Abstract
Background
Pazopanib is a multi-tyrosine kinase inhibitor that is used to treat advanced soft-tissue sarcoma, and its efficacy has been confirmed in several clinical trials, although no clinically useful biomarkers have been identified. In other cancers, the neutrophil-to-lymphocyte ratio (NLR), the platelet-to-lymphocyte ratio (PLR), and the lymphocyte-to-monocyte ratio (LMR) are associated with chemotherapy response and prognosis. Therefore, we aimed to evaluate the associations of pazopanib response with NLR, PLR, and LMR among patients with advanced soft-tissue sarcoma.
Methods
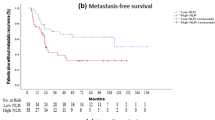
Data regarding NLR, PLR, and LMR were obtained for 25 patients who received pazopanib for soft-tissue sarcoma. The patients were categorized according to their values for NLR (≥3.8 vs. <3.8), PLR (≥230 vs. <230), and LMR (≥2.4 vs. <2.4), and we evaluated the associations of these markers with progression-free survival and overall survival using Kaplan–Meier curves and Cox proportional models.
Results
No significant differences in progression-free survival or overall survival were observed based on the pre-treatment NLR, PLR, and LMR values. However, decreased NLR values after treatment using pazopanib were independently associated with significantly prolonged progression-free survival (hazard ratio: 0.07, p = 0.001) and overall survival (hazard ratio: 0.17, p = 0.0006).
Conclusions
Decreased NLR values after treatment using pazopanib may predict high efficacy and favorable outcomes among patients with advanced soft-tissue sarcoma.



Similar content being viewed by others
References
Clark MA, Fisher C, Judson I et al (2005) Soft-tissue sarcomas in adults. N Engl J Med 353:701–711
Byerly S, Chopra S, Nassif NA et al (2016) The role of margins in extremity soft tissue sarcoma. J Surg Oncol 113:333–338
Callegaro D, Miceli R, Bonvalot S et al (2016) Development and external validation of two nomograms to predict overall survival and occurrence of distant metastases in adults after surgical resection of localised soft-tissue sarcomas of the extremities: a retrospective analysis. Lancet Oncol 17:671–680
van der Graaf WT, Blay JY, Chawla SP et al (2012) Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomized, double-blind, placebo-controlled phase 3 trial. Lancet 379:1879–1886
Schöffski P, Chawla S, Maki RG et al (2016) Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: a randomised, open-label, multicentre, phase 3 trial. Lancet 387:1629–1637
Kawai A, Araki N, Sugiura H et al (2015) Trabectedin monotherapy after standard chemotherapy versus best supportive care in patients with advanced, translocation-related sarcoma: a randomised, open-label, phase 2 study. Lancet Oncol 16:406–416
Demetri GD, Chawla SP, von Mehren M et al (2009) Efficacy and safety of trabectedin or dacarbazine for metastatic liposarcoma or leiomyosarcoma after failure of conventional chemotherapy: results of a phase III randomized multicenter clinical trial. J Clin Oncol 27:4188–4196
Koehler K, Liebner D, Chen JL (2016) TP53 mutational status is predictive of pazopanib response in advanced sarcomas. Ann Oncol 27:539–543
Palma N, Morris JC, Ali SM et al (2015) Exceptional response to pazopanib in a patient with urothelial carcinoma harboring FGFR3 activating mutation and amplification. Eur Urol 68:168–170
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12:223–226
Schreiber RD, Old LJ, Smyth MJ (2011) Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331:1565–1570
Qi Q, Zhuang L, Shen Y et al (2016) A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer 122:2158–2167
Wang F, Liu ZY, **a YY et al (2015) Changes in neutrophil/lymphocyte and platelet/lymphocyte ratios after chemotherapy correlate with chemotherapy response and prediction of prognosis in patients with unresectable gastric cancer. Oncol Lett 10:3411–3418
Asano Y, Kashiwagi S, Onoda N et al (2016) Predictive value of neutrophil/lymphocyte ratio for efficacy of preoperative chemotherapy in triple-negative breast cancer. Br J Cancer 114:14–20
Ni XJ, Zhang XL, Ou-Yang QW et al (2014) An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PLoS One 9:e111886
Jiang L, Jiang S, Situ D et al (2015) Prognostic value of monocyte and neutrophils to lymphocytes ratio in patients with metastatic soft tissue sarcoma. Oncotarget 6:9542–9550
Szkandera J, Gerger A, Liegl-Atzwanger B et al (2015) The derived neutrophil/lymphocyte ratio predicts poor clinical outcome in soft tissue sarcoma patients. Am J Surg 210:111–116
Que Y, Qiu H, Li Y et al (2015) Preoperative platelet-lymphocyte ratio is superior to neutrophil-lymphocyte ratio as a prognostic factor for soft-tissue sarcoma. BMC Cancer 15:648
Kobayashi N, Usui S, Kikuchi S et al (2012) Preoperative lymphocyte count is an independent prognostic factor in node-negative non-small cell lung cancer. Lung Cancer 75:223–227
Milne K, Alexander C, Webb JR et al (2012) Absolute lymphocyte count is associated with survival in ovarian cancer independent of tumor-infiltrating lymphocytes. J Transl Med 10:33
Kusumanto YH, Dam WA, Hospers GA et al (2003) Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6:283–287
Nagaraj S, Schrum AG, Cho HI et al (2010) Mechanism of T cell tolerance induced by myeloid-derived suppressor cells. J Immunol 15:3106–3116
Kobayashi M, Kubo T, Komatsu K et al (2013) Changes in peripheral blood immune cells: their prognostic significance in metastatic renal cell carcinoma patients treated with molecular targeted therapy. Med Oncol 30:556
Terme M, Pernot S, Marcheteau E et al (2013) VEGFA-VEGFR pathway blockade inhibits tumor-induced regulatory T-cell proliferation in colorectal cancer. Cancer Res 73:539–549
Sharpe K, Stewart GD, Mackay A et al (2013) The effect of VEGF-targeted therapy on biomarker expression in sequential tissue from patients with metastatic clear cell renal cancer. Clin Cancer Res 19:6924–6934
Pal SK, Hossain DM, Zhang Q et al (2015) Pazopanib as third line therapy for metastatic renal cell carcinoma: clinical efficacy and temporal analysis of cytokine profile. J Urol 193:1114–1121
Gasic GJ, Gasic TB, Stewart CC (1968) Antimetastatic effects associated with platelet reduction. Proc Natl Acad Sci USA 61:46–52
Nieswandt B, Hafner M, Echtenacher B et al (1999) Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res 59:1295–1300
Labelle M, Begum S, Hynes RO (2011) Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell 20:576–590
Yoshizawa K, Okamoto T, Moriya K et al (1994) Effects of natural human interleukin-6 on thrombopoiesis and tumor progression in tumor-bearing mice. Cancer Lett 79:83–89
Nakamura T, Matsumine A, Kawai A et al (2016) The clinical outcome of pazopanib treatment in Japanese patients with relapsed soft tissue sarcoma: a Japanese Musculoskeletal Oncology Group (JMOG) study. Cancer 122:1408–1416
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
All authors declare that there are no conflicts of interest relevant to this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kobayashi, H., Okuma, T., Oka, H. et al. Neutrophil-to-lymphocyte ratio after pazopanib treatment predicts response in patients with advanced soft-tissue sarcoma. Int J Clin Oncol 23, 368–374 (2018). https://doi.org/10.1007/s10147-017-1199-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1199-6