Abstract
Objective
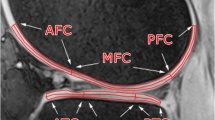
To develop and validate a 3D registration approach by which double echo steady state (DESS) MR images with cartilage thickness segmentations are used to extract the cartilage transverse relaxation time (T2) from multi-echo-spin-echo (MESE) MR images, without direct segmentations for MESE.
Materials and methods
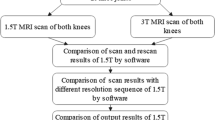
Manual DESS segmentations of 89 healthy reference knees (healthy) and 60 knees with early radiographic osteoarthritis (early ROA) from the Osteoarthritis Initiative were registered to corresponding MESE images that had independent direct T2 segmentations. For validation purposes, (a) regression analysis of deep and superficial cartilage T2 was performed and (b) between-group differences between healthy vs. early ROA knees were compared for registered vs. direct MESE analysis.
Results
Moderate to high correlations were observed for the deep (r = 0.80) and the superficial T2 (r = 0.81), with statistically significant between-group differences (ROA vs. healthy) of + 1.4 ms (p = 0.002) vs. + 1.3 ms (p < 0.001) for registered vs. direct T2 segmentation in the deep, and + 1.3 ms (p = 0.002) vs. + 2.3 ms (p < 0.001) in the superficial layer.
Discussion
This registration approach enables extracting cartilage T2 from MESE scans using DESS (cartilage thickness) segmentations, avoiding the need for direct MESE T2 segmentations.




Similar content being viewed by others
References
Mosher TJ, Dardzinski BJ (2004) Cartilage MRI T2 relaxation time map**: overview and applications. Semin Musculoskelet Radiol 8:355–368
Jungmann PM, Kraus MS, Nardo L, Liebl H, Alizai H, Joseph GB, Liu F, Lynch J, McCulloch CE, Nevitt MC, Link TM (2013) T2 relaxation time measurements are limited in monitoring progression, once advanced cartilage defects at the knee occur: longitudinal data from the osteoarthritis initiative. J Magn Reson 38:1415–1424
Liess C, Luesse S, Karger N, Heller M, Glueer CC (2002) Detection of changes in cartilage water content using MRI T2-map** in vivo. Osteoarthritis Cartilage 10:907–913
Kim T, Min BH, Yoon SH, Kim H, Park S, Lee HY, Kwack KS (2014) An in vitro comparative study of T2 and T2* map**s of human articular cartilage at 3-Tesla MRI using histology as the standard of reference. Skelet Radiol 43:947–954
Lammentausta E, Kiviranta P, Nissi MJ, Laasanen MS, Kiviranta I, Nieminen MT, Jurvelin JS (2006) T2 relaxation time and delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) of human patellar cartilage at 1.5 T and 9.4 T: Relationships with tissue mechanical properties. JOrthopRes 24:366–374
Liebl H, Joseph G, Nevitt MC, Singh N, Heilmeier U, Subburaj K, Jungmann PM, McCulloch CE, Lynch JA, Lane NE, Link TM (2015) Early T2 changes predict onset of radiographic knee osteoarthritis: data from the osteoarthritis initiative. AnnRheum Dis 74:1353–1359
Prasad AP, Nardo L, Schooler J, Joseph GB, Link TM (2013) T(1)rho and T(2) relaxation times predict progression of knee osteoarthritis. Osteoarthr Cart 21:69–76
Wirth W, Maschek S, Beringer P, Eckstein F (2017) Subregional laminar cartilage MR spin-spin relaxation times (T2) in osteoarthritic knees with and without medial femorotibial cartilage loss - data from the osteoarthritis initiative (OAI). Osteoarthr Cartil 25:1313–1323
Eckstein F, Le Graverand MP, Charles HC, Hunter DJ, Kraus VB, Sunyer T, Nemirovskyi O, Wyman BT, Buck R (2011) Clinical, radiographic, molecular and MRI-based predictors of cartilage loss in knee osteoarthritis. Ann Rheum Dis 70:1223–1230
Dardzinski BJ, Mosher TJ, Li S, Van Slyke MA, Smith MB (1997) Spatial variation of T2 in human articular cartilage. Radiology 205:546–550
Wirth W, Maschek S, Roemer FW, Sharma L, Duda GN, Eckstein F (2019) Radiographically normal knees with contralateral joint space narrowing display greater change in cartilage transverse relaxation time than those with normal contralateral knees: a model of early OA?—data from the Osteoarthritis Initiative (OAI). Osteoarthr Cartil 27:1663–1668
Wirth W, Maschek S, Eckstein F (2017) Sex- and age-dependence of region- and layer-specific knee cartilage composition (spin–spin–relaxation time) in healthy reference subjects. Ann Anat Anat Anzeiger 210:1–8
Wirth W, Maschek S, Roemer FW, Eckstein F (2016) Layer-specific femorotibial cartilage T2 relaxation time in knees with and without early knee osteoarthritis: data from the osteoarthritis initiative (OAI). Sci Rep 6:34202
Chaudhari AS, Kogan F, Pedoia V, Majumdar S, Gold GE, Hargreaves BA (2019) Rapid knee MRI acquisition and analysis techniques for imaging osteoarthritis. J Magn Reson Imaging. https://doi.org/10.1002/jmri.26991
Eckstein F, Kwoh CK, Link TM (2014) Imaging research results from the osteoarthritis initiative (OAI): a review and lessons learned 10 years after start of enrolment. Ann Rheum Dis 73:1289–1300
Graichen H, Eisenhart-Rothe RV, Vogl T, Englmeier KH, Eckstein F (2004) Quantitative assessment of cartilage status in osteoarthritis by quantitative magnetic resonance imaging: technical validation for use in analysis of cartilage volume and further morphologic parameters. Arthritis Rheum 50:811–816
Schneider E, Nevitt M, McCulloch C, Cicuttini FM, Duryea J, Eckstein F, Tamez-Pena J (2012) Equivalence and precision of knee cartilage morphometry between different segmentation teams, cartilage regions, and MR acquisitions. Osteoarthritis Cartilage 20:869–879
Gold GE, Han E, Stainsby J, Wright G, Brittain J, Beaulieu C (2004) Musculoskeletal MRI at 3.0 T: Relaxation times and image contrast. Am J Roentgenol. https://doi.org/10.2214/ajr.183.2.1830343
Eckstein F, Kunz M, Schutzer M, Hudelmaier M, Jackson RD, Yu J, Eaton CB, Schneider E (2007) Brief report 2 year longitudinal change and testeretest-precision of knee cartilage morphology in a pilot study for the osteoarthritis initiative 1, 2. Osteoarthr Cart 15:1326–1332
Wirth W, Nevitt M, Hellio Le Graverand MP, Benichou O, Dreher D, Davies RY, Lee J, Picha K, Gimona A, Maschek S, Hudelmaier M, Eckstein F (2010) Sensitivity to change of cartilage morphometry using coronal FLASH, sagittal DESS, and coronal MPR DESS protocols–comparative data from the osteoarthritis initiative (OAI). OsteoarthritisCartilage 18:547–554
Wirth W, Eckstein F, Boeth H, Diederichs G, Hudelmaier M, Duda GNN (2014) Longitudinal analysis of MR spin–spin relaxation times (T2) in medial femorotibial cartilage of adolescent vs mature athletes: dependence of deep and superficial zone properties on sex and age. Osteoarthr Cartil 22:1554–1558
Urish KL, Williams AA, Durkin JR, Chu CR (2013) Registration of magnetic resonance image series for knee articular cartilage analysis: data from the osteoarthritis initiative. Cartilage 4:20–27
Johnson HJ, McCormick MM, Ibanez L (2015) The ITK software guide: design and functionality, Fourth Ed. Kitware Inc.
Pluim JPW, Maintz JBAA, Viergever MA (2003) Mutual-information-based registration of medical images: a survey. IEEE Trans Med Imaging. https://doi.org/10.1109/TMI.2003.815867
Peterfy CG, Schneider E, Nevitt M (2008) The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthr Cartil 16:1433–1441
Eckstein F, Boudreau RM, Wang Z, Hannon MJ, Wirth W, Cotofana S, Guermazi A, Roemer FW, Nevitt M, John MR, Ladel C, Sharma L, Hunter DJ, Kwoh CK (2014) Trajectory of cartilage loss within 4 years of knee replacement—a nested case-control study from the osteoarthritis initiative. Osteoarthr Cartil 22:1542–1549
Eckstein F, Collins JE, Nevitt MC, Lynch JA, Kraus V, Katz JN, Losina E, Wirth W, Guermazi A, Roemer FW, Hunter DJ (2015) Cartilage thickness change as an imaging biomarker of knee osteoarthritis progression—data from the fnih OA biomarkers consortium. Arthritis Rheumatol (Hoboken, NJ) 67:3184–3189
Wirth W, Hunter DJ, Nevitt MC, Sharma L, Kwoh CK, Ladel C, Eckstein F (2017) Predictive and concurrent validity of cartilage thickness change as a marker of knee osteoarthritis progression: data from the osteoarthritis initiative. Osteoarthr Cartil 25:2063–2071
Eckstein F, Maschek S, Roemer FW, Duda GN, Sharma L, Wirth W (2019) Cartilage loss in radiographically normal knees depends on radiographic status of the contralateral knee—data from the osteoarthritis initiative. Osteoarthr Cartil 27:273–277
Frobell RB, Nevitt MC, Hudelmaier M, Wirth W, Wyman BT, Benichou O, Dreher D, Davies R, Lee JH, Baribaud F, Gimona A, Eckstein F (2010) Femorotibial subchondral bone area and regional cartilage thickness: a cross-sectional description in healthy reference cases and various radiographic stages of osteoarthritis in 1003 knees from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 62:1612–1623
Chaudhari AS, Black MS, Eijgenraam S, Wirth W, Maschek S, Sveinsson B, Eckstein F, Oei EHG, Gold GE, Hargreaves BA (2018) Five-minute knee MRI for simultaneous morphometry and T2 relaxometry of cartilage and meniscus and for semiquantitative radiological assessment using double-echo in steady-state at 3T. J Magn Reson Imaging 47:1328–1341
Chaudhari AS, Stevens KJ, Sveinsson B, Wood JP, Beaulieu CF, Oei EHG, Rosenberg JK, Kogan F, Alley MT, Gold GE, Hargreaves BA (2019) Combined 5-minute double-echo in steady-state with separated echoes and 2-minute proton-density-weighted 2D FSE sequence for comprehensive whole-joint knee MRI assessment. J Magn Reson Imaging. https://doi.org/10.1002/jmri.26582
Eijgenraam SM, Chaudhari AS, Reijman M, Bierma-Zeinstra SMA, Hargreaves BA, Runhaar J, Heijboer FWJ, Gold GE, Oei EHG (2019) Time-saving opportunities in knee osteoarthritis: T2 map** and structural imaging of the knee using a single 5-min MRI scan. Eur Radiol. https://doi.org/10.1007/s00330-019-06542-9
Fripp J, Crozier S, Warfield SK, Ourselin S (2007) Automatic segmentation of the bone and extraction of the bone-cartilage interface from magnetic resonance images of the knee. Phys Med Biol. https://doi.org/10.1088/0031-9155/52/6/005
Shan L, Zach C, Charles C, Niethammer M (2014) Automatic atlas-based three-label cartilage segmentation from MR knee images. Med Image Anal. https://doi.org/10.1016/j.media.2014.05.008
Lee HS, Kim HA, Kim H, Hong H, Yoon YC, Kim J (2016) Multi-atlas segmentation of the cartilage in knee MR images with sequential volume- and bone-mask-based registrations. Med Imaging 2016 Comput Diagnosis 10(1117/12):2216630
Raj A, Vishwanathan S, Ajani B, Krishnan K, Agarwal H (2018) Automatic knee cartilage segmentation using fully volumetric convolutional neural networks for evaluation of osteoarthritis. Proc Int Symp Biomed Imaging. https://doi.org/10.1109/ISBI.2018.8363705
Tack A, Mukhopadhyay A, Zachow S (2018) Knee menisci segmentation using convolutional neural networks: data from the Osteoarthritis Initiative. Osteoarthr Cartil. https://doi.org/10.1016/j.joca.2018.02.907
Liu F, Zhou Z, Samsonov A, Blankenbaker D, Larison W, Kanarek A, Lian K, Kambhampati S, Kijowski R (2018) Deep learning approach for evaluating knee MR images: achieving high diagnostic performance for cartilage lesion detection. Radiology. https://doi.org/10.1148/radiol.2018172986
Acknowledgements
We would like to thank the Ludwig Bolzmann Gesellschaft for funding this study and would like to thank the OAI participants, OAI study investigators, and OAI Clinical Center staff for generating this publicly available image sets.
Funding
This work was funded by the Ludwig Boltzmann Institute for Arthritis and Rehabilitation, Austria. The MRI acquisition of data used in this analysis was funded by the Osteoarthritis Initiative, a public–private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the Osteoarthritis Initiative study Investigators. Private funding partners of the OAI include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer, Inc. Private-sector funding for the Osteoarthritis Initiative is managed by the Foundation for the National Institutes of Health. The sponsors were not involved in the design and conduct of this particular study, in the analysis and interpretation of the data, and in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
Fürst: Study conception and design, Acquisition of data, Analysis and interpretation of data, Drafting of the manuscript; Wirth: Analysis and interpretation of data, Drafting of the manuscript, Critical revision; Chaudhari: Analysis and interpretation of data, Drafting of the manuscript, Critical revision; Eckstein: Study conception and design, Analysis and interpretation of data, Drafting of the manuscript, Critical revision.
Corresponding author
Ethics declarations
Conflict of interest
David Fürst and Wolfgang Wirth have a part-time employment with Chondrometrics GmbH; Wolfgang Wirth is a co-owner of Chondrometrics GmbH and has provided consulting services to Galapagos. Felix Eckstein is CEO of Chondrometrics GmbH, a company providing MR image analysis services to academic researchers and industry. He has provided consulting services to Merck KGaA, Abbvie, Tissuegene, Servier, Roche, Galapagos, and Novartis. Akshay Chaudhari has provided consulting services to SkopeMR, Inc., Subtle Medical, Chondrometrics GmbH, Image Analysis Group, and Culvert Engineering; and is a shareholder of Subtle Medical, LVIS Corporation, and BrainKey Inc.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the OAI.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fürst, D., Wirth, W., Chaudhari, A. et al. Layer-specific analysis of femorotibial cartilage t2 relaxation time based on registration of segmented double echo steady state (dess) to multi-echo-spin-echo (mese) images. Magn Reson Mater Phy 33, 819–828 (2020). https://doi.org/10.1007/s10334-020-00852-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-020-00852-6