Abstract
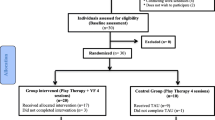
Telehealth services were rapidly adopted during the COVID-19 pandemic, but evidence regarding the effectiveness and feasibility of telehealth services in child and adolescent mental healthcare is sparse. This study aims to investigate feasibility, satisfaction, and goal attainment in video-delivered consultations in routine care child and adolescent psychiatry and psychotherapy. A total of 1046 patients from four university child and adolescent outpatient psychiatric clinics and one university outpatient unit for child and adolescent psychotherapy were screened for study participation. We examined a) the percentage of patients considered eligible for video-delivered consultation, b) clinicians’, parents’ and patients’ satisfaction with video consultation, c) clinicians’ ratings of goal attainment in video consultation, and d) factors associated with satisfaction and goal attainment. 59% of the screening sample (n = 621) fulfilled eligibility criteria and were considered eligible for video consultation. A total of 267 patients consented to participate in the study and received a video consultation. Clinicians reported high levels of satisfaction with video consultation and high levels of goal attainment in video consultations, especially for patients scheduled for initial patient assessments. Parents and patients were also highly satisfied with the video consultations, especially if patients had less severe emotional and behavioral problems. The present findings suggest that video consultations are a feasible and well-accepted alternative to in-person consultations in child and adolescent mental health care, especially for children with less severe symptoms and for children in early phases of assessment and treatment. Limitations include the lack of a control group. The study was registered at the German Clinical Trials Registry (DRKS00023525).

Similar content being viewed by others
Data availability
Data generated or analyzed during the study are available from the corresponding author by request.
References
Ravens-Sieberer U, Kaman A, Erhart M et al (2021) Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adoles Psychiat 31:879–889
Samji H, Wu J, Ladak A et al (2022) Review: mental health impacts of the covid-19 pandemic on children and youth—a systematic review. Child Adoles Ment Health 27:173–189
Treier AK, Holas V, Görtz-Dorten A et al (2023) Impact of the COVID-19 pandemic on children with and without affective dysregulation and their families. Eur Child Adolesc Psychiat 32:951–961
Wolf K, Schmitz J (2023) Sco** review: longitudinal effects of the COVID-19 pandemic on child and adolescent mental health. Eur Child Adolesc Psychiat. https://doi.org/10.1007/s00787-023-02206-8
Döpfner M, Adam J, Habbel C et al (2021) TEMPO-Studiengruppe, B-FAST-Studiengruppe. Die psychische Belastung Von Kindern, Jugendlichen und ihren Familien während Der COVID-19-Pandemie Und Der Zusammenhang Mit emotionalen und Verhaltensauffälligkeiten. Bundesgesundheitsbl 64:1522–1532
Holler A, Maldei-Gohring T, Reiß F, Oet (2023) COVID statt Kita - Der anhaltende Einfluss Der COVID-19 pandemie auf die psychische Gesundheit Von Vorschulkindern [COVID instead of daycare. The ongoing impact of the COVID-19 pandemic on preschoolers’ mental health]. Z Klin Psychol Psychother. https://doi.org/10.1026/1616-3443/a000692
Panchal U, Salazar de Pablo G, Franco M et al (2023) The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adoles Psychiat 32:1151–11771
Aafjes-van Doorn K, Békés V, Prout TA (2021) Grappling with our therapeutic relationship and professional self-doubt during COVID-19: will we use video therapy again? Counsel Psychol Quart 34:473–484
Obermann K, Brendt I, Hagen J et al (2020) Ärzte im Gesundheitsmarkt 2020: Ärztliche Arbeit und Nutzung von Videosprechstunden während der COVID-19-Pandemie, https://www.stiftung-gesundheit.de/pdf/studien/aerzte-im-zukunftsmarkt-gesundheit_2020_1.pdf assessed 13 June 2023)
