2020;11(1):53–60.
Li Q, et al. HRD1 prevents atherosclerosis-mediated endothelial cell apoptosis by promoting LOX-1 degradation. Cell Cycle. 2020;19(12):1466–77.
Zhang N, et al. The regulation of Ero1-alpha in homocysteine-induced macrophage apoptosis and vulnerable plaque formation in atherosclerosis. Atherosclerosis. 2021;334:39–47.
Tawakol A, Abohashem S, Zureigat H. Imaging apoptosis in atherosclerosis: from cell death, a ray of light. J Am Coll Cardiol. 2020;76(16):1875–7.
Liu C, et al. The function, regulation and mechanism of programmed cell death of macrophages in atherosclerosis. Front Cell Dev Biol. 2021;9:809516.
Lin X, et al. Focus on ferroptosis, pyroptosis, apoptosis and autophagy of vascular endothelial cells to the strategic targets for the treatment of atherosclerosis. Arch Biochem Biophys. 2022;715:109098.
Fang S, et al. IRGM/Irgm1 facilitates macrophage apoptosis through ROS generation and MAPK signal transduction: Irgm1(+/-) mice display increases atherosclerotic plaque stability. Theranostics. 2021;11(19):9358–75.
Guo Y, et al. PCSK9 (proprotein convertase subtilisin/Kexin type 9) Triggers vascular smooth muscle cell senescence and apoptosis: implication of its direct role in degenerative vascular disease. Arterioscler Thromb Vasc Biol. 2022;42(1):67–86.
van der Meer IM, et al. Soluble Fas, a mediator of apoptosis, C-reactive protein, and coronary and extracoronary atherosclerosis. The Rotterdam Coronary Calcification Study. Atherosclerosis. 2006;189(2):464–9.
Zadelaar AS, et al. Increased vulnerability of pre-existing atherosclerosis in ApoE-deficient mice following adenovirus-mediated Fas ligand gene transfer. Atherosclerosis. 2005;183(2):244–50.
Patel M, et al. Considerations for analysis of endothelial shear stress and strain in FSI models of atherosclerosis. J Biomech. 2021;128:110720.
Schneider DB, et al. Expression of Fas ligand in arteries of hypercholesterolemic rabbits accelerates atherosclerotic lesion formation. Arterioscler Thromb Vasc Biol. 2000;20(2):298–308.
Pi S, et al. The P2RY12 receptor promotes VSMC-derived foam cell formation by inhibiting autophagy in advanced atherosclerosis. Autophagy. 2021;17(4):980–1000.
Liu J, et al. Reduced macrophage apoptosis is associated with accelerated atherosclerosis in low-density lipoprotein receptor-null mice. Arterioscler Thromb Vasc Biol. 2005;25(1):174–9.
Martinet W, et al. Macrophage death as a pharmacological target in atherosclerosis. Front Pharmacol. 2019;10:306.
Mirzaei S, et al. Elucidating role of reactive oxygen species (ROS) in cisplatin chemotherapy: a focus on molecular pathways and possible therapeutic strategies. Molecules. 2021;26(8):2382.
Mill C, et al. Wnt5a-induced Wnt1-inducible secreted protein-1 suppresses vascular smooth muscle cell apoptosis induced by oxidative stress. Arterioscler Thromb Vasc Biol. 2014;34(11):2449–56.
Zhang Y, et al. Palmitate induces VSMC apoptosis via toll like receptor (TLR)4/ROS/p53 pathway. Atherosclerosis. 2017;263:74–81.
Choi Y, et al. Causal associations between serum bilirubin levels and decreased stroke risk: a two-sample mendelian randomization study. Arterioscler Thromb Vasc Biol. 2020;40(2):437–45.
Geng T, et al. CD137 Signaling promotes endothelial apoptosis by inhibiting Nrf2 pathway, and upregulating NF-κB pathway. Mediators Inflamm. 2020;2020:4321912.
