Abstract
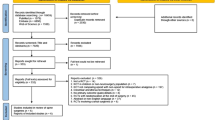
In recent years, nonsteroidal anti-inflammatory drug (NSAIDs), which are considered to affect the prognosis of spinal surgery, have been widely used in perioperative analgesia in spinal surgery, but the relationship between these two factors remains unclear. The purpose of this study was to explore the effect of perioperative use of NSAIDs on the prognosis of patients treated with spinal surgery. We systematically searched PubMed, Embase, and Cochrane Library for relevant articles published on or before July 14, 2023. We used a random-effect model for the meta-analysis to calculate the standardized mean difference (SMD) with a 95% confidence interval (CI). Sensitivity analyses were conducted to analyze stability. A total of 23 randomized clinical trials including 1457 participants met the inclusion criteria. Meta-analysis showed that NSAIDs were significantly associated with postoperative morphine use (mg) (SMD = -0.90, 95% CI -1.12 to -0.68) and postoperative pain (SMD = -0.71, 95% CI -0.85 to -0.58). These results were further confirmed by the trim-and-fill procedure and leave-one-out sensitivity analyses. The current study shows that perioperative use of NSAIDs appears to be an important factor in reducing postoperative pain and morphine use in patients undergoing spinal surgery. However, well-designed, high-quality randomized controlled trials (RCTs) are still required.






Similar content being viewed by others
Data availability
All the data sets used and analysed in this study were published and are available and can be shared by eligible investigators.
References
Kushner P et al (2022) The use of non-steroidal anti-inflammatory drugs (NSAIDs) in COVID-19. NPJ Prim Care Respir Med 32(1):35
McCormack K (1994) Non-steroidal anti-inflammatory drugs and spinal nociceptive processing. Pain 59(1):9–43
Souter AJ, Fredman B, White PF (1994) Controversies in the perioperative use of nonsterodial antiinflammatory drugs. Anesth Analg 79(6):1178–1190
Odineal DD et al (2020) Effect of Mobile device-assisted N-of-1 trial participation on Analgesic Prescribing for Chronic Pain: Randomized Controlled Trial. J Gen Intern Med 35(1):102–111
Yeom JH et al (2012) Peri-operative ketamine with the ambulatory elastometric infusion pump as an adjuvant to manage acute postoperative pain after spinal fusion in adults: a prospective randomized trial. Korean J Anesthesiology 63(1):54–58
(a)Reuben SS, Ablett D, Kaye R (2005) High dose nonsteroidal anti-inflammatory drugs compromise spinal fusion. Can J Anesth 52(5):506–512
Yoo JS et al (2019) Multimodal analgesia in pain management after spine surgery. J Spine Surg 5(Suppl 2):S154–s159
Licina A, Silvers A (2022) Perioperative Multimodal Analgesia for adults undergoing surgery of the Spine-A systematic review and Meta-analysis of three or more modalities. World Neurosurg 163:11–23
Hiller A et al (2012) Acetaminophen improves analgesia but does not reduce opioid requirement after major spine surgery in children and adolescents. Spine 37(20):E1225–E1231
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (clinical research ed. 372:n71
Sterne JAC et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Luo M et al The impact of diabetes on postoperative outcomes following spine surgery: a meta-analysis of 40 cohort studies with 2.9 million participants. (1743–9159 (Electronic)).
Duval S, Tweedie R Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. (0006-341X (Print)).
