Abstract
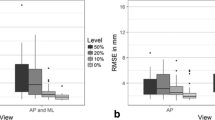
Background: Orthopedic trauma care relies on two-dimensional radiograms both before and during the operation. Understanding the three-dimensional nature of complex fractures on plain radiograms is challenging. Modern fluoroscopes can acquire three-dimensional volume datasets even during an operation, but the device limitations constrain the acquired volume to a cube of only 12-cm edge. However, viewing the surrounding intact structures is important to comprehend the fracture in its context. We suggest merging a fluoroscope’s volume scan into a generic bone model to form a composite full-length 3D bone model. Methods: Materials consisted of one cadaver bone and 20 three-dimensional surface models of human femora. Radiograms and computed tomography scans were taken before and after applying a controlled fracture to the bone. A 3D scan of the fracture was acquired using a mobile fluoroscope (Siemens Siremobil). The fracture was fitted into the generic bone models by rigid registration using a modified least-squares algorithm. Registration precision was determined and a clinical appraisal of the composite models obtained. Results: Twenty composite bone models were generated. Average registration precision was 2.0 mm (range 1.6 to 2.6). Average processing time on a laptop computer was 35 s (range 20 to 55). Comparing synthesized radiograms with the actual radiograms of the fractured bone yielded clinically satisfactory results. Conclusion: A three-dimensional full-length representation of a fractured bone can reliably be synthesized from a short scan of the patient’s fracture and a generic bone model. This patient-specific model can subsequently be used for teaching, surgical operation planning, and intraoperative visualization purposes.






Similar content being viewed by others
References
Müller KH, Strosche H, Scheuer I: Plate osteosynthesis in posttraumatic deformities of the femoral shaft. Arch Orthop Trauma Surg 103:303–319, 1984
Rüedi TP, Buckley RE, Moran CG: AO Principles of Fracture Management, Second expanded edition (2007), Stuttgart: Thieme, 2006
Messmer P, Long G, Suhm N, Hehli M, Wirth J, Regazzoni P, Jacob AL: Three-dimensional fracture simulation for preoperative planning and education. Eur J Trauma 27:171–177, 2001
Kotsianos D, Wirth S, Fischer T, Euler E, Rock C, Linsenmaier U, Pfeifer KJ, Reiser M: 3D imaging with an isocentric mobile C-arm comparison of image quality with spiral CT. Eur Radiol 14:1590–1595, 2004
Wirth S, Euler E, Linsenmaier U, Heining SM, Kotsianos D, Pfeifer KJ, Mutschler W, Reiser M: C-arm-based mobile computed tomography: a comparison with established imaging on the basis of simulated treatments of talus neck fractures in a cadaveric study. Comput Aided Surg 9:27–38, 2004
Richter M, Geerling J, Zech S, Goesling T, Krettek C: Intraoperative three-dimensional imaging with a motorized mobile C-arm (SIREMOBIL ISO-C-3D) in foot and ankle trauma care: a preliminary report. J Orthop Trauma 19:259–266, 2005
Messmer P, Matthews F, Jacob AL, Kikinis R, Regazzoni P, Noser H: A CT database for research, development and education: concept and potential. J Digit Imaging 20:17–22, 2007
Messmer P, Matthews F, Wullschleger C, Huegli R, Regazzoni P, Jacob AL: Image fusion for intraoperative control of axis in long bone fracture treatment. Eur J Trauma 6:555–561, 2006
Lorensen WE, Cline HE: Marching cubes: a high resolution 3D surface construction algorithm. Comput Graph 21:163–169 1987
Besl PJ, McKay ND: A method for registration of 3-D shapes. IEEE Trans Pattern Anal Mach Intell 14:239–255, 1992
Estepar RSJ, Brun A, Westin CF: Robust generalized total least squares iterative closest point registration. MICCAI, LNCS 3216:234–241, 2004
Urquhart DM, Edwards ER, Graves SE, Williamson OD, McNeil JJ, Kossmann T, Richardson MD, Harrison DJ, Hart MJ, Cicuttini FM: Characterisation of orthopaedic trauma admitted to adult level 1 trauma centres. Injury 37:120–127, 2006
Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H: Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury 28 Suppl 1:A31–A41, 1997
Marschollek M, Teistler M, Bott OJ, Stuermer KM, Pretschner DP, Dresing K: Pre-operative dynamic interactive exploration of complex articular fractures using a novel 3D navigation tool. Methods Inf Med 45:384–388, 2006
Rieger M, Gabl M, Gruber H, Jaschke WR, Mallouhi A: CT virtual reality in the preoperative workup of malunited distal radius fractures: preliminary results. Eur Radiol 15:792–797, 2005
Wicky S, Blaser PF, Blanc CH, Leyvraz PF, Schnyder P, Meuli RA: Comparison between standard radiography and spiral CT with 3D reconstruction in the evaluation, classification and management of tibial plateau fractures. Eur Radiol 10:1227–1232, 2000
Woolson ST, Dev P, Fellingham LL, Vassiliadis A: Three-dimensional imaging of bone from computerized tomography. Clin Orthop Relat Res:239–248, 1986
Doornberg J, Lindenhovius A, Kloen P, van Dijk CN, Zurakowski D, Ring D: Two and three-dimensional computed tomography for the classification and management of distal humeral fractures. Evaluation of reliability and diagnostic accuracy. J Bone Joint Surg Am 88:1795–1801, 2006
Braten M, Tveit K, Junk S, Aamodt A, Anda S, Terjesen T: The role of fluoroscopy in avoiding rotational deformity of treated femoral shaft fractures: an anatomical and clinical study. Injury 31:311–315, 2000
Heiland M, Schmelzle R, Hebecker A, Schulze D: Intraoperative 3D imaging of the facial skeleton using the SIREMOBIL Iso-C3D. Dentomaxillofac Radiol 33:130–132, 2004
Heiland M, Schulze D, Adam G, Schmelzle R: 3D-imaging of the facial skeleton with an isocentric mobile C-arm system (Siremobil Iso-C3D). Dentomaxillofac Radiol 32:21–25, 2003
Verlaan JJ, van de Kraats EB, Dhert WJ, Oner FC: The role of 3-D rotational x-ray imaging in spinal trauma. Injury 36 Suppl 2:B98–B103, 2005
Grutzner PA, Suhm N: Computer aided long bone fracture treatment. Injury 35 Suppl 1:S-A57-A64, 2004
Noble PC, Sugano N, Johnston JD, Thompson MT, Conditt MA, Engh CA, Sr., Mathis KB: Computer simulation: how can it help the surgeon optimize implant position? Clin Orthop Relat Res:242–252, 2003
Sagbo S, Blochaou F, Langlotz F, Vangenot C, Nolte L, Zheng G: A semi-automatic orthopedic implant management tool for computer assisted planning, navigation and simulation: from XML implant database to unified implant access interface. Conf Proc IEEE Eng Med Biol Soc 1:890–893, 2005
Zheng G, Ballester MA, Styner M, Nolte LP: Reconstruction of patient-specific 3D bone surface from 2D calibrated fluoroscopic images and point distribution model. Med Image Comput Comput Assist Interv Int Conf Med Image Comput Comput Assist Interv 9:25–32, 2006
Acknowledgments
The authors thank the following for contributing to this study: Department of Pathology, University Hospital of Basel/Switzerland (Prof. M.J. Mihatsch and Ralf Schoch) for supplying the bone specimen. Department of Radiology, University Hospital, Basel/Switzerland (Ms Severin Dziergwa) for performing repeated computed tomography scans. The AO Research Institute, Davos/Switzerland (Dr. Karsten Schwieger and Mr. Boyko Gueorguiev) for assisting in creating a controlled bone fracture. The AO Development Institute, Davos/Switzerland (Dr. Hanspeter Noser) for granting access to the AO bone database. The AO bone database is available to partner institutes for dedicated research projects. This study was co-funded by the Robert Mathys Foundation, Bettlach/Switzerland (Grant E06-0001) and a donation from Mrs M. Täsch Furger, Stäfa/Switzerland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matthews, F., Messmer, P., Raikov, V. et al. Patient-Specific Three-Dimensional Composite Bone Models for Teaching and Operation Planning. J Digit Imaging 22, 473–482 (2009). https://doi.org/10.1007/s10278-007-9078-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-007-9078-8