Iyer S, et al. Robust autoactivation for apoptosis by BAK but not BAX highlights BAK as an important therapeutic target. Cell Death Dis. 2020;11(4):268.
Li D, et al. Reactive oxygen species (ROS) control the expression of Bcl-2 family proteins by regulating their phosphorylation and ubiquitination. Cancer Sci. 2004;95(8):644–50.
Luanpitpong S, et al. Mitochondrial superoxide mediates doxorubicin-induced keratinocyte apoptosis through oxidative modification of ERK and Bcl-2 ubiquitination. Biochem Pharmacol. 2012;83(12):1643–54.
Luanpitpong S, et al. Regulation of apoptosis by Bcl-2 cysteine oxidation in human lung epithelial cells. Mol Biol Cell. 2013;24(6):858–69.
Seo J, et al. Necroptosis molecular mechanisms: recent findings regarding novel necroptosis regulators. Exp Mol Med. 2021;53(6):1007–17.
Du J, et al. Icariside II overcomes TRAIL resistance of melanoma cells through ROS-mediated downregulation of STAT3/cFLIP signaling. Oncotarget. 2016;7(32):52218–29.
Robinson N, et al. Programmed necrotic cell death of macrophages: focus on pyroptosis, necroptosis, and parthanatos. Redox Biol. 2019;26:101239.
Liu B, et al. Inflammatory caspases drive pyroptosis in acute lung injury. Front Pharmacol. 2021;12:631256.
Yuan B, et al. Inhibition of AIM2 inflammasome activation alleviates GSDMD-induced pyroptosis in early brain injury after subarachnoid haemorrhage. Cell Death Dis. 2020;11(1):76.
Zhang KJ, et al. Pyroptosis: a new frontier in kidney diseases. Oxid Med Cell Longev. 2021;2021:6686617.
Yu P, et al. Pyroptosis: mechanisms and diseases. Signal Transduct Target Ther. 2021;6(1):128.
Du T, et al. Pyroptosis, metabolism, and tumor immune microenvironment. Clin Transl Med. 2021;11(8):e492.
Xu S, et al. Targeting HDAC6 attenuates nicotine-induced macrophage pyroptosis via NF-κB/NLRP3 pathway. Atherosclerosis. 2021;317:1–9.
Li X, et al. SENP7 knockdown inhibited pyroptosis and NF-κB/NLRP3 inflammasome pathway activation in Raw 264.7 cells. Sci Rep. 2020;10(1):16265.
Wolf D, Ley K. Immunity and inflammation in atherosclerosis. Circ Res. 2019;124(2):315–27.
Zhu X, et al. Potential injurious effects of the fine particulate PM2.5 on the progression of atherosclerosis in apoE-deficient mice by activating platelets and leukocytes. Arch Med Sci. 2019;15(1):250–61.
Abbate A, et al. Interleukin-1 and the inflammasome as therapeutic targets in cardiovascular disease. Circ Res. 2020;126(9):1260–80.
Ridker PM, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31.
Svensson EC, et al. TET2-driven clonal hematopoiesis and response to canakinumab: an exploratory analysis of the CANTOS randomized clinical trial. JAMA Cardiol. 2022;7(5):521–8.
Kirii H, et al. Lack of interleukin-1beta decreases the severity of atherosclerosis in ApoE-deficient mice. Arterioscler Thromb Vasc Biol. 2003;23(4):656–60.
Shi X, et al. Expression of the NLRP3 inflammasome in carotid atherosclerosis. J Stroke Cerebrovasc Dis. 2015;24(11):2455–66.
Niyonzima N, et al. Cholesterol crystals use complement to increase NLRP3 signaling pathways in coronary and carotid atherosclerosis. EBioMedicine. 2020;60:102985.
Duewell P, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464(7293):1357–61.
Sharma A, et al. Specific NLRP3 inhibition protects against diabetes-associated atherosclerosis. Diabetes. 2021;70(3):772–87.
Zheng F, et al. Silence of NLRP3 suppresses atherosclerosis and stabilizes plaques in apolipoprotein E-deficient mice. Mediators Inflamm. 2014;2014:507208.