McBeath AG, du Plock S, Bager-Charleson S (2020) The challenges and experiences of psychotherapists working remotely during the coronavirus pandemic. Couns Psychother Res 20:394–405
Fernandez E, Woldgabreal Y, Day A et al (2021) Live psychotherapy by video versus in-person: a meta-analysis of efficacy and its relationship to types and targets of treatment. Clin Psychol Psychother 28:1535–1549
Matsumoto K, Hamatani S, Shimizu E (2021) Effectiveness of videoconference-delivered cognitive behavioral therapy for adults with psychiatric disorders: Systematic and meta-analytic review. J Med Internet Res 23:e31293
Mazziotti R, Rutigliano G (2021) Tele-mental health for reaching out to patients in a time of pandemic: provider survey and meta-analysis of patient satisfaction. JMIR Ment Health 8:e26187
Li H, Glecia A, Kent-Wilkinson A et al (2022) Transition of mental health service delivery to telepsychiatry in response to COVID-19: a literature review. Psychiat Quart 93:181–197
Pogorzelska K, Chlabicz S (2022) Patient satisfaction with telemedicine during the COVID-19 pandemic – a systematic review. Int J Environ Res Pub Health 19:6113
American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Telepsychiatry and AACAP Committee on Quality Issues (2017) Clinical update: telepsychiatry with children and adolescents. J Am Acad Child Adolesc Psychiatry 56(10):875–893
Gloff N, Lenoue S, Novins D, Myers K (2015) Telemental health for children and adolescents. Int Rev Psychiatry 27:6513–6524
Thomas JF, Novins DK, Hosokawa PW et al (2018) The use of telepsychiatry to provide cost-efficient care during pediatric mental health emergencies. Psychiatric Serv 69(2):161–168
Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W (2015) Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Americ Acad Child Adolesc Psychiatry 54:263–274
Fox KC, Connor P, McCullers E, Waters T (2008) Effect of a behavioural health and specialty care telemedicine programme on goal attainment for youths in juvenile detention. J Telemed Telecare 14:227–230
Von Wirth E, Willems S, Döpfner M, Kohl LT (2023) Effectiveness of videoconference-delivered psychotherapy for children, adolescents, and their parents: A meta-analysis of randomized controlled trials. J Telemed Telecare. https://doi.org/10.1177/1357633X231199
Comer JS, Furr JM, Kerns CE et al (2017) Internet-delivered, family-based treatment for early-onset OCD: a pilot randomized trial. J Consulting Clin Psychol 85:178–186
Hollmann K, Hohnecker CS, Haigis A et al (2022) Internet-based cognitive behavioral therapy in children and adolescents with obsessive-compulsive disorder: a randomized controlled trial. Front Psychiat 13:989550
Nelson E, Barnard M, Cain S (2003) Treating childhood depression over videoconferencing. Telemed e-Health 9:49–55
Himle MB, Freitag M, Walther M et al (2012) A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav Res Ther 50:565–570
Prato A, Maugeri N, Chiarotti F et al (2022) A randomized controlled trial comparing videoconference vs. face-to-face delivery of behavior therapy for youths with Tourette syndrome in the time of COVID-19. Front Psychiat 24:862422
**e Y et al (2013) A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemed e-Health 19:1–8
Ricketts EJ, Goetz AR, Capriotti MR et al (2016) A randomized waitlist-controlled pilot trials of voice of internet protocol-delivered behavior therapy for youth with chronic tic disorders. J Telemed Telecare 22:153–162
Meininger L, Adam J, von Wirth E et al (2022) Cognitive-behavioral teletherapy for children and adolescents with mental disorders and their families during the COVID-19 pandemic: a survey on acceptance and satisfaction. Child Adolesc Psychiatry Ment Health 16:61
Von Wirth E, Meininger L, Adam J et al (2023) Satisfaction with videoconference-delivered CBT provided as part of a blended treatment approach for children and adolescents with mental disorders and their families during the COVID-19 pandemic: a follow-up survey among caregivers and therapists. J Telemed Telecare. https://doi.org/10.1177/1357633X231157103
