Abstract
Objective
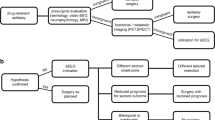
To describe the association between preoperative ictal scalp electroencephalogram (EEG) results and surgical outcomes in patients with focal epilepsies.
Methods
The data of consecutive patients with focal epilepsies who received surgical treatments at our center from January 2012 to December 2021 were retrospectively analyzed.
Results
Our data showed that 44.2% (322/729) of patients had ictal EEG recorded on video EEG monitoring during preoperative evaluation, of which 60.6% (195/322) had a concordant ictal EEG results. No significant difference of surgery outcomes between patients with and without ictal EEG was discovered. Among MRI-negative patients, those with concordant ictal EEG had a significantly better outcome than those without ictal EEG (75.7% vs. 43.8%, p = 0.024). Further logistic regression analysis showed that concordant ictal EEG was an independent predictor for a favorable outcome (OR = 4.430, 95%CI 1.175–16.694, p = 0.028). Among MRI-positive patients, those with extra-temporal lesions and discordant ictal EEG results had a worse outcome compared to those without an ictal EEG result (44.7% vs. 68.8%, p = 0.005). Further logistic regression analysis showed that discordant ictal EEG was an independent predictor of worse outcome (OR = 0.387, 95%CI 0.186–0.807, p = 0.011) in these patients. Furthermore, our data indicated that the number of seizures was not associated with the concordance rates of the ictal EEG, nor the surgical outcomes.
Conclusions
The value of ictal scalp EEG for epilepsy surgery varies widely among patients. A concordant ictal EEG predicts a good surgical outcome in MRI-negative patients, whereas a discordant ictal EEG predicts a poor postoperative outcome in lesional extratemporal lobe epilepsy.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, [hua zhang], upon reasonable request.
References
European federation of neurological societies task force (2000) Pre-surgical evaluation for epilepsy surgery - European standards. Eur J Neurol 7(1):119–122. https://doi.org/10.1046/j.1468-1331.2000.00004.x
Struck AF, Cole AJ, Cash SS, Westover MB (2015) The number of seizures needed in the emu. Epilepsia 56(11):1753–1759. https://doi.org/10.1111/epi.13090
Henning O, Baftiu A, Johannessen SI, Landmark CJ (2014) Withdrawal of antiepileptic drugs during presurgical video-eeg monitoring: an observational study for evaluation of current practice at a referral center for epilepsy. Acta Neurol Scand 129(4):243–251. https://doi.org/10.1111/ane.12179
Liu J, Chen D, Xu Y, Zhang Y, Liu L (2023) Safety and efficacy of rapid withdrawal of anti-seizure medication during long-term video-eeg monitoring. Front Neurol 141196078. https://doi.org/10.3389/fneur.2023.1196078
Kumar S, Ramanujam B, Chandra PS et al (2018) Randomized controlled study comparing the efficacy of rapid and slow withdrawal of antiepileptic drugs during long-term video-eeg monitoring. Epilepsia 59(2):460–467. https://doi.org/10.1111/epi.13966
Ding Y, Zhu Y, Jiang B et al (2018) (18)f-fdg pet and high-resolution mri co-registration for pre-surgical evaluation of patients with conventional mri-negative refractory extra-temporal lobe epilepsy. Eur J Nucl Med Mol Imaging 45(9):1567–1572. https://doi.org/10.1007/s00259-018-4017-0
Sharma HK, Feldman R, Delman B et al (2021) Utility of 7 tesla mri brain in 16 mri negative epilepsy patients and their surgical outcomes. Epilepsy Behav Rep 15100424. https://doi.org/10.1016/j.ebr.2020.100424
Hur YJ, Kim AJ, Nordli DJ (2017) Mri supersedes ictal eeg when other presurgical data are concordant. Seizure 5318–22. https://doi.org/10.1016/j.seizure.2017.10.013
