Abstract
Objectives
We aimed to compare oral and pathogenic microorganisms in bloodstream infections (BSIs) in allogeneic hematopoietic stem cell transplantation (allo-HSCT). We also investigated the relationship between BSIs and oral mucositis to identify the ratio of BSIs caused by oral microorganisms and the pathogenic microorganisms involved.
Materials and methods
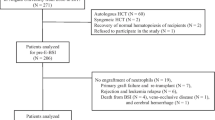
We collected data on BSIs in 96 patients who underwent allo-HSCT in our institute between April 2009 and December 2019, including BSI pathogens isolated from blood cultures (BBSIs) and microorganisms isolated from washing the oral cavity with sterile distilled water. Oral microorganisms obtained at the onset of BSI (OBSIs) and during allo-HSCT (OSCTs) were defined as isolates collected during the week of blood culturing. Study entry was limited to samples collected up to 1 month after allo-HSCT without BSI. When the BBSI and OBSI were the same, we considered the oral microorganism to have caused the BSI.
Results
The incidence rate of BSIs was 27%, and the predominant microorganism was coagulase-negative Staphylococci. Normal bacterial flora were decreased to 15.8% in OBSIs and 25.5% in OSCTs. The distribution of microorganisms without normal bacterial flora showed significant difference between BBSIs and OSCTs (p < 0.05). Oral mucositis was found in 72.9%, and BSI caused by oral microorganisms occurred in 46.2% of BSIs in allo-HSCT patients.
Conclusion
The distribution of microorganisms obtained from blood in patients with BSI during allo-HSCT was found to be similar to that of microorganisms from oral cultures.
Clinical relevance
Oral microorganism monitoring may be able to predict BSI during allo-HSCT.

Similar content being viewed by others
Data availability
Not applicable.
References
Montassier E, Batard E, Gastinne T, Potel G, de La Cochetière MF (2013) Recent changes in bacteremia in patients with cancer: a systematic review of epidemiology and antibiotic resistance. Eur J Clin Microbiol Infect Dis 32(7):841–850. https://doi.org/10.1007/s10096-013-1819-7
Islas-Munoz B, Volkow-Fernandez P, Ibanes-Gutierrez C, Villamar-Ramirez A, Vilar-Compte D, Cornejo-Juarez P (2018) Bloodstream infections in cancer patients. Risk factors associated with mortality. Int J Infect Dis 71:59–64. https://doi.org/10.1016/j.ijid.2018.03.022
Collin BA, Leather HL, Wingard JR, Ramphal R (2001) Evolution, incidence, and susceptibility of bacterial bloodstream isolates from 519 bone marrow transplant patients. Clin Infect Dis 33(7):947–953. https://doi.org/10.1086/322604
Misch EA, Andes DR (2019) Bacterial infections in the stem cell transplant recipient and hematologic malignancy patient. Infect Dis Clin N Am 33(2):399–445. https://doi.org/10.1016/j.idc.2019.02.011
Ge J, Yang T, Zhang L, Zhang X, Zhu X, Tang B, Wan X, Tong J, Song K, Yao W, Sun G, Sun Z, Liu H (2018) The incidence, risk factors and outcomes of early bloodstream infection in patients with malignant hematologic disease after unrelated cord blood transplantation: a retrospective study. BMC Infect Dis 18(1):654. https://doi.org/10.1186/s12879-018-3575-x
Mikulska M, Raiola AM, Galaverna F, Balletto E, Borghesi ML, Varaldo R, Gualandi F, Giannoni L, Pastori G, Giacobbe DR, Signori A, Del Bono V, Viscoli C, Bacigalupo A, Angelucci E (2018) Pre-engraftment bloodstream infections after allogeneic hematopoietic cell transplantation: impact of T cell-replete transplantation from a haploidentical donor. Biol Blood Marrow Transplant 24(1):109–118. https://doi.org/10.1016/j.bbmt.2017.08.024
Yan CH, Wang Y, Mo XD, Sun YQ, Wang FR, Fu HX, Chen Y, Han TT, Kong J, Cheng YF, Zhang XH, Xu LP, Liu KY, Huang XJ (2018) Incidence, risk factors, microbiology and outcomes of pre-engraftment bloodstream infection after haploidentical hematopoietic stem cell transplantation and comparison with HLA-identical sibling transplantation. Clin Infect Dis 67(suppl_2):S162–S173. https://doi.org/10.1093/cid/ciy658
Sorrig R, Klausen TW, Salomo M, Vangsted A, Gimsing P (2018) Risk factors for blood stream infections in multiple myeloma: a population-based study of 1154 patients in Denmark. Eur J Haematol 101(1):21–27. https://doi.org/10.1111/ejh.13066
