Abstract
Purpose
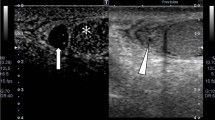
Testicular torsion requires emergency surgery; thus, prompt and correct diagnosis is very important. Ultrasound with color Doppler is usually the first-choice modality for diagnosis; however, skill and experience are required for confident diagnosis. Recently, contrast-enhanced ultrasound for the diagnosis of testicular torsion has been reported, but there have been only a few reports. This study aimed to compare contrast-enhanced ultrasound findings in cases of testicular torsion and non-testicular torsion.
Methods
Patients who underwent contrast-enhanced ultrasound for acute scrotum at our institution between April 2010 and January 2023 were divided into testicular torsion (n = 17) and non-testicular torsion (n = 16) groups. The respective contrast-enhanced ultrasound findings were retrospectively examined and compared.
Results
In 16 out of 17 cases of testicular torsion, the parenchyma of the affected testis was not enhanced. In the remaining case, reduced contrast enhancement was observed; however, it was still notably less than that observed on the unaffected testis. On the other hand, in all cases of non-testicular torsion (n = 16), the parenchyma of the affected testis was notably enhanced.
Conclusion
Contrast-enhanced ultrasound is considered an easy and accurate method for diagnosing testicular torsion.

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Günther P, Rübben I. The acute scrotum in childhood and adolescence. Dtsch Arztebl Int. 2012;109:449–57 (quiz 458).
Bandarkar AN, Blask AR. Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis. Pediatr Radiol. 2018;48:735–44.
Laher A, Ragavan S, Mehta P, et al. Testicular torsion in the emergency room: a review of detection and management strategies. Open Access Emerg Med. 2020;12:237–46.
Schellhaas B, Strobel D. Tips and tricks in contrast-enhanced ultrasound (CEUS) for the characterization and detection of liver malignancies. Ultraschall Med. 2019;40:404–24.
Omoto K, Matsunaga H, Take N, et al. Sentinel node detection method using contrast-enhanced ultrasonography with sonazoid in breast cancer: preliminary clinical study. Ultrasound Med Biol. 2009;35:1249–56.
Valentino M, Bertolotto M, Derchi L, et al. Role of contrast enhanced ultrasound in acute scrotal diseases. Eur Radiol. 2011;21:1831–40.
Zou B, Zeng F, Yang Y. Using contrast-enhanced ultrasonography to assess the degree of acute testicular torsion: a case series. BMC Med Imaging. 2022;22:220.
Maruyama H, Ishibashi H, Takahashi M, et al. Effect of signal intensity from the accumulated microbubbles in the liver for differentiation of idiopathic portal hypertension from liver cirrhosis. Radiology. 2009;252:587–94.
Maruyama H, Takahashi M, Ishibashi H, et al. Ultrasound-guided treatments under low acoustic power contrast harmonic imaging for hepatocellular carcinomas undetected by B-mode ultrasonography. Liver Int. 2009;29:708–14.
Dogra VS, Gottlieb RH, Oka M, et al. Sonography of the scrotum. Radiology. 2003;227:18–36.
Nebot CS, Salvador RL, Aliaga SP, et al. Perinatal testicular torsion: ultrasound assessment and differential diagnosis. Radiologia. 2017;59:391–400.
Lee YS, Kim MJ, Han SW, et al. Superb microvascular imaging for the detection of parenchymal perfusion in normal and undescended testes in young children. Eur J Radiol. 2016;85:649–56.
Visalli C, Vinci SL, Mondello S, et al. Microvascular imaging ultrasound (MicroV) and power Doppler vascularization analysis in a pediatric population with early scrotal pain onset. Jpn J Radiol. 2022;40:192–201.
Claudon M, Cosgrove D, Albrecht T, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—update 2008. Ultraschall Med. 2008;29:28–44.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
HF drafted the manuscript. NM performed the ultrasound examinations. MO and YT supervised the writing of the manuscript. HF, MO, YT, and AW evaluated the echo images.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of the Japanese Red Cross Society Himeji Hospital (No. 2022–22). Informed consent was obtained from all patients. All patients consented to the publication of their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Fukuzawa, H., Minoda, N., Okamoto, M. et al. Contrast-enhanced ultrasound findings in testicular torsion and non-testicular torsion. J Med Ultrasonics 51, 133–138 (2024). https://doi.org/10.1007/s10396-023-01384-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-023-01384-x