Abstract
Objective
To perform an overview of systematic reviews (SR) assessing the impact of malocclusion treatments (Orthodontic Treatment — OT and/or Orthodontic Surgical Treatment — OST) on Oral Health-Related Quality of Life (OHRQoL).
Materials and methods
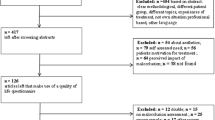
A search strategy was conducted in electronic databases until June 7th, 2021, followed by a manual search in grey literature and registration databases. Two independent authors applied the eligibility criteria, extracted the data, assessed the risk of bias (AMSTAR-2), and performed the certainty of evidence (GRADE) evaluation. Meta-analysis was planned to be carried out in RevMan 5.3 (with 95% confidence intervals (CI) considering p < 0.05), in case of homogeneous studies considering OHRQoL instrument and time of follow-up.
Results
A total of 126 articles were accessed on the database, 18 registers, 33 records on grey literature and 3 articles by means of citation searching. After duplicates removal and eligibility criteria analyses, 15 SR were included. From that, 13 showed improvement in OHRQoL after OT and/or OST. The methodological quality ranges from high (n = 2), to critically low (n = 9). Meta-analysis was conducted. Improvement on OHRQoL after a 6-month OST using the OQLQ–22 (p < 0.00001; 19.65; CI: 12.60–26.70) and OHIP–14 instruments (p < 0.00001; 10.70; CI: 9.89–11.51); and after a 6-month OT using the CPQ 11–14 instrument (p = 0.010; 3.57; CI: 0.86–6.28) with very low certainty of the evidence for all outcomes was observed.
Conclusions
Although most SR selected in this overview are characterized by a critically low quality, as well as very low certainty of the evidence, OT and/or OST seem to have a positive impact in improving the OHRQoL.
Clinical Relevance
The overview of existing systematic reviews compiled that OT and/or OST seem to have a positive impact on improving the OHRQoL. This information will facilitate clinical decision-making considering the clinical and psychological parameters.




Similar content being viewed by others
References
Obilade OA, Sanu OO, da Costa OO (2016) Impact of three malocclusion traits on the quality of life of orthodontic patients. Int Orthod 14(3):366–385. https://doi.org/10.1016/j.ortho.2016.07.003
Jago JD (1974) The epidemiology of dental occlusion; a critical appraisal. J Public Health Dent 34(2):80–93. https://doi.org/10.1111/j.1752-7325.1974.tb00682.x
Feu D, de Oliveira BH, de Oliveira Almeida MA, Kiyak HA, Miguel JAM (2010) Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofac Orthop 138(2):152–159. https://doi.org/10.1016/j.ajodo.2008.09.033
Chen M, Feng Z-C, Liu X, Li Z-M, Cai B, Wang D-W (2015) Impact of malocclusion on oral health-related quality of life in young adults. Angle Orthod 85(6):986–991. https://doi.org/10.2319/101714-743.1
Sischo L, Broder HL (2011) Oral health-related quality of life: what, why, how, and future implications. J Dent Res 90(11):1264–1270. https://doi.org/10.1177/0022034511399918
AlQuraini N, Shah R, Cunningham SJ (2019) Perceptions of outcomes of orthodontic treatment in adolescent patients: a qualitative study. Eur J Orthod 41(3):294–300. https://doi.org/10.1093/ejo/cjy071
Antunes LAA, Ornellas G, Fraga RS, Antunes LS (2018) Oral health outcomes: the association of clinical and socio-dental indicators to evaluate dental caries in preschool children. Cien Saude Colet 23(2):491–500. https://doi.org/10.1590/1413-81232018232.21022015
