Abstract
Background
Sacroiliac joint dysfunction (SIJD) after lumbar/lumbosacral fusion has become increasingly recognized as the utilization of lumbar fusion has grown. Despite the significant morbidity associated with this condition, uncertainty regarding its diagnosis and treatment remains. We aim to update the current knowledge of the etiology, diagnosis, and treatment of post-lumbar surgery SIJD.
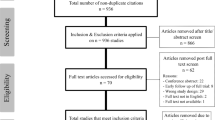
Methods
PRISMA guidelines were used to search the PubMed/Medline, Web of Science, Cochrane Reviews, Embase, and OVID databases for literature published in the last 10 years. The ROBIS tool was utilized for risk of bias assessment. Statistical analyses were performed using the R foundation. A Fisher’s exact test was performed to determine the risk of SIJD based on operative technique, gender, and symptom onset timeline. Odds ratios were reported with 95% confidence intervals. A p-value \(\le\) 0.05 was considered statistically significant.
Results
Seventeen publications were included. The incidence of new onset SIJD was 7.0%. The mean age was 56 years, and the follow-up length was 30 months. SIJD was more common with fixed lumbar fusion vs floating fusion (OR = 1.48 [0.92, 2.37], p = 0.083), fusion of \(\ge\) 3 segments (p < 0.05), and male gender increased incidence of SIJD (OR = 1.93 [1.27, 2.98], p = 0.001). Intra-articular injection decreased the Visual Analogue Scale (VAS) score by 75%, while radiofrequency ablation (RFA) reduced the score by 90%. An open approach resulted in a 13% reduction in VAS score versus 68 and 29% for SIJ fixation using the iFuse and DIANA approaches, respectively.
Conclusions
Lumbar fusion predisposes patients to SIJD, likely through manipulation of the SIJ’s biomechanics. Definitive diagnosis of SIJD remains multifaceted and a newer modality such as SPECT/CT may find a future role. When conservative measures are ineffective, RFA and SIJ fixation using the iFuse System yield the greatest improvement VAS and ODI.






Similar content being viewed by others
Data availability
This systematic review was not registered; however, a review protocol and data are available upon request.
Code availability
Not applicable.
Abbreviations
- SIJ:
-
Sacroiliac joint pain
- SIJD:
-
Sacroiliac joint dysfunction
- SIJP:
-
Sacroiliac joint pain
- VAS:
-
Visual Analogue Scale
- ODI:
-
Oswestry Disability Index
- SPECT/CT:
-
Single-photon emission computerized tomography
- MIS:
-
Minimally invasive
- RFA:
-
Radiofrequency ablation
- LBP:
-
Low back pain
- PT:
-
Pelvic tilt
- LL:
-
Lumbar lordosis
- SS:
-
Sacral slope
- PI:
-
Pelvic incidence
References
Ahlquist S, Park HY, Gatto J, Shamie AN, Park DY (2018) Does approach matter? A comparative radiographic analysis of spinopelvic parameters in single-level lumbar fusion. Spine J 18(11):1999–2008. https://doi.org/10.1016/j.spinee.2018.03.014
Al-Riyami K, Gnanasegaran G, Van den Wyngaert T, Bomanji J (2017) Bone SPECT/CT in the postoperