Abstract
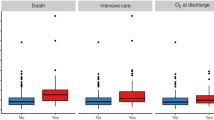
Severe acute respiratory syndrome-corona virus 2 (SARS-CoV-2) is associated with significant morbidity and mortality. C-reactive protein (CRP) is a useful inflammatory biomarker for patients admitted with an infection. This study aimed to compare CRP level as an indicator of inflammation severity between SARS-CoV-2 and common respiratory viral infections. A cross-sectional study of all adult patients hospitalized in the internal medicine department, geriatric department, or internal intensive care unit between 02/2012 and 06/2021 with laboratory-confirmed respiratory viral infection was performed. SARS-CoV-2, influenza A, influenza B, and respiratory syncytial virus (RSV) were studied. Patients with laboratory-confirmed concurrent viral or bacterial infections were excluded. Patients with malignancy were also excluded. Age, gender, comorbidities, and CRP level upon admission were compared between groups. Univariate and multivariable analyses were applied. Among 1124 patients, 18.2% had SARS‑CoV‑2, 48.3% influenza A, 18.9% RSV, and 14.6% influenza B. SARS‑CoV‑2 patients were significantly younger (median 69.4 vs. ≥ 76 years) and had lower Charlson score (median 3 vs. ≥ 4 in other groups) compared to patients with other viral pathogens. After adjustment for patients’ age, gender and comorbidities, SARS‑CoV‑2 patients had a higher probability (OR = 1.84–2.02, p < 0.01) of having CRP values in the upper quartile (> 117 mg/L) compared to all other viral pathogens while between all others there was no significant difference. To conclude, a higher CRP level upon admission is approximately twice more common among SARS-CoV-2 patients compared to other widespread respiratory viruses which may demonstrate the higher intensity of inflammation caused by SARS-CoV-2.



Similar content being viewed by others
References
Israeli Ministry of Health. COVID-19 Data Tracker. Isr Minist Heal 2022. https://datadashboard.health.gov.il/COVID-19/general.
Strålin K, Wahlström E, Walther S, et al. Mortality in hospitalized COVID-19 patients was associated with the COVID-19 admission rate during the first year of the pandemic in Sweden. Infect Dis (Auckl). 2022;54:145–51. https://doi.org/10.1080/23744235.2021.1983643/SUPPL_FILE/INFD_A_1983643_SM7321.EPS.
Asch DA, Sheils NE, Islam MN, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021;181:471–8. https://doi.org/10.1001/JAMAINTERNMED.2020.8193.
Strålin K, Wahlström E, Walther S, et al. Mortality trends among hospitalised COVID-19 patients in Sweden: a nationwide observational cohort study. Lancet Reg Heal Eur. 2021;4:100054. https://doi.org/10.1016/J.LANEPE.2021.100054.
Brosh-Nissimov T, Orenbuch-Harroch E, Chowers M, et al. BNT162b2 vaccine breakthrough: clinical characteristics of 152 fully vaccinated hospitalized COVID-19 patients in Israel. Clin Microbiol Infect. 2021;27:1652. https://doi.org/10.1016/J.CMI.2021.06.036.
Morris G, Bortolasci CC, Puri BK, et al. The cytokine storms of COVID-19, H1N1 influenza, CRS and MAS compared Can one sized treatment fit all? Cytokine. 2021;144:155593. https://doi.org/10.1016/J.CYTO.2021.155593.
da Costa VG, Saivish MV, Santos DER, de Lima Silva RF, Moreli ML. Comparative epidemiology between the 2009 H1N1 influenza and COVID-19 pandemics. J Infect Public Health. 2020;13:1797–804. https://doi.org/10.1016/J.JIPH.2020.09.023.
Petersen E, Koopmans M, Go U, et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020;20:e238–44. https://doi.org/10.1016/S1473-3099(20)30484-9.
Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999;17:1019–25. https://doi.org/10.1016/S0736-4679(99)00135-3.
