Abstract
Introduction/objective
Knee alignment and anterior cruciate ligament (ACL) injury are risk factors for knee osteoarthritis (OA). The objective was to examine interactions between knee alignment and ACL status on cartilage volume loss in participants with or at risk of knee OA.
Method
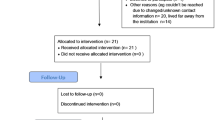
Participants were from the Osteoarthritis Initiative, a longitudinal cohort study. Data were from baseline and 24- and 72-month follow-up visits. Participants with knee OA (progression subcohort) or at risk of knee OA (incidence subcohort) that had partial or full ACL tears (OA-ACL group; n=66) or an intact ACL (OA-only group, n=367) were selected. Femur-tibia angles from radiographs quantified knee alignment. Changes in tibial and femoral cartilage volumes were measured using magnetic resonance imaging. Hierarchical linear models examined if knee alignment, presence of ACL, and their interaction were related to cartilage volume loss after accounting for other variables.
Results
Interactions between alignment and ACL status were significantly related to cartilage volume loss in the lateral plateau (β=−20.19, 95% confidence interval [CI]=−34.65 to −5.73) and lateral condyle (β=−23.64, 95%CI=−43.06 to −4.23). Valgus alignment was related to lateral compartment cartilage loss in the OA-ACL group, but not in the OA-only group. Varus alignment was related to cartilage loss in the medial plateau (β=7.49, 95%CI=0.17 to 14.80) and medial condyle (β=19.70, 95%CI=5.96 to 33.44) in both groups.
Conclusion
The impact of knee alignment on knee OA initiation and progression varies based on ACL status. Initial lateral compartment damage or changes in joint kinematics after ACL rupture might account for these findings.
Key Points • The relationship between knee alignment and lateral compartment cartilage loss depended on the status of the anterior cruciate ligament in participants with knee osteoarthritis or at risk for knee osteoarthritis. • Valgus alignment was related to lateral compartment cartilage loss in participants with a deficient anterior cruciate ligament. • Varus alignment was related to medial compartment cartilage loss regardless of the status of the anterior cruciate ligament. |



Similar content being viewed by others
Data availability
The datasets used in the current study are available through the Osteoarthritis Initiative website: https://nda.nih.gov/oai/.
References
Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, Fang F, Schwartz TA, Abbate LM, Callahan LF, Kalsbeek WD, Hochberg MC (2007) Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol 34(1):172–180
Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M (2010) Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis 69(11):1940–1945. https://doi.org/10.1136/ard.2010.129742
Felson DT, Niu J, Gross KD, Englund M, Sharma L, Cooke TD, Guermazi A, Roemer FW, Segal N, Goggins JM, Lewis CE, Eaton C, Nevitt MC (2013) Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheum 65(2):355–362. https://doi.org/10.1002/art.37726
Yang NH, Nayeb-Hashemi H, Canavan PK, Vaziri A (2010) Effect of frontal plane tibiofemoral angle on the stress and strain at the knee cartilage during the stance phase of gait. J Orthop Res 28(12):1539–1547. https://doi.org/10.1002/jor.21174
Bennell KL, Bowles KA, Wang Y, Cicuttini F, Davies-Tuck M, Hinman RS (2011) Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis 70(10):1770–1774. https://doi.org/10.1136/ard.2010.147082
Muthuri SG, McWilliams DF, Doherty M, Zhang W (2011) History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthr Cartil 19(11):1286–1293. https://doi.org/10.1016/j.joca.2011.07.015
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50(10):3145–3152. https://doi.org/10.1002/art.20589
Andriacchi TP, Koo S, Scanlan SF (2009) Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am 91(suppl 1):95–101. https://doi.org/10.2106/JBJS.H.01408
Riordan EA, Little C, Hunter D (2014) Pathogenesis of post-traumatic OA with a view to intervention. Best Pract Res Clin Rheumatol 28(1):17–30. https://doi.org/10.1016/j.berh.2014.02.001
Andriacchi TP, Favre J, Erhart-Hledik JC, Chu CR (2015) A systems view of risk factors for knee osteoarthritis reveals insights into the pathogenesis of the disease. Ann Biomed Eng 43(2):376–387. https://doi.org/10.1007/s10439-014-1117-2