Makridis KL, Prager C, Atalay DA et al (2022) Ictal eeg recording is not mandatory in all candidates for paediatric epilepsy surgery with clear mri lesions and corresponding seizure semiology. Epileptic Disord 24(4):657–666. https://doi.org/10.1684/epd.2022.1436
Castro-Villablanca F, Moeller F, Pujar S et al (2022) Seizure outcome determinants in children after surgery for single unilateral lesions on magnetic resonance imaging: role of preoperative ictal and interictal electroencephalography. Epilepsia 63(12):3168–3179. https://doi.org/10.1111/epi.17425
Vollmar C, Stredl I, Heinig M, Noachtar S, Remi J (2018) Unilateral temporal interictal epileptiform discharges correctly predict the epileptogenic zone in lesional temporal lobe epilepsy. Epilepsia 59(8):1577–1582. https://doi.org/10.1111/epi.14514
Tezer FI, Dericioglu N, Bozkurt G, Bilginer B, Akalan N, Saygi S (2011) Epilepsy surgery in patients with unilateral mesial temporal sclerosis and contralateral scalp ictal onset. Turk Neurosurg 21(4):549–554
Catarino CB, Vollmar C, Noachtar S (2012) Paradoxical lateralization of non-invasive electroencephalographic ictal patterns in extra-temporal epilepsies. Epilepsy Res 99(1–2):147–155. https://doi.org/10.1016/j.eplepsyres.2011.11.002
Tatum WT, Benbadis SR, Hussain A et al (2008) Ictal eeg remains the prominent predictor of seizure-free outcome after temporal lobectomy in epileptic patients with normal brain mri. Seizure 17(7):631–636. https://doi.org/10.1016/j.seizure.2008.04.001
Wang X, Zhang C, Wang Y et al (2016) Prognostic factors for seizure outcome in patients with mri-negative temporal lobe epilepsy: a meta-analysis and systematic review. Seizure 3854–62. https://doi.org/10.1016/j.seizure.2016.04.002
Elwan S, Alexopoulos A, Silveira DC, Kotagal P (2018) Lateralizing and localizing value of seizure semiology: comparison with scalp eeg, mri and pet in patients successfully treated with resective epilepsy surgery. Seizure 61203–208. https://doi.org/10.1016/j.seizure.2018.08.026
Foldvary N, Klem G, Hammel J, Bingaman W, Najm I, Luders H (2001) The localizing value of ictal eeg in focal epilepsy. Neurology 57(11):2022–2028. https://doi.org/10.1212/wnl.57.11.2022
Asadollahi M, Sperling MR, Rabiei AH, Asadi-Pooya AA (2017) Drug-resistant parietal lobe epilepsy: clinical manifestations and surgery outcome. Epileptic Disord 19(1):35–39. https://doi.org/10.1684/epd.2017.0893
Garganis K, Kokkinos V, Zountsas B (2012) Extratemporal surface eeg features do not preclude successful surgical outcomes in drug-resistant epilepsy patients with unitemporal mri lesions. Epileptic Disord 14(3):275–289. https://doi.org/10.1684/epd.2012.0527
Hupalo M, Wojcik R, Jaskolski DJ (2017) Intracranial video-eeg monitoring in presurgical evaluation of patients with refractory epilepsy. Neurol Neurochir Pol 51(3):201–207. https://doi.org/10.1016/j.pjnns.2017.02.002
Minotti L, Montavont A, Scholly J, Tyvaert L, Taussig D (2018) Indications and limits of stereoelectroencephalography (seeg). Neurophysiol Clin 48(1):15–24. https://doi.org/10.1016/j.neucli.2017.11.006
Guo Z, Zhang C, Wang X et al (2022) Is intracranial electroencephalography mandatory for mri-negative neocortical epilepsy surgery? J Neurosurg 1–11. https://doi.org/10.3171/2022.8.JNS22995
Steinbrenner M, Duncan JS, Dickson J et al (2022) Utility of 18f-fluorodeoxyglucose positron emission tomography in presurgical evaluation of patients with epilepsy: a multicenter study. Epilepsia 63(5):1238–1252. https://doi.org/10.1111/epi.17194
Czarnetzki C, Spinelli L, Huppertz HJ et al (2023) Yield of non-invasive imaging in mri-negative focal epilepsy. J Neurol. https://doi.org/10.1007/s00415-023-11987-6
