Abstract
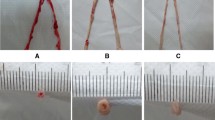
The objective of this study was to establish an animal model of arteriosclerosis for assessing vasospasm and to investigate the relationship between arteriosclerosis and vasospasm. Twelve-week-old male Sprague–Dawley rats were fed a diet supplemented with adenine and vitamin D (adenine/vitD). Body weight, blood, and femoral artery histopathology were assessed at 2, 4, and 6 weeks. Change in the femoral artery was examined by transmission electron microscope (TEM). Vasospasm was induced by administering epinephrine extravascularly into the femoral artery and released by the treatment with lidocaine as a vasodilator. During this period, the extravascular diameter and blood flow were measured. The rats in the adenine/vitD group developed renal dysfunction, uremia, hyperphosphatemia, and elevated serum alkaline phosphatase. Histological and TEM analyses of the femoral arteries in the treated rats revealed the degeneration of elastic fibers and extensive calcification of the tunica media and intima. Vascular smooth muscles were degenerated and osteoblasts were developed, resulting in calcified arteriosclerosis. Vasospasm in arteriosclerotic arteries was detected; however, vasodilation as well as an increase in the blood flow was not observed. This study revealed the development of vasospasm in the femoral arteries of the arteriosclerotic rats and, a conventional vasodilator did not release the vasospasm.










Similar content being viewed by others
References
Bartella AK, Luderich C, Kamal M et al (2020) Ankle Brachial Index predicts for difficulties in performing microvascular anastomosis. J Oral Maxillofac Surg 78:1020–1026
Chen HC, Coskunfirat OK, Ozkan O et al (2006) Guidelines for the optimization of microsurgery in atherosclerotic patients. Microsurgery 26:356–362
Cigna E, Torto FL, Parisi P, Felli A, Ribuffo D (2014) Management of microanastomosis in patients affected by vessel diseases. Eur Rev Med Pharmacol Sci 18(22):3399–3405
Bertelli JA, Mira JC (1994) Vascular freezing–a new method for immediate and permanent vasospasm relief: an experimental study in the rat. Plast Reconstr Surg 93:1041–1049
Hyza P, Streit L, Schwarz D, Kubek T, Vesely J (2014) Vasospasm of the flap pedicle: the effect of 11 of the most often used vasodilating drugs. Comparative study in a rat model. Plast Reconstr Surg 134(4):574–584
Yokoyama T, Kadota S, Takeuchi K et al (2011) Changes in the blood flow and prevention of vasospasm of the femoral artery by topical application of lidocaine in rats. Ann Plast Surg 67(2):178–183
Kunitomo M, Kinoshita K, Bandô Y (1981) Experimental atherosclerosis in rats fed a vitamin D, cholesterol-rich diet. J Pharmacobiodyn 4(9):718–723
Katsumata K, Kusano K, Hirata M et al (2003) Sevelamer hydrochloride prevents ectopic calcification and renal osteodystrophyin chronic renal failure rats. Kidney Int 64(2):441–450
Wang X, Wang F, Li N, Hu M, Chen Y, Tan M (2015) The effects of endothelial progenitor cells on rat atherosclerosis. Biotechnol Appl Biochem 62(2):186–192
Nagano N, Miyata S, Abe M, Wakita S, Kobayashi N, Wada M (2006) Sevelamer hydrochloride reverses parathyroid gland enlargement via regression of cell hypertrophy but not apoptosis in rats with chronic renal insufficiency. Nephrol Dial Transplant 21(3):634–643
Geter RK, Winters RR, Puckett CL (1986) Resolution of experimental microvascular spasm and improvement in anastomotic patency by direct topical agent application. Plast Reconstr Surg 77(1):105–115
Clemens MW, Higgins JP, Wilgis EFS (2009) Prevention of anastomotic thrombosis by botulinum toxin a in an animal model. Plast Reconstr Surg 123(1):64–70
Tanaka K, Hirata Y, Tabata Y, Ouchi Y, Sata M (2018) Locally applied suramin inhibits angiogenesis in adventitia and arterial lesion progression in apolipoprotein E-deficient mice. Circulation 126:A12181
McCullough PA, Agrawal V, Danielewicz E, Abela GS (2008) Accelerated atherosclerotic calcification and Mönckeberg’s sclerosis: a continuum of advanced vascular pathology in chronic kidney disease. Clin J Am Soc Nephrol 3(6):1585–1598
Koeda T, Wakaki K, Koizumi F, Yokozawa T, Oura H (1988) Early changes of proximal tubules in the kidney of adenine-ingesting rats, with special reference to biochemical and electron microscopic studies. Jpn J Nephrol 30:239–246