Haran JP, Suner S, Gardiner F. Correlation of C-reactive protein to severity of symptoms in acute influenza A infection. J Emerg Trauma Shock. 2012;5:149. https://doi.org/10.4103/0974-2700.96484.
Vasileva D, Badawi A. C-reactive protein as a biomarker of severe H1N1 influenza. Inflamm Res. 2019;68:39. https://doi.org/10.1007/S00011-018-1188-X.
Povoa P, Teixeira-Pinto A, Carneiro A. C-reactive protein as an early marker of sepsis resolution: results from the Portuguese Community-acquired Sepsis Study (SACiUCI study). Crit Care. 2011. https://doi.org/10.1186/cc9692.
Zhou P, Lou YX, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3. https://doi.org/10.1038/s41586-020-2012-7.
Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–80.e8. https://doi.org/10.1016/J.CELL.2020.02.052.
Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Auckl). 2021;53:737–54. https://doi.org/10.1080/23744235.2021.1924397/SUPPL_FILE/INFD_A_1924397_SM4019.DOCX.
Trougakos IP, Stamatelopoulos K, Terpos E, et al. Insights to SARS-CoV-2 life cycle, pathophysiology, and rationalized treatments that target COVID-19 clinical complications. J Biomed Sci. 2021;28:1–18. https://doi.org/10.1186/S12929-020-00703-5.
Ponti G, Maccaferri M, Ruini C, Tomasi A, Ozben T. Biomarkers associated with COVID-19 disease progression. Crit Rev Clin Lab Sci. 2020;57:389–99. https://doi.org/10.1080/10408363.2020.1770685.
Wang G, Wu C, Zhang Q, et al. C-reactive protein level may predict the risk of COVID-19 aggravation. Open Forum Infect Dis. 2020. https://doi.org/10.1093/ofid/ofaa153.
Luo X, Zhou W, Yan X, et al. Prognostic value of C-reactive protein in patients with coronavirus 2019. Clin Infect Dis. 2020;71:2174–9. https://doi.org/10.1093/CID/CIAA641.
Pepys MB. C-reactive protein predicts outcome in COVID-19: is it also a therapeutic target? Eur Heart J. 2021;42:2280. https://doi.org/10.1093/EURHEARTJ/EHAB169.
Malik P, Patel U, Mehta D, et al. Emergency care: Biomarkers and outcomes of COVID-19 hospitalisations: systematic review and meta-analysis. BMJ Evid Based Med. 2020;26:107–8. https://doi.org/10.1136/BMJEBM-2020-111536.
Fazal M. C-reactive protein a promising biomarker of COVID-19 severity. Korean J Clin Lab Sci. 2021;53:201–7. https://doi.org/10.15324/KJCLS.2021.53.3.201.
Loomba RS, Villarreal EG, Farias JS, Aggarwal G, Aggarwal S, Flores S. Serum biomarkers for prediction of mortality in patients with COVID-19. Ann Clin Biochem. 2022;59:15–22. https://doi.org/10.1177/00045632211014244.
Villoteau A, Asfar M, Otekpo M, Loison J, Gautier J, Annweiler C. Elevated C-reactive protein in early COVID-19 predicts worse survival among hospitalized geriatric patients. PLoS ONE. 2021. https://doi.org/10.1371/JOURNAL.PONE.0256931.
Milenkovic M, Hadzibegovic A, Kovac M, et al. D-dimer, CRP, PCT, and IL-6 levels at admission to ICU can predict in-hospital mortality in patients with COVID-19 pneumonia. Oxid Med Cell Longev. 2022. https://doi.org/10.1155/2022/8997709.
Yitbarek GY, Ayehu GW, Asnakew S, et al. The role of C-reactive protein in predicting the severity of COVID-19 disease: a systematic review. SAGE Open Med. 2021;9:205031212110507. https://doi.org/10.1177/20503121211050755.
Liu F, Li L, Xu MD, et al. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020;127:104370. https://doi.org/10.1016/J.JCV.2020.104370.