Zheng D-H, Wang X-X, Su Y-R, Zhao Y-R, Xu C, Kong C, Zhang J (2015) Assessing changes in quality of life using the Oral Health Impact Profile (OHIP) in patients with different classifications of malocclusion during comprehensive orthodontic treatment. BMC Oral Health 15:148. https://doi.org/10.1186/s12903-015-0130-7
Foster Page LA, Thomson WM, Jokovic A, Locker D (2005) Validation of the Child Perceptions Questionnaire (CPQ11-14). J Dent Res 84(7):649–652. https://doi.org/10.1177/154405910508400713
Mayo KH, Vig KD, Vig PS, Kowalski CJ (1991) Attitude variables of dentofacial deformity patients: demographic characteristics and associations. J Oral Maxillofac Surg 49(6):594–602. https://doi.org/10.1016/0278-2391(91)90341-i
Healey DL, Gauld RDC, Thomson WM (2016) Treatment-associated changes in malocclusion and oral health-related quality of life: a 4-year cohort study. Am J Orthod Dentofac Orthop 150(5):811–817. https://doi.org/10.1016/j.ajodo.2016.04.019
Lee S, McGrath C, Samman N (2008) Impact of orthognathic surgery on quality of life. J Oral Maxillofac Surg 66(6):1194–1199. https://doi.org/10.1016/j.joms.2008.01.006
Choi WS, Lee S, McGrath C (2010) Samman N (2010) Change in quality of life after combined orthodontic-surgical treatment of dentofacial deformities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109(1):46–51. https://doi.org/10.1016/j.tripleo.2009.08.019
Pelo S, Gasparini G, Garagiola U, Cordaro M, Di Nardo F, Staderini E, Patini R, de Angelis P, D’Amato G, Saponaro G, Moro A (2017) Surgery-first orthognathic approach vs traditional orthognathic approach: oral health-related quality of life assessed with 2 questionnaires. Am J Orthod Dentofac Orthop 152(2):250–254. https://doi.org/10.1016/j.ajodo.2016.12.022
Cheng LH, Roles D (1998) Telfer MR (1998) Orthognathic surgery: the patients’ perspective. Br J Oral Maxillofac Surg 36(4):261–263. https://doi.org/10.1016/s0266-4356(98)90709-4
Feu D, Miguel JAM, Celeste RK, Oliveira BH (2013) Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod 83(5):892–898. https://doi.org/10.2319/100412-781.1
Silvola A-S, Rusanen J, Tolvanen M, Pirttiniemi P, Lahti S (2012) Occlusal characteristics and quality of life before and after treatment of severe malocclusion. Eur J Orthod 34(6):704–709. https://doi.org/10.1093/ejo/cjr085
Maia NG, Normando D, Maia FA, Ferreira MAF, do Socorro Costa Feitosa Alves M (2010) Factors associated with long-term patient satisfaction. Angle Orthod 80(6):1155–1158. https://doi.org/10.2319/120909-708.1
Agou S, Locker D, Muirhead V, Tompson B, Streiner DL (2011) Does psychological well-being influence oral-health-related quality of life reports in children receiving orthodontic treatment? Am J Orthod Dentofac Orthop 139(3):369–377. https://doi.org/10.1016/j.ajodo.2009.05.034
Murphy C, Kearns G, Sleeman D, Cronin M, Allen PF (2011) The clinical relevance of orthognathic surgery on quality of life. Int J Oral Maxillofac Surg 40(9):926–930. https://doi.org/10.1016/j.ijom.2011.04.001
Kurabe K, Kojima T, Kato Y, Saito I, Kobayashi T (2016) Impact of orthognathic surgery on oral health-related quality of life in patients with jaw deformities. Int J Oral Maxillofac Surg 45(12):1513–1519. https://doi.org/10.1016/j.ijom.2016.07.003
Bertolini F, Russo V, Sansebastiano G (2000) Pre- and postsurgical psycho-emotional aspects of the orthognathic surgery patient. Int J Adult Orthodon Orthognath Surg 15(1):16–23
Pollock M, Fernandes RM, Becker LA, Featherstone R, Hartling L (2016) What guidance is available for researchers conducting overviews of reviews of healthcare interventions? A sco** review and qualitative metasummary. Syst Rev 5(1):190. https://doi.org/10.1186/s13643-016-0367-5
Hunt OT, Johnston CD, Hepper PG, Burden DJ (2001) The psychosocial impact of orthognathic surgery: a systematic review. Am J Orthod Dentofac Orthop 120(5):490–497. https://doi.org/10.1067/mod.2001.118402
Meger MN, Fatturi AL, Gerber JT, Weiss SG, Rocha JS, Scariot R, Wambier LM (2021) Impact of orthognathic surgery on quality of life of patients with dentofacial deformity: a systematic review and meta-analysis. Br J Oral Maxillofac Surg 59(3):265–271. https://doi.org/10.1016/j.bjoms.2020.08.014
Pachêco-Pereira C, Pereira JR, Dick BD, Perez A, Flores-Mir C (2015) Factors associated with patient and parent satisfaction after orthodontic treatment: a systematic review. Am J Orthod Dentofac Orthop 148(4):652–659. https://doi.org/10.1016/j.ajodo.2015.04.039
Macey R, Thiruvenkatachari B, O’Brien K, Batista KBSL (2020) Do malocclusion and orthodontic treatment impact oral health? A systematic review and meta-analysis. Am J Orthod Dentofac Orthop 157(6):738-744.e10. https://doi.org/10.1016/j.ajodo.2020.01.015
Yao K, Zhu G, Chen M, Zhang B, Wu Y, Li P (2020) Effect of surgery-first orthognathic approach on oral health-related quality of life: a systematic review. Angle Orthod 90(5):723–733. https://doi.org/10.2319/112619-749.1
Mandava P, Singaraju GS, Obili S, Nettam V, Vatturu S, Erugu S (2021) Impact of self-esteem on the relationship between orthodontic treatment and the oral health-related quality of life in patients after orthodontic treatment - a systematic review. Med Pharm Rep 94(2):158–69. https://doi.org/10.15386/mpr-1843
Andiappan M, Gao W, Bernabé E, Kandala NB, Donaldson AN (2015) Malocclusion, orthodontic treatment, and the Oral Health Impact Profile (OHIP-14): systematic review and meta-analysis. Angle Orthod 85(3):493–500. https://doi.org/10.2319/051414-348.1
Piassi E, Antunes LS, Antunes LAA (2016) Orthodontic treatment reduces the impact on children and adolescents’ oral health-related quality of life. Indian J Dent Res 27(2):213–219. https://doi.org/10.4103/0970-9290.183122
Soh CL, Narayanan V (2013) Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery - a systematic review. Int J Oral Maxillofac Surg 42(8):974–980. https://doi.org/10.1016/j.ijom.2013.03.023
Zhou Y, Wang Y, Wang X, Voliere G, Hu R (2014) The impact of orthodontic treatment on the quality of life a systematic review. BMC Oral Health 14:66. https://doi.org/10.1186/1472-6831-14-66
Javidi H, Vettore M, Benson PE (2017) Does orthodontic treatment before the age of 18 years improve oral health-related quality of life? A systematic review and meta-analysis. Am J Orthod Dentofac Orthop 151(4):644–655. https://doi.org/10.1016/j.ajodo.2016.12.011
Broers DLM, van der Heijden GJMG, Rozema FR, de Jongh A (2017) Do patients benefit from orthognathic surgery? A systematic review on the effects of elective orthognathic surgery on psychosocial functioning and patient satisfaction. Eur J Oral Sci 125(6):411–418. https://doi.org/10.1111/eos.12371
Yi J, Lu W, **ao J, Li X, Li Y, Zhao Z (2019) Effect of conventional combined orthodontic-surgical treatment on oral health-related quality of life: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 156(1):29-43.e5. https://doi.org/10.1016/j.ajodo.2019.03.008
Zamboni R, de Moura FR, Brew MC, Rivaldo EG, Braz MA, Grossmann E, Bavaresco CS (2019) Impacts of orthognathic surgery on patient satisfaction, overall quality of life, and oral health-related quality of life: a systematic literature review. Int J Dent 16https://doi.org/10.1155/2019/2864216
Ferrando-Magraner E, García-Sanz V, Bellot-Arcís C, Montiel-Company J-M, Almerich-Silla J-M, Paredes-Gallardo V (2019) Oral health-related quality of life of adolescents after orthodontic treatment A systematic review. J Clin Exp Dent 11(2):e194-202. https://doi.org/10.4317/jced.55527