Li Y, et al. VX-765 attenuates atherosclerosis in ApoE deficient mice by modulating VSMCs pyroptosis. Exp Cell Res. 2020;389(1):111847.
Fidler TP, et al. The AIM2 inflammasome exacerbates atherosclerosis in clonal haematopoiesis. Nature. 2021;592(7853):296–301.
Hakimi M, et al. Inflammation-related induction of absent in melanoma 2 (AIM2) in vascular cells and atherosclerotic lesions suggests a role in vascular pathogenesis. J Vasc Surg. 2014;59(3):794–803.
Menu P, et al. Atherosclerosis in ApoE-deficient mice progresses independently of the NLRP3 inflammasome. Cell Death Dis. 2011;2(3):e137.
Chen S, et al. Sex-specific effects of the Nlrp3 inflammasome on atherogenesis in LDL receptor-deficient mice. JACC Basic Transl Sci. 2020;5(6):582–98.
Kelley N, et al. The NLRP3 inflammasome: an overview of mechanisms of activation and regulation. Int J Mol Sci. 2019;20(13):3328.
Takahashi M. Cell-specific roles of NLRP3 inflammasome in myocardial infarction. J Cardiovasc Pharmacol. 2019;74(3):188–93.
McKee CM, Coll RC. NLRP3 inflammasome priming: a riddle wrapped in a mystery inside an enigma. J Leukoc Biol. 2020;108(3):937–52.
Zhou R, et al. A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469(7329):221–5.
Kim SR, et al. NLRP3 inflammasome activation by mitochondrial ROS in bronchial epithelial cells is required for allergic inflammation. Cell Death Dis. 2014;5(10):e1498.
Lin HC, et al. Cbl negatively regulates NLRP3 inflammasome activation through GLUT1-dependent glycolysis inhibition. Int J Mol Sci. 2020;21(14):5104.
Yu E, et al. Mitochondrial DNA damage can promote atherosclerosis independently of reactive oxygen species through effects on smooth muscle cells and monocytes and correlates with higher-risk plaques in humans. Circulation. 2013;128(7):702–12.
Gray K, et al. Effects of DNA damage in smooth muscle cells in atherosclerosis. Circ Res. 2015;116(5):816–26.
Li S, et al. SFTSV infection induces BAK/BAX-dependent mitochondrial DNA release to trigger NLRP3 inflammasome activation. Cell Rep. 2020;30(13):4370-4385.e7.
Zhong Z, et al. New mitochondrial DNA synthesis enables NLRP3 inflammasome activation. Nature. 2018;560(7717):198–203.
Ding Z, et al. LOX-1, mtDNA damage, and NLRP3 inflammasome activation in macrophages: implications in atherogenesis. Cardiovasc Res. 2014;103(4):619–28.
Tumurkhuu G, et al. Ogg1-dependent DNA repair regulates NLRP3 inflammasome and prevents atherosclerosis. Circ Res. 2016;119(6):e76-90.
Ruan J, Wang S, Wang J. Mechanism and regulation of pyroptosis-mediated in cancer cell death. Chem Biol Interact. 2020;323:109052.
Wang Y, et al. Mitochondrial ROS promote macrophage pyroptosis by inducing GSDMD oxidation. J Mol Cell Biol. 2019;11(12):1069–82.
Raut PK, et al. Growth of breast cancer cells by leptin is mediated via activation of the inflammasome: critical roles of estrogen receptor signaling and reactive oxygen species production. Biochem Pharmacol. 2019;161:73–88.
Juliana C, et al. Non-transcriptional priming and deubiquitination regulate NLRP3 inflammasome activation. J Biol Chem. 2012;287(43):36617–22.
Py BF, et al. Deubiquitination of NLRP3 by BRCC3 critically regulates inflammasome activity. Mol Cell. 2013;49(2):331–8.