Andriacchi TP, Dyrby CO (2005) Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech 38(2):293–298. https://doi.org/10.1016/j.jbiomech.2004.02.010
Osteoarthritis Initiative (2017) Osteoarthritis Initiative a knee healthy study. https://oai.epi-ucsf.org/datarelease/. Accessed August 10, 2017
Collins JE, Losina E, Nevitt MC, Roemer FW, Guermazi A, Lynch JA, Katz JN, Kent Kwoh C, Kraus VB, Hunter DJ (2016) Semiquantitative imaging biomarkers of knee osteoarthritis progression: data from the Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis Rheum 68(10):2422–2431. https://doi.org/10.1002/art.39731
Roemer FW, Kwoh CK, Hannon MJ, Hunter DJ, Eckstein F, Fujii T, Boudreau RM, Guermazi A (2015) What comes first? Multitissue involvement leading to radiographic osteoarthritis: magnetic resonance imaging-based trajectory analysis over four years in the Osteoarthritis Initiative. Arthritis Rheum 67(8):2085–2096. https://doi.org/10.1002/art.39176
Wise BL, Niu J, Guermazi A, Liu F, Heilmeier U, Ku E, Lynch JA, Zhang Y, Felson DT, Kwoh CK, Lane NE (2017) Magnetic resonance imaging lesions are more severe and cartilage T2 relaxation time measurements are higher in isolated lateral compartment radiographic knee osteoarthritis than in isolated medial compartment disease - data from the Osteoarthritis Initiative. Osteoarthr Cartil 25(1):85–93. https://doi.org/10.1016/j.joca.2016.08.002
Peterfy CG, Schneider E, Nevitt M (2008) The Osteoarthritis Initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthr Cartil 16(12):1433–1441. https://doi.org/10.1016/j.joca.2008.06.016
Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, Roemer FW (2011) Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthr Cartil 19(8):990–1002. https://doi.org/10.1016/j.joca.2011.05.004
Dodin P, Pelletier JP, Martel-Pelletier J, Abram F (2010) Automatic human knee cartilage segmentation from 3D magnetic resonance images. IEEE Trans Biomed Eng 57(11):2699–2711. https://doi.org/10.1109/TBME.2010.2058112.doi:10.1109/TBME.2010.2058112
Martel-Pelletier J, Roubille C, Abram F, Hochberg MC, Dorais M, Delorme P, Raynauld JP, Pelletier JP (2015) First-line analysis of the effects of treatment on progression of structural changes in knee osteoarthritis over 24 months: data from the Osteoarthritis Initiative progression cohort. Ann Rheum Dis 74(3):547–556. https://doi.org/10.1136/annrheumdis-2013-203906
Nevitt MC, Peterfy C, Guermazi A, Felson DT, Duryea J, Woodworth T, Chen H, Kwoh K, Harris TB (2007) Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum 56(5):1512–1520. https://doi.org/10.1002/art.22557
Iranpour-Boroujeni T, Li J, Lynch JA, Nevitt M, Duryea J (2014) A new method to measure anatomic knee alignment for large studies of OA: data from the Osteoarthritis Initiative. Osteoarthr Cartil 22(10):1668–1674. https://doi.org/10.1016/j.joca.2014.06.011
Moyer R, Wirth W, Duryea J, Eckstein F (2016) Anatomical alignment, but not goniometry, predicts femorotibial cartilage loss as well as mechanical alignment: data from the Osteoarthritis Initiative. Osteoarthr Cartil 24(2):254–261. https://doi.org/10.1016/j.joca.2015.08.016
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Fagerland MW, Sandvik L (2009) Performance of five two-sample location tests for skewed distributions with unequal variances. Contemp Clin Trials 30(5):490–496. https://doi.org/10.1016/j.cct.2009.06.007
Singer JD, Willett JB (2003) Applied longitudinal data analysis: modeling change and event occurrence. Oxford University Press, New York
Wang J, **e H, Fisher J (2011) Multilevel models: applications using SAS. De Gruyter, Berlin
Sharma L, Eckstein F, Song J, Guermazi A, Prasad P, Kapoor D, Cahue S, Marshall M, Hudelmaier M, Dunlop D (2008) Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum 58(6):1716–1726. https://doi.org/10.1002/art.23462
Cicuttini F, Wluka A, Hankin J, Wang Y (2004) Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology 43(3):321–324. https://doi.org/10.1093/rheumatology/keh017
Saliba CM, Brandon SCE, Deluzio KJ (2017) Sensitivity of medial and lateral knee contact force predictions to frontal plane alignment and contact locations. J Biomech 57:125–130. https://doi.org/10.1016/j.jbiomech.2017.03.005