Kameda K, Kimura SI, Akahoshi Y, Nakano H, Harada N, Ugai T, Wada H, Yamasaki R, Ishihara Y, Kawamura K, Sakamoto K, Ashizawa M, Sato M, Terasako-Saito K, Nakasone H, Kikuchi M, Yamazaki R, Kanda J, Kako S, Tanihara A, Nishida J, Kanda Y (2016) High incidence of afebrile bloodstream infection detected by surveillance blood culture in patients on corticosteroid therapy after allogeneic hematopoietic stem cell transplantation. Biology Blood Marrow Transplant 22(2):371–377. https://doi.org/10.1016/j.bbmt.2015.09.019
Villa A, Sonis ST (2016) Pharmacotherapy for the management of cancer regimen-related oral mucositis. Expert Opin Pharmacother 17(13):1801–1807. https://doi.org/10.1080/14656566.2016.1217993
Osakabe L, Utsumi A, Saito B, Okamatsu Y, Kinouchi H, Nakamaki T, Hironaka S (2017) Influence of Oral anaerobic bacteria on hematopoietic stem cell transplantation patients: oral mucositis and general condition. Transplant Proc 49(9):2176–2182. https://doi.org/10.1016/j.transproceed.2017.09.012
Raber-Durlacher JE, Laheij AM, Epstein JB, Epstein M, Geerligs GM, Wolffe GN, Blijlevens NM, Donnelly JP (2013) Periodontal status and bacteremia with oral viridans streptococci and coagulase negative staphylococci in allogeneic hematopoietic stem cell transplantation recipients: a prospective observational study. Support Care Cancer 21(6):1621–1627. https://doi.org/10.1007/s00520-012-1706-2
Soga Y, Maeda Y, Ishimaru F, Tanimoto M, Maeda H, Nishimura F, Takashiba S (2011) Bacterial substitution of coagulase-negative staphylococci for streptococci on the oral mucosa after hematopoietic cell transplantation. Support Care Cancer 19(7):995–1000. https://doi.org/10.1007/s00520-010-0923-9
Nagafuji K, Matsuo K, Teshima T, Mori S, Sakamaki H, Hidaka M, Ogawa H, Kodera Y, Kanda Y, Maruta A, Mori T, Yoshiba F, Ichinohe T, Kasai M, Takatsuka Y, Kubo K, Sao H, Atsuta Y, Suzuki R, Yoshida T, Tsuchida M, Harada M (2010) Peripheral blood stem cell versus bone marrow transplantation from HLA-identical sibling donors in patients with leukemia: a propensity score-based comparison from the Japan Society for Hematopoietic Stem Cell Transplantation registry. Int J Hematol 91(5):855–864. https://doi.org/10.1007/s12185-010-0581-1
Rubinstein P, Carrier C, Scaradavou A, Kurtzberg J, Adamson J, Migliaccio AR, Berkowitz RL, Cabbad M, Dobrila NL, Taylor PE, Rosenfield RE, Stevens CE (1998) Outcomes among 562 recipients of placental-blood transplants from unrelated donors. N Engl J Med 339(22):1565–1577. https://doi.org/10.1056/nejm199811263392201
Weinstein MP, Clinical, Laboratory Standards I (2019) Performance standards for antimicrobial susceptibility testing, vol M100, v. 40 , no.1. Clinical and Laboratory Standards Institute, 30th edn. Clinical and Laboratory Standards Institute,
Clinical, Laboratory Standards I, Wikler MA (2008) Performance standards for antimicrobial susceptibility testing : eighteenth informational supplement, vol M100-S18, v.28 , no.1. Clinical and Laboratory Standards Institute. Clinical and Laboratory Standards Institute,
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of America. Clin Infect Dis 52(4):e56–e93. https://doi.org/10.1093/cid/cir073
Gjaerde LI, Moser C, Sengelov H (2017) Epidemiology of bloodstream infections after myeloablative and non-myeloablative allogeneic hematopoietic stem cell transplantation: a single-center cohort study. Transpl Infect Dis 19(5). https://doi.org/10.1111/tid.12730
Elzi L, Babouee B, Vögeli N, Laffer R, Dangel M, Frei R, Battegay M, Widmer AF (2012) How to discriminate contamination from bloodstream infection due to coagulase-negative staphylococci: a prospective study with 654 patients. Clin Microbiol Infect 18(9):E355–E361. https://doi.org/10.1111/j.1469-0691.2012.03964.x
Davis R, Bryson HM (1994) Levofloxacin. A review of its antibacterial activity, pharmacokinetics and therapeutic efficacy. Drugs 47(4):677–700. https://doi.org/10.2165/00003495-199447040-00008
Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE (2005) Defining the normal bacterial flora of the oral cavity. J Clin Microbiol 43(11):5721–5732. https://doi.org/10.1128/jcm.43.11.5721-5732.2005
Timmers GJ, Dijstelbloem Y, Simoons-Smit AM, van Winkelhoff AJ, Touw DJ, Vandenbroucke-Grauls CM, Huijgens PC (2004) Pharmacokinetics and effects on bowel and throat microflora of oral levofloxacin as antibacterial prophylaxis in neutropenic patients with haematological malignancies. Bone Marrow Transplant 33(8):847–853. https://doi.org/10.1038/sj.bmt.1704431