Lopez-Castejon G, et al. Deubiquitinases regulate the activity of caspase-1 and interleukin-1β secretion via assembly of the inflammasome. J Biol Chem. 2013;288(4):2721–33.
Hu B, et al. The DNA-sensing AIM2 inflammasome controls radiation-induced cell death and tissue injury. Science. 2016;354(6313):765–8.
Chen ML et al. Trimethylamine-N-oxide induces vascular inflammation by activating the NLRP3 inflammasome through the SIRT3-SOD2-mtROS signaling pathway. J Am Heart Assoc. 2017;6(9):e006347.
Chen H, et al. Cadmium induces NLRP3 inflammasome-dependent pyroptosis in vascular endothelial cells. Toxicol Lett. 2016;246:7–16.
Dixon SJ, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72.
Leng Y, et al. Ferroptosis: a potential target in cardiovascular disease. Front Cell Dev Biol. 2021;9:813668.
Lee H, et al. Energy-stress-mediated AMPK activation inhibits ferroptosis. Nat Cell Biol. 2020;22(2):225–34.
Ng SW, Norwitz SG, Norwitz ER. The impact of iron overload and ferroptosis on reproductive disorders in humans: implications for preeclampsia. Int J Mol Sci. 2019;20(13):3283.
Chen J, et al. The multifaceted role of ferroptosis in liver disease. Cell Death Differ. 2022;29(3):467–80.
Conrad M, Pratt DA. The chemical basis of ferroptosis. Nat Chem Biol. 2019;15(12):1137–47.
Liang C, et al. Recent progress in ferroptosis inducers for cancer therapy. Adv Mater. 2019;31(51):e1904197.
Qian ZM, Ke Y. Hepcidin and its therapeutic potential in neurodegenerative disorders. Med Res Rev. 2020;40(2):633–53.
Beatty A, et al. Ferroptotic cell death triggered by conjugated linolenic acids is mediated by ACSL1. Nat Commun. 2021;12(1):2244.
Zeya B, Chandra NC. LOX-1: Its cytotopographical variance and disease stress. J Biochem Mol Toxicol. 2019;33(9):e22375.
Bai T, et al. Inhibition of ferroptosis alleviates atherosclerosis through attenuating lipid peroxidation and endothelial dysfunction in mouse aortic endothelial cell. Free Radic Biol Med. 2020;160:92–102.
Muri J, et al. B1 and marginal zone B cells but not follicular B2 cells require Gpx4 to prevent lipid peroxidation and ferroptosis. Cell Rep. 2019;29(9):2731-2744.e4.
Guo Z, et al. Suppression of atherogenesis by overexpression of glutathione peroxidase-4 in apolipoprotein E-deficient mice. Free Radic Biol Med. 2008;44(3):343–52.
Mathew OP, Ranganna K, Milton SG. Involvement of the antioxidant effect and anti-inflammatory response in butyrate-inhibited vascular smooth muscle cell proliferation. Pharmaceuticals (Basel). 2014;7(11):1008–27.
Naito Y, et al. Crosstalk between iron and arteriosclerosis. J Atheroscler Thromb. 2022;29(3):308–14.
Vinchi F, et al. Atherosclerosis is aggravated by iron overload and ameliorated by dietary and pharmacological iron restriction. Eur Heart J. 2020;41(28):2681–95.
Zhang M, et al. Effect of tetramethylpyrazine and hyperlipidemia on hepcidin homeostasis in mice. Int J Mol Med. 2019;43(1):501–6.
Malhotra R, et al. Hepcidin deficiency protects against atherosclerosis. Arterioscler Thromb Vasc Biol. 2019;39(2):178–87.
Saeed O, et al. Pharmacological suppression of hepcidin increases macrophage cholesterol efflux and reduces foam cell formation and atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32(2):299–307.
Shah R, Shchepinov MS, Pratt DA. Resolving the role of lipoxygenases in the initiation and execution of ferroptosis. ACS Cent Sci. 2018;4(3):387–96.