Frobell RB, Roos HP, Roos EM, Hellio Le Graverand MP, Buck R, Tamez-Pena J, Totterman S, Boegard T, Lohmander LS (2008) The acutely ACL injured knee assessed by MRI: are large volume traumatic bone marrow lesions a sign of severe compression injury? Osteoarthr Cartil 16(7):829–836. https://doi.org/10.1016/j.joca.2007.11.003
Andriacchi TP, Mundermann A (2006) The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol 18(5):514–518. https://doi.org/10.1097/01.bor.0000240365.16842.4e
Zabala ME, Favre J, Andriacchi TP (2015) Relationship between knee mechanics and time since injury in ACL-deficient knees without signs of osteoarthritis. Am J Sports Med 43(5):1189–1196. doi. https://doi.org/10.1177/0363546514567296
Frank CB, Beveridge JE, Huebner KD, Heard BJ, Tapper JE, O'Brien EJ, Shrive NG (2012) Complete ACL/MCL deficiency induces variable degrees of instability in sheep with specific kinematic abnormalities correlating with degrees of early osteoarthritis. J Orthop Res 30(3):384–392. https://doi.org/10.1002/jor.21549
Eckstein F, Wirth W, Hudelmaier M, Stein V, Lengfelder V, Cahue S, Marshall M, Prasad P, Sharma L (2008) Patterns of femorotibial cartilage loss in knees with neutral, varus, and valgus alignment. Arthritis Rheum 59(11):1563–1570. https://doi.org/10.1002/art.24208
Birmingham TB, Moyer R, Leitch K, Chesworth B, Bryant D, Willits K, Litchfield R, Fowler PJ, Giffin JR (2017) Changes in biomechanical risk factors for knee osteoarthritis and their association with 5-year clinically important improvement after limb realignment surgery. Osteoarthr Cartil 25(12):1999–2006. https://doi.org/10.1016/j.joca.2017.08.017
Marriott K, Birmingham TB, Kean CO, Hui C, Jenkyn TR, Giffin JR (2015) Five-year changes in gait biomechanics after concomitant high tibial osteotomy and ACL reconstruction in patients with medial knee osteoarthritis. Am J Sports Med 43(9):2277–2285. https://doi.org/10.1177/0363546515591995
Johnson VL, Guermazi A, Roemer FW, Hunter DJ (2017) Comparison in knee osteoarthritis joint damage patterns among individuals with an intact, complete and partial anterior cruciate ligament rupture. Int J Rheum Dis 20(10):1361–1371. https://doi.org/10.1111/1756-185x.13003
Funding
Shawn Robbins is supported by the Arthritis Society (grant number YIS-14-065) and the Fonds de recherche du Québec – Santé (grant number 33107). The OAI is a public-private partnership comprised five contracts (N01-AR-2-2258; N01-AR-2-2259; N01AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health. Funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the Consortium and OAI is managed by the Foundation for the National Institutes of Health. Data provided from the FNIH OA Biomarkers Consortium Project made possible through grants and direct or in-kind contributions by the following: AbbVie; Amgen; Arthritis Foundation; Artialis; Bioiberica; BioVendor; DePuy; Flexion Therapeutics; GSK; IBEX; IDS; Merck Serono; Quidel; Rottapharm | Madaus; Sanofi; Stryker; the Pivotal OAI MRI Analyses (POMA) study, NIH HHSN2682010000 21C; and the Osteoarthritis Research Society International.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
Jean-Pierre Pelletier and Johanne Martel-Pelletier are shareholders in ArthroLab Inc. François Abram is an employee of ArthroLab Inc. There are no other conflicts of interest to report.
Ethical standards
Ethics approval for the OAI database was made by the Institutional Review Board of the University of California (approval number 10-00532) and from the clinical sites that participated in the study. Informed consent was obtained from participants during enrollment into the OAI.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A conference abstract based on this data and analysis has been published: Robbins S, Teoli A, Abram F, Pelletier JP, Martel-Pelletier J (2019) The effect of knee alignment on cartilage loss differs based on anterior cruciate ligament status in patients with or at risk of knee osteoarthritis: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 27(Suppl 1):S343.
Rights and permissions
About this article
Cite this article
Robbins, S.M., Raymond, N., Abram, F. et al. The effect of alignment on knee osteoarthritis initiation and progression differs based on anterior cruciate ligament status: data from the Osteoarthritis Initiative. Clin Rheumatol 38, 3557–3566 (2019). https://doi.org/10.1007/s10067-019-04759-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04759-z