(b)Reuben SS, Ekman EF, The effect of cyclooxygenase-2 inhibition on analgesia and spinal fusion (Retraction in: Journal of Bone and Joint Surgery -, Series A (2009) 91:4 (965)). Journal of Bone and Joint Surgery, 2005. 87(3): p. 536–542
Aubrun F et al (2000) Randomised, placebo-controlled study of the postoperative analgesic effects of ketoprofen after spinal fusion surgery. Acta Anaesthesiol Scand 44(8):934–939
Grundmann U et al (2006) The efficacy of the non-opioid analgesics parecoxib, Paracetamol and metamizol for postoperative pain relief after lumbar microdiscectomy. Anesth Analg 103(1):217–222
Karst M et al (2003) Effect of celecoxib and dexamethasone on postoperative pain after lumbar disc surgery. Neurosurgery 53(2):331–337
Kelsaka E, Güldoğuş F, Cetinoğlu E (2014) Effect of intravenous dexketoprofen use on postoperative analgesic consumption in patients with lumbar disc surgery. Aǧrı: Ağrı (Algoloji) Derneği’nin Yayın. organıdır = J Turkish Soc Algology 26(2):82–86
Kraiwattanapong C et al (2020) Effect of multimodal drugs infiltration on postoperative pain in split laminectomy of lumbar spine: a randomized controlled trial. Spine 45(24):1687–1695
Munro HM et al (2002) Low-dose ketorolac improves analgesia and reduces morphine requirements following posterior spinal fusion in adolescents. Can J Anesth 49(5):461–466
Raja S (2019) A prospective randomized study to analyze the efficacy of balanced pre-emptive analgesia in spine surgery. Spine J 19(4):569–577
Reuben SS et al (1998) Dose-response of ketorolac as an adjunct to patient-controlled analgesia morphine in patients after spinal fusion surgery. Anesth Analg 87(1):98–102
Reuben SS, Connelly NR, Steinberg R (1997) Ketorolac as an adjunct to patient-controlled morphine in postoperative spine surgery patients. Reg Anesth 22(4):343–346
Siribumrungwong K et al (2015) Comparing parecoxib and ketorolac as preemptive analgesia in patients undergoing posterior lumbar spinal fusion: a prospective randomized double-blinded placebo-controlled trial. BMC Musculoskelet Disord, 16(1)
Bekker A et al (2002) Evaluation of preoperative administration of the cyclooxygenase-2 inhibitor rofecoxib for the treatment of postoperative pain after lumbar disc surgery. Neurosurgery, 50(5): p. 1053-7; discussion 1057-8
Bilir S et al (2016) Effects of peroperative intravenous Paracetamol and lornoxicam for lumbar disc surgery on postoperative pain and opioid consumption: a randomized, prospective, placebo-controlled study. Agri 28(2):98–105
Cassinelli EH et al (2008) Ketorolac use for postoperative pain management following lumbar decompression surgery: a prospective, randomized, double-blinded, placebo-controlled trial. Spine (Phila Pa 1976) 33(12):1313–1317
Jirarattanaphochai K et al (2008) Effect of parecoxib on postoperative pain after lumbar spine surgery: a bicenter, randomized, double-blinded, placebo-controlled trial. Spine (Phila Pa 1976) 33(2):132–139
Korkmaz Dilmen O et al (2010) Efficacy of intravenous Paracetamol, metamizol and lornoxicam on postoperative pain and morphine consumption after lumbar disc surgery. Eur J Anaesthesiol 27(5):428–432
McGlew IC et al (1991) A comparison of rectal indomethacin with placebo for pain relief following spinal surgery. Anaesth Intensive Care 19(1):40–45
Nissen I, Jensen KA, Ohrström JK (1992) Indomethacin in the management of postoperative pain. Br J Anaesth 69(3):304–306
Pookarnjanamorakot C, Laohacharoensombat W, Jaovisidha S (2002) The clinical efficacy of piroxicam fast-dissolving dosage form for postoperative pain control after simple lumbar spine surgery: a double-blinded randomized study. Spine (Phila Pa 1976) 27(5):447–451
Reuben SS et al (2009) The analgesic efficacy of celecoxib, pregabalin, and their combination for spinal fusion surgery (Retraction in: Anesthesia and Analgesia 108:4 (1350)). Anesthesia and Analgesia, 2006. 103(5): p. 1271–1277
Singhatanadgige W et al (2020) No difference in Pain after spine surgery with local Wound Filtration of Morphine and Ketorolac: a Randomized Controlled Trial. Clin Orthop Relat Res 478(12):2823–2829
Srivastava S et al (2012) Effects of preoperative single dose etoricoxib on postoperative pain and sleep after lumbar diskectomy: prospective randomized double blind controlled study. Middle East J Anaesthesiol 21(5):725–730
Zhang Z et al (2017) Nonsteroidal anti-inflammatory drugs for postoperative pain control after lumbar spine surgery: a meta-analysis of randomized controlled trials. J Clin Anesth 43:84–89
Cashman JN (1996) The mechanisms of action of NSAIDs in analgesia. Drugs 52(Suppl 5):13–23
Funding
This work was supported by the Health and Family Planning Commission Program of Hunan Province (no. 202204074707), and the Health and Family Planning Commission Program of Wuhan City (no. WX18C29).
Author information
Authors and Affiliations
Contributions
ML and GY conceived the idea for the review and with all other authors designed the protocol. FS, ZT, JT, YK, BZ, ZC, DK, JJ, JX, ZY and HW constructed the search. ML, GY and HD selected the studies and extracted the relevant data. ML and ZX wrote the original draft and ZX, ML and ZX critically revised and edited successive drafts of the paper. All authors gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, M., Yang, G., Dai, H. et al. The impact of perioperative nonsteroidal anti-inflammatory drugs on the postoperative outcomes of spinal surgery: a meta-analysis of 23 randomized controlled trials. Neurosurg Rev 47, 140 (2024). https://doi.org/10.1007/s10143-024-02371-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-024-02371-7