Okada H, Kaneko Y, Yawata T et al (1999) Reversibility of adenine-induced renal failure in rats. Clin Exp Nephrol 3:82–88
Yokozawa T, Zheng PD, OuraH KZ (1986) Animal model of adenine-induced chronic renal failure in rats. Nephron 44:230–234
Yokozawa T, Zheng PD, Oura H (1984) Biochemical features induced by adenine feeding in rats. Polyuria, electrolyte disorders, and 2, 8-dihydroxyadenine deposits. J Nutr Sci Vitaminol 30:245–254
Bellasi A, Mandreoli M, Baldrati L et al (2011) Chronic kidney disease progression and outcome according to serum phosphorus in mild-to-moderate kidney dysfunction. Clin J Am Soc Nephrol 6:883–891
Jono S, McKee MD, Murry CE et al (2000) Phosphate regulation of vascular smooth muscle cell calcification. Circ Res 87:e10–e17
Nuraly SA, Ilya D, Dinara KS, Mohammed SR (2022) Vitamin D and phosphate interactions in health and disease. Adv Exp Med Biol 1362:37–46
Mody N, Parhami F, Sarafian TA, Demer LL (2001) Oxidative stress modulates osteoblastic differentiation of vascular and bone cells. Free Radic Biol Med 31:509–519
Thyberg J (2000) Differences in caveolae dynamics in vascular smooth muscle cells of different phenotypes. Lab Invest 80(6):915–929
Caughey GE, Vitry AI, Gilbert AL, Roughead EE (2008) Prevalence of comorbidity of chronic diseases in Australia. BMC Public Health 8:221
Peters TT, Post SF et al (2015) Free flap reconstruction for head and neck cancer can be safely performed in both young and elderly patients after careful patient selection. Eur Arch Otorhinolaryngol 272:2999–3005
Ozkan O, Ozgentas HE, Islamoglu K, Boztug N, Bigat Z, Dikici MB (2005) Experiences with microsurgical tissue transfers in elderly patients. Microsurgery 25:390–395
Coskunfirat OK, Chen HC, Spanio S, Tang YB (2005) The safety of microvascular free tissue transfer in the elderly population. Plast Reconstr Surg 115:771–775
Perrot P, Floch RL, Waast FB, Bourdais L, Pannier M, Duteille F (2008) Free-flap reconstruction in the elderly patient. Ann Chir Plast Esthet 53:420–423
Serletti JM, Higgins JP, Moran S, Orlando GS (2000) Factors affecting outcome in free-tissue transfer in the elderly. Plast Reconstr Surg 106:66–70
Zhang ZD, Macdonald RL (2006) Contribution of the remodeling response to cerebral vasospasm. Neurol Res 28:713–720
Hong MK, Park SW, Lee CW et al (2000) Intravascular ultrasound findings of negative arterial remodeling at sites of focal coronary spasm in patients with vasospastic angina. Am Heart J 140(3):395–401
Yamagishi M, Miyatake K, Tamai J, Nakatani S, Koyama J, Nissen SE (1994) Intravascular ultrasound detection of atherosclerosis at the site of focal vasospasm in angiographically normal or minimally narrowed coronary segments. J Am Coll Cardiol 23:352–357
Zhang Y, Janssen L, Chu FV (2005) Atherosclerosis of radial arterial graft may increase the potential of vessel spasm in coronary bypass surgery. J Thorac Cardiovasc Surg 130(5):1477–1478
Wadström J, Gerdin B (1991) Modulatory effects of topically administered lidocaine and pentobarbital on traumatic vasospasm in the rabbit ear artery. Br J Plast Surg 44(5):341–347
Garfield E, Somlyo AP (1985) Structure of smooth muscle part of the contemporary biomedicine book series 5. Calcium Contractility. https://doi.org/10.1007/978-1-4612-5172-9_1
David PW. Vascular Smooth Muscle Structure and Function. In Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists 7: 13–24, 2011
Acknowledgements
The authors are grateful to Dr. S. Taketani for providing invaluable advice. This work was supported in part by grants from the Ministry of Education, Science, Sports and Culture of Japan (Approval No. 21K09809).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval and consent to participate
The study was approved by the Ethics Review Board of Kansai Medical University in accordance with the ethical guidelines of the Helsinki Declaration of 1975. All specimens were collected and used with informed consent from the donors.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsuoka, Y., Fukui, M., Hihara, M. et al. Ultrastructural changes of vascular smooth muscle cells and resistance to vasospasm treatment in femoral arteries of an arteriosclerotic rat model. Med Mol Morphol 57, 45–58 (2024). https://doi.org/10.1007/s00795-023-00372-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00795-023-00372-x