Remi J, Vollmar C, de Marinis A, Heinlin J, Peraud A, Noachtar S (2011) Congruence and discrepancy of interictal and ictal eeg with mri lesions in focal epilepsies. Neurology 77(14):1383–1390. https://doi.org/10.1212/WNL.0b013e31823152c3
Monnerat BZ, Velasco TR, Assirati JJ, Carlotti CJ, Sakamoto AC (2013) On the prognostic value of ictal eeg patterns in temporal lobe epilepsy surgery: a cohort study. Seizure 22(4):287–291. https://doi.org/10.1016/j.seizure.2013.01.019
Alvim M, Morita ME, Yasuda CL et al (2018) Is inpatient ictal video-electroencephalographic monitoring mandatory in mesial temporal lobe epilepsy with unilateral hippocampal sclerosis? A prospective study. Epilepsia 59(2):410–419. https://doi.org/10.1111/epi.13977
Schmeiser B, Zentner J, Steinhoff BJ et al (2017) The role of presurgical eeg parameters and of reoperation for seizure outcome in temporal lobe epilepsy. Seizure 51:174–179. https://doi.org/10.1016/j.seizure.2017.08.015
Liava A, Mai R, Cardinale F et al (2016) Epilepsy surgery in the posterior part of the brain. Epilepsy Behav 64(Pt A):273–282. https://doi.org/10.1016/j.yebeh.2016.09.025
Jehi LE, O’Dwyer R, Najm I, Alexopoulos A, Bingaman W (2009) A longitudinal study of surgical outcome and its determinants following posterior cortex epilepsy surgery. Epilepsia 50(9):2040–2052. https://doi.org/10.1111/j.1528-1167.2009.02070.x
Holtkamp M, Sharan A, Sperling MR (2012) Intracranial eeg in predicting surgical outcome in frontal lobe epilepsy. Epilepsia 53(10):1739–1745. https://doi.org/10.1111/j.1528-1167.2012.03600.x
Fitzgerald Z, Morita-Sherman M, Hogue O et al (2021) Improving the prediction of epilepsy surgery outcomes using basic scalp eeg findings. Epilepsia 62(10):2439–2450. https://doi.org/10.1111/epi.17024
Jehi L, Yardi R, Chagin K et al (2015) Development and validation of nomograms to provide individualised predictions of seizure outcomes after epilepsy surgery: a retrospective analysis. Lancet Neurol 14(3):283–290. https://doi.org/10.1016/S1474-4422(14)70325-4
Remi J, Shen S, Tacke M et al (2020) Congruence and discrepancy of interictal and ictal eeg with mri lesions in pediatric epilepsies. Clin EEG Neurosci 51(6):412–419. https://doi.org/10.1177/1550059420921712
Sainju RK, Wolf BJ, Bonilha L, Martz G (2012) Relationship of number of seizures recorded on video-eeg to surgical outcome in refractory medial temporal lobe epilepsy. Arq Neuropsiquiatr 70(9):694–699. https://doi.org/10.1590/s0004-282x2012000900009
So EL (2006) Value and limitations of seizure semiology in localizing seizure onset. J Clin Neurophysiol 23(4):353–357. https://doi.org/10.1097/01.wnp.0000228498.71365.7b
Funding
This work was supported by the National Natural Science Foundation of China (Program No. 82371459) and the Innovation Capability Support Program of Shaanxi (Program No. 2021LCZX-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Ethics Committee of the First Affiliated Hospital of **’an Jiaotong University.
Consent for publication
All authors consent to the publication of this manuscript.
Conflict of interest
The authors declare no competing interests.
dsfd
Informed consent
Patients signed informed consent regarding publishing their data and photographs. Authors are responsible for correctness of the statements provided in the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, H., Meng, Q., Liu, Y. et al. The value of ictal scalp EEG in focal epilepsies surgery: a retrospective analysis. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07657-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07657-8