Tajan N, Deves M, Potier R (2023) Tele-psychotherapy during the COVID-19 pandemic: a mini-review. Front Psychiatry 14:1060961
Di Fazio N, Morena D, Delogu G et al (2022) Mental health consequences of COVID-19 pandemic period in the European population: an institutional challenge. Int J Environ Res Pub Health 19(15):9347
Plötner M, Moldt K, In-Albon T, Schmitz J (2022) Einfluss Der COVID-19-Pandemie auf die ambulante psychotherapeutische Versorgung Von Kindern Und Jugendlichen. Psychother 67:469–477
Benton T, Njoroge WFM, Ng WYK (2022) Sounding the alarm for children’s mental health during the COVID-19 pandemic. JAMA Pediat 176:e216295
Omboni S, Padwal RS, Alessa T et al (2022) The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health 1:7–35
Döpfner M, Plück J, Kinnen C (2014) Manual deutsche Schulalter-Formen Der Child Behavior Checklist Von Thomas M. Achenbach. Elternfragebögen über das Verhalten Von Kindern Und Jugendlichen. CBCL/6-18R), Lehrerfragebögen über das Verhalten Von Kindern Und Jugendlichen (TRF/6-18R), Fragebogen für Jugendliche (YSR/11-18R). Hogrefe, Göttingen
Döpfner M, Görtz-Dorten A (2020) Corona Belastungsbogen. Unveröffentlicht, Klinik für Psychiatrie, Psychosomatik und Psychotherapie des Kindes- und Jugendalters an der Uniklinik Köln
Nikolaidis A, Paksarian D, Alexander L et al (2021) The Coronavirus health and impact survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Scie Rep 11:8139
Turchik J, Karpenko V, Ogles B et al (2010) Parent and adolescent satisfaction with mental health services: does it relate to youth diagnosis, age, gender, or treatment outcome? Community Ment Health J 46:282–288
Garland AF, Haine RA, Boxmeyer CL (2007) Determinates of youth and parent satisfaction in usual care psychotherapy. Eval Program Plan 30(1):45–54
Copeland VC, Koeske G, Greeno CG (2004) Child and mother client satisfaction questionnaire scores regarding mental health services: race, age, and gender correlates. Res Soc Work Pract 14(6):434–442
Viefhaus P, Döpfner M, Dachs L et al (2021) Parent- and therapist-rated treatment satisfaction following routine child cognitive-behavioral therapy. Eur Child Adolesc Psychiatry 30:427–439
Garland AF, Aarons GA, Saltzman MD, Kruse MI (2000) Correlates of adolescents’ satisfaction with mental health services. Ment Health Serv Res 2(3):127–139
Godley SH, Fiedler EM, Funk RR (1998) Consumer satisfaction of parents and their children with child/adolescent mental health services. Eval Program Plan 21(1):31–45
Zhou X, Edirippulige S, Bai X, Bambling M (2021) Are online mental health interventions for youth effective? A systematic review. J Telemed Telecare 27:638–666
Venturo-Conerly KE, Fitzpatrick OM, Horn RL, Ugueto AM, Weisz JR (2022) Effectiveness of youth psychotherapy delivered remotely: a meta-analysis. Americ Psycholog 77:71–84
Funding
This research was conducted as part of the collaborative research project egePan Unimed funded within the Network University Medicine by the German Federal Ministry of Education and Research (BMBF, funding code: 01KX2021). The funding body has no role in the design of the study and the collection, analysis, and interpretation of data, and in writing the manuscript. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MD and SB developed the initial study conception and design. Material preparation was performed by MD, JA and CG. All authors contributed to data collection. Data analysis was performed by EvW, MD, JA and CG. The first draft of the manuscript was written by EvW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval has been obtained for all study centers.
Informed consent
Verbal and written consent was obtained from children and parents/caregivers.
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Döpfner, M., von Wirth, E., Adam, J. et al. Feasibility, satisfaction, and goal attainment in routine telemedicine consultation in child and adolescent psychiatry and psychotherapy. Eur Child Adolesc Psychiatry (2024). https://doi.org/10.1007/s00787-024-02477-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-024-02477-9