Li C, et al. CTRP5 promotes transcytosis and oxidative modification of low-density lipoprotein and the development of atherosclerosis. Atherosclerosis. 2018;278:197–209.
Sampilvanjil A, et al. Cigarette smoke extract induces ferroptosis in vascular smooth muscle cells. Am J Physiol Heart Circ Physiol. 2020;318(3):H508-h518.
Yu B, et al. Magnetic field boosted ferroptosis-like cell death and responsive MRI using hybrid vesicles for cancer immunotherapy. Nat Commun. 2020;11(1):3637.
Wang C, et al. Fenton-like reaction of the iron(II)-histidine complex generates hydroxyl radicals: implications for oxidative stress and Alzheimer’s disease. Chem Commun (Camb). 2021;57(92):12293–6.
Samet JM, et al. Non-redox cycling mechanisms of oxidative stress induced by PM metals. Free Radic Biol Med. 2020;151:26–37.
Singh N, Bhatla SC. Heme oxygenase-nitric oxide crosstalk-mediated iron homeostasis in plants under oxidative stress. Free Radic Biol Med. 2022;182:192–205.
Marques VB, et al. Chronic iron overload intensifies atherosclerosis in apolipoprotein E deficient mice: role of oxidative stress and endothelial dysfunction. Life Sci. 2019;233:116702.
Xu S. Iron and atherosclerosis: the link revisited. Trends Mol Med. 2019;25(8):659–61.
Chen GH, et al. Mitochondrial oxidative stress mediated Fe-induced ferroptosis via the NRF2-ARE pathway. Free Radic Biol Med. 2022;180:95–107.
Li X, et al. A narrative review of the role of necroptosis in liver disease: a double-edged sword. Ann Transl Med. 2021;9(5):422.
Speir M, et al. Targeting RIP kinases in chronic inflammatory disease. Biomolecules. 2021;11(5):646.
Yan J, et al. Necroptosis and tumor progression. Trends Cancer. 2022;8(1):21–7.
Zhou Y, et al. Insight into crosstalk between ferroptosis and necroptosis: novel therapeutics in ischemic stroke. Oxid Med Cell Longev. 2021;2021:9991001.
Yu Z, et al. Necroptosis: a novel pathway in neuroinflammation. Front Pharmacol. 2021;12:701564.
Wang H, et al. Mixed lineage kinase domain-like protein MLKL causes necrotic membrane disruption upon phosphorylation by RIP3. Mol Cell. 2014;54(1):133–46.
Orozco S, et al. RIPK1 both positively and negatively regulates RIPK3 oligomerization and necroptosis. Cell Death Differ. 2014;21(10):1511–21.
Bertheloot D, Latz E, Franklin BS. Necroptosis, pyroptosis and apoptosis: an intricate game of cell death. Cell Mol Immunol. 2021;18(5):1106–21.
Chen J, et al. Molecular insights into the mechanism of necroptosis: the necrosome as a potential therapeutic target. Cells. 2019;8(12):1486.
Kattoor AJ, Kanuri SH, Mehta JL. Role of Ox-LDL and LOX-1 in atherogenesis. Curr Med Chem. 2019;26(9):1693–700.
Karunakaran D, et al. Targeting macrophage necroptosis for therapeutic and diagnostic interventions in atherosclerosis. Sci Adv. 2016;2(7):e1600224.
Leeper NJ. The role of necroptosis in atherosclerotic disease. JACC Basic Transl Sci. 2016;1(6):548–50.
Lin J, et al. A role of RIP3-mediated macrophage necrosis in atherosclerosis development. Cell Rep. 2013;3(1):200–10.
Meng L, et al. RIP3-dependent necrosis induced inflammation exacerbates atherosclerosis. Biochem Biophys Res Commun. 2016;473(2):497–502.
Karunakaran D, et al. RIPK1 expression associates with inflammation in early atherosclerosis in humans and can be therapeutically silenced to reduce NF-κB activation and atherogenesis in mice. Circulation. 2021;143(2):163–77.