Kiehlbauch JA, Hannett GE, Salfinger M, Archinal W, Monserrat C, Carlyn C (2000) Use of the National Committee for Clinical Laboratory Standards guidelines for disk diffusion susceptibility testing in New York state laboratories. J Clin Microbiol 38(9):3341–3348. https://doi.org/10.1128/jcm.38.9.3341-3348.2000
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39(3):309–317. https://doi.org/10.1086/421946
Al-Anazi KA, Al-Jasser AM (2014) Infections caused by Stenotrophomonas maltophilia in recipients of hematopoietic stem cell transplantation. Front Oncol 4:232. https://doi.org/10.3389/fonc.2014.00232
Harada K, Sekiya N, Konishi T, Nagata A, Yamada Y, Takezaki T, Kaito S, Kurosawa S, Sakaguchi M, Yasuda S, Sasaki S, Yoshioka K, Watakabe-Inamoto K, Igarashi A, Najima Y, Hagino T, Muto H, Kobayashi T, Doki N, Kakihana K, Sakamaki H, Ohashi K (2017) Predictive implications of albumin and C-reactive protein for progression to pneumonia and poor prognosis in Stenotrophomonas maltophilia bacteremia following allogeneic hematopoietic stem cell transplantation. BMC Infect Dis 17(1):638. https://doi.org/10.1186/s12879-017-2745-6
Labarca JA, Leber AL, Kern VL, Territo MC, Brankovic LE, Bruckner DA, Pegues DA (2000) Outbreak of Stenotrophomonas maltophilia bacteremia in allogenic bone marrow transplant patients: role of severe neutropenia and mucositis. Clin Infect Dis 30(1):195–197. https://doi.org/10.1086/313591
Vucicevic Boras V, Vidovic Juras D, Aurer I, Basic-Kinda S, Mikulic M (2019) Gingival ulcerations in a patient with acute myeloid leukemia: a case report and literature review. Acta Clin Croat 58(3):556–560. https://doi.org/10.20471/acc.2019.58.03.23
Miyairi I, Franklin JA, Andreansky M, Knapp KM, Hayden RT (2005) Acute necrotizing ulcerative gingivitis and bacteremia caused by Stenotrophomonas maltophilia in an immunocompromised host. Pediatr Infect Dis J 24(2):181–183. https://doi.org/10.1097/01.inf.0000151038.82538.de
Soga Y, Saito T, Nishimura F, Ishimaru F, Mineshiba J, Mineshiba F, Takaya H, Sato H, Kudo C, Kokeguchi S, Fujii N, Tanimoto M, Takashiba S (2008) Appearance of multidrug-resistant opportunistic bacteria on the gingiva during leukemia treatment. J Periodontol 79(1):181–186. https://doi.org/10.1902/jop.2008.070205
Taur Y, Xavier JB, Lipuma L, Ubeda C, Goldberg J, Gobourne A, Lee YJ, Dubin KA, Socci ND, Viale A, Perales MA, Jenq RR, van den Brink MR, Pamer EG (2012) Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis 55(7):905–914. https://doi.org/10.1093/cid/cis580
van der Meulen TA, Harmsen H, Bootsma H, Spijkervet F, Kroese F, Vissink A (2016) The microbiome-systemic diseases connection. Oral Dis 22(8):719–734. https://doi.org/10.1111/odi.12472
van Leeuwen SJM, Potting CMJ, Huysmans M, Blijlevens NMA (2019) Salivary changes before and after hematopoietic stem cell transplantation: a systematic review. Biol Blood Marrow Transplant 25(6):1055–1061. https://doi.org/10.1016/j.bbmt.2019.01.026
Delitto AE, Rocha F, Decker AM, Amador B, Sorenson HL, Wallet SM (2018) MyD88-mediated innate sensing by oral epithelial cells controls periodontal inflammation. Arch Oral Biol 87:125–130. https://doi.org/10.1016/j.archoralbio.2017.12.016
Funding
The work was supported by the Department of Oral and Maxillofacial Surgery, Faculty of Medicine, Kagawa University, Kagawa, Japan.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Osamu Imataki, Makiko Uemura, Akihiro Takeuchi, Saki Aoki, Mao Tanaka, Yasuhiro Nakai, Fumi Nakai, and Minoru Miyake. The first draft of the manuscript was written by Yumiko Ohbayashi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Yumiko Ohbayashi, Osamu Imataki, Makiko Uemura, Akihiro Takeuchi, Saki Aoki, Mao Tanaka, Yasuhiro Nakai, Fumi Nakai, and Minoru Miyake declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Kagawa University Ethical Committee (H24-#107). and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This study was a retrospective observational study, carried out by the opt-out method of our hospital website.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ohbayashi, Y., Imataki, O., Uemura, M. et al. Oral microorganisms and bloodstream infection in allogeneic hematopoietic stem cell transplantation. Clin Oral Invest 25, 4359–4367 (2021). https://doi.org/10.1007/s00784-020-03749-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03749-9