Feigin E, Levinson T, Wasserman A, Shenhar-Tsarfaty S, Berliner S, Ziv-Baran T. Age-dependent biomarkers for prediction of in-hospital mortality in COVID-19 patients. J Clin Med. 2022;11:2682. https://doi.org/10.3390/JCM11102682.
Ziv-Baran T, Wasserman A, Goldiner I, et al. The association between C-reactive protein and common blood tests in apparently healthy individuals undergoing a routine health examination. Clin Chim Acta. 2020. https://doi.org/10.1016/j.cca.2019.12.002.
Fajgenbaum DC, June CH. Cytokine storm. N Engl J Med. 2020;383:2255–73. https://doi.org/10.1056/NEJMra2026131.
Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect. 2020;80:607–13. https://doi.org/10.1016/J.JINF.2020.03.037.
Sahu BR, Kampa RK, Padhi A, Panda AK. C-reactive protein: a promising biomarker for poor prognosis in COVID-19 infection. Clin Chim Acta. 2020;509:91–4. https://doi.org/10.1016/J.CCA.2020.06.013.
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. https://doi.org/10.1016/S0140-6736(20)30628-0.
Wang C, Kang K, Gao Y, et al. Cytokine levels in the body fluids of a patient with COVID-19 and acute respiratory distress syndrome: a case report. Ann Intern Med. 2020;173:499–501. https://doi.org/10.7326/L20-0354.
Sterne JAC, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–41. https://doi.org/10.1001/JAMA.2020.17023.
Domingo P, Mur I, et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA. 2021;326:499–518. https://doi.org/10.1001/JAMA.2021.11330.
Ghosn L, Chaimani A, Evrenoglou T, et al. Interleukin-6 blocking agents for treating COVID-19: a living systematic review. Cochrane Database Syst Rev. 2021. https://doi.org/10.1002/14651858.CD013881/INFORMATION/EN.
Marconi VC, Ramanan AV, de Bono S, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med. 2021;9:1407–18. https://doi.org/10.1016/S2213-2600(21)00331-3.
Aljabr W, Al-Amari A, Abbas B, et al. Evaluation of the levels of peripheral CD3+, CD4+, and CD8+ and IgG and IgM antibodies in COVID-19 patients at different stages of infection. Microbiol Spectr. 2022;10(1):e0084521. https://doi.org/10.1128/spectrum.00845-21.
Scalia G, Raia M, Gelzo M, et al. Lymphocyte population changes at two time points during the acute period of COVID-19 infection. J Clin Med. 2022;11(15):4306. https://doi.org/10.3390/jcm11154306.
Yang WJ, Cho IR, Seong DH, et al. Clinical implication of serum C-reactive protein in patients with uncomplicated acute pyelonephritis as marker of prolonged hospitalization and recurrence. Urology. 2009;73(1):19–22. https://doi.org/10.1016/j.urology.2008.07.061.
Andersen SB, Egelund GB, Jensen AV, Petersen PT, Rohde G, Ravn P. Failure of CRP decline within three days of hospitalization is associated with poor prognosis of community-acquired pneumonia. Infect Dis (Lond). 2017;49(4):251–60. https://doi.org/10.1080/23744235.2016.1253860.
Funding
This work was supported in part by the Dalia and Arie Prashkovsky grant for biomedical research.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by SS-T, OH and TL. Analysis was performed by TZ-B. TZ-B, SB, AW and TL were responsible for the methodology. Supervision was performed by IS, DZ, OR and SB. The first draft of the manuscript was written by AW, TL and TZ-B and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Levinson, T., Wasserman, A., Shenhar-Tsarfaty, S. et al. Comparative analysis of CRP as a biomarker of the inflammatory response intensity among common viral infections affecting the lungs: COVID-19 versus influenza A, influenza B and respiratory syncytial virus. Clin Exp Med 23, 5307–5313 (2023). https://doi.org/10.1007/s10238-023-01176-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01176-0