Rasheed A, et al. Loss of MLKL (mixed lineage kinase domain-like protein) decreases necrotic core but increases macrophage lipid accumulation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2020;40(5):1155–67.
Zhang Y, et al. RIP1 autophosphorylation is promoted by mitochondrial ROS and is essential for RIP3 recruitment into necrosome. Nat Commun. 2017;8:14329.
Zhu P, et al. Ripk3 promotes ER stress-induced necroptosis in cardiac IR injury: a mechanism involving calcium overload/XO/ROS/mPTP pathway. Redox Biol. 2018;16:157–68.
Hsu SK, et al. The role of necroptosis in ROS-mediated cancer therapies and its promising applications. Cancers (Basel). 2020;12(8):2185.
Lu B, et al. Shikonin induces glioma cell necroptosis in vitro by ROS overproduction and promoting RIP1/RIP3 necrosome formation. Acta Pharmacol Sin. 2017;38(11):1543–53.
Tang Q, et al. Bim- and Bax-mediated mitochondrial pathway dominates abivertinib-induced apoptosis and ferroptosis. Free Radic Biol Med. 2022;180:198–209.
Wang F, et al. Neuregulin-1 alleviate oxidative stress and mitigate inflammation by suppressing NOX4 and NLRP3/caspase-1 in myocardial ischaemia-reperfusion injury. J Cell Mol Med. 2021;25(3):1783–95.
Masuyama A, et al. Defective autophagy in vascular smooth muscle cells enhances atherosclerotic plaque instability. Biochem Biophys Res Commun. 2018;505(4):1141–7.
Vion AC, et al. Autophagy is required for endothelial cell alignment and atheroprotection under physiological blood flow. Proc Natl Acad Sci U S A. 2017;114(41):E8675-e8684.
Cai X, et al. GLP-1 treatment protects endothelial cells from oxidative stress-induced autophagy and endothelial dysfunction. Int J Biol Sci. 2018;14(12):1696–708.
Ge P, et al. Downregulation of microRNA-512-3p enhances the viability and suppresses the apoptosis of vascular endothelial cells, alleviates autophagy and endoplasmic reticulum stress as well as represses atherosclerotic lesions in atherosclerosis by adjusting spliced/unspliced ratio of X-box binding protein 1 (XBP-1S/XBP-1U). Bioengineered. 2021;12(2):12469–81.
Martínez GJ, Celermajer DS, Patel S. The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosis-associated inflammation. Atherosclerosis. 2018;269:262–71.
Yang M, et al. Colchicine alleviates cholesterol crystal-induced endothelial cell pyroptosis through activating AMPK/SIRT1 pathway. Oxid Med Cell Longev. 2020;2020:9173530.
Parsamanesh N, et al. NLRP3 inflammasome as a treatment target in atherosclerosis: a focus on statin therapy. Int Immunopharmacol. 2019;73:146–55.
Mollazadeh H, et al. Effects of statins on mitochondrial pathways. J Cachexia Sarcopenia Muscle. 2021;12(2):237–51.
Yang L, et al. Dapagliflozin attenuates cholesterol overloading-induced injury in mice hepatocytes with type 2 diabetes mellitus (T2DM) via eliminating oxidative damages. Cell Cycle. 2022;21(6):641–54.
Funding
This research is supported by the National Natural Science Foundation of China (No. 82061130223 and No. 82072031), HMU Marshal Initiative Funding (HMUMIF-21016), and Fund of Key Laboratory of Myocardial Ischemia, Ministry of Education (KF202020/LX).
Author information
Authors and Affiliations
Contributions
Y. C., X. L, X.B., and. B.X.: conceptualization and writing; H. J. and B. Y.: review and editing.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All the authors have given their approval for this manuscript to be published.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Luo, X., Xu, B. et al. Oxidative Stress-Mediated Programmed Cell Death: a Potential Therapy Target for Atherosclerosis. Cardiovasc Drugs Ther (2022). https://doi.org/10.1007/s10557-022-07414-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-022-07414-z