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P (2015) Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 13(3):132–40. https://doi.org/10.1097/XEB.0000000000000055
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L (2013) Overviews of reviews (Chapter V). In: Deeks JJ, Higgins JPT AD. Cochrane Handbook for Systematic Reviews of Interventions.; Version 6.2 Available at: https://training.cochrane.org/handbook/current/chapter-v, Accessed Jan 20th 2022.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Deeks JJ, Higgins JPT AD (2019) CHAPTER 10: analysing data and undertaking meta-analyses. In: Cochrane Handbook for Systematic Reviews of Interventions. Available at: https://training.cochrane.org/handbook/current/chapter-10 , Accessed 15th Dec 2021
Schünemann H, Brożek J, Guyatt G OA (2013) GRADE handbook for grading quality of evidence and strength of recommendations. The GRADE Working Group. Available at: https://gdt.gradepro.org/app/handbook/handbook.html , Accessed 15th Dec 2021
Dimberg L, Arnrup K, Bondemark L (2015) The impact of malocclusion on the quality of life among children and adolescents: a systematic review of quantitative studies. Eur J Orthod 37(3):238–247. https://doi.org/10.1093/ejo/cju046
Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM (2015) The impact of malocclusions on oral health-related quality of life in children—a systematic review and meta-analysis. Clin Oral Invest 20(8):1881–1894. https://doi.org/10.1007/s00784-015-1681-3
Liu Z, McGrath C, Hägg U (2009) The impact of malocclusion/orthodontic treatment need on the quality of life. A systematic review Angle Orthod 79(3):585–591. https://doi.org/10.2319/042108-224.1
de Almeida AB, Leite ICG, Silva GA (2018) Evidence in Orthodontics related to qualitative research. Dental Press J Orthod 23(4):64–71. https://doi.org/10.1590/2177-6709.23.4.064-071.oar
Javidi H, Benson P (2015) The impact of malocclusion and its treatment on the oral health related quality of life of adults, assessed using the Oral Health Impact Profile (OHIP-14). Evid Based Dent 16(2):57–58. https://doi.org/10.1038/sj.ebd.6401100
Sun L, Wong HM, McGrath CPJ (2017) Relationship between the severity of malocclusion and oral health related quality of life: a systematic review and meta-analysis. Oral Health Prev Dent 15(6):503–517. https://doi.org/10.3290/j.ohpd.a38994
Sun L, Wong HM, McGrath CPJ (2018) Association between the severity of malocclusion, assessed by occlusal indices and oral health related quality of life: a systematic review and meta-analysis. Oral Health Prev Dent 16(3):211–223. https://doi.org/10.3290/j.ohpd.a40761
da Costa AC, Rodrigues FS, Heimer MV (2017) Self concept of dental aesthetics and its impact on the life of adolescents. Adolesc Saúde 14(4):157–166
Alanko OME, Svedström-Oristo AL, Tuomisto MT (2010) Patients’ perceptions of orthognathic treatment, well-being, and psychological or psychiatric status: a systematic review. Acta Odontol Scand 68(5):249–260. https://doi.org/10.3109/00016357.2010.494618
Feu D, Quintão CCA, Miguel JAM (2010) Quality of life instruments and their role in orthodontics. Dental Press J Orthod 15(6):61–70
Bo Z, Huang X, Huo S, Zhang C, Zhao S, Cen X et al (2020) Effect of clear aligners on oral health-related quality of life: a systematic review. Orthod Craniofac Res 23(4):363–370. https://doi.org/10.1111/ocr.12382
Gandedkar NH, Darendeliler MA (2020) Combined orthodontic-surgical treatment may be an effective choice to improve oral health—related quality of life for individuals affected with severe dentofacial deformities. J Evid Based Dent Pract 20(3):101462. https://doi.org/10.1016/j.jebdp.2020.101462
Nichersu A-R, Dragomirescu A-O, Manea M, Ionescu E (2020) The impact of malocclusions on the quality of life and psychological status A systematic review. Int J Med Dent 24(3):424–433
Abdullah WA (2015) Changes in quality of life after orthognathic surgery in Saudi patients. Saudi Dent J 27(3):161–164. https://doi.org/10.1016/j.sdentj.2014.12.001
Göelzer JG, Becker OE, Haas Junior OL, Scolari N, Santos Melo MF, Heitz C, de Oliveira RB (2014) Assessing change in quality of life using the Oral Health Impact Profile (OHIP) in patients with different dentofacial deformities undergoing orthognathic surgery: a before and after comparison. Int J Oral Maxillofac Surg 43(11):1352–1359. https://doi.org/10.1016/j.ijom.2014.06.015
Soh CL, Narayanan V (2015) The impact of surgical correction on the quality of life in patients with dentofacial deformity-a prospective study. J Oral Maxillofac Surgery Med Pathol 27(3):323–327. https://doi.org/10.1016/j.ajoms.2014.03.003
Baherimoghaddam T, Tabrizi R, Naseri N, Pouzesh A, Oshagh M, Torkan S (2016) Assessment of the changes in quality of life of patients with class II and III deformities during and after orthodontic-surgical treatment. Int J Oral Maxillofac Surg 45(4):476–485. https://doi.org/10.1016/j.ijom.2015.10.019
Alanko O, Tuomisto MT, Peltomäki T, Tolvanen M, Soukka T, Svedström-Oristo AL (2017) A longitudinal study of changes in psychosocial well-being during orthognathic treatment. Int J Oral Maxillofac Surg 46(11):1380–1386. https://doi.org/10.1016/j.ijom.2017.05.004
Benson PE, Da’as T, Johal A, Mandall NA, Williams AC, Baker SR, Marshman Z (2015) Relationships between dental appearance, self-esteem, socio-economic status, and oral health-related quality of life in UK schoolchildren: a 3-year cohort study. Eur J Orthod 37(5):481–90. https://doi.org/10.1093/ejo/cju076
Antoun JS, Fowler PV, Jack HC, Farella M (2015) Oral health-related quality of life changes in standard, cleft, and surgery patients after orthodontic treatment. Am J Orthod Dentofac Orthop 148(4):568–575. https://doi.org/10.1016/j.ajodo.2015.03.028
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3 Rating the quality of evidence. J Clin Epidemiol 64(4):401–6
Funding
This systematic review and meta-analysis study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001(Ribeiro), CNPq- Conselho Nacional de Desenvolvimento Científico e Tecnológico (Antunes/ Antunes) and by the Alexander von Humboldt Foundation (Küchler/Kirschneck accepted on July 4, 2019).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Luciana Gonçalves Ribeiro, Lívia Azeredo Alves Antunes, Ludmila Silva Guimarães, Flares Baratto-Filho, Erika Calvano Küchler and Leonardo Santos Antunes. The first draft of the manuscript was written by Luciana Gonçalves Ribeiro and Lívia Azeredo Alves Antunes. The final draft was written and revised by Lívia Azeredo Alves Antunes (systematic review methods), and Christian Kirschneck (orthodontics), and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Submission declaration
The work is part of academic thesis and has not been published previously.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro, L.G., Antunes, L.S., Küchler, E.C. et al. Impact of malocclusion treatments on Oral Health-Related Quality of Life: an overview of systematic reviews. Clin Oral Invest 27, 907–932 (2023). https://doi.org/10.1007/s00784-022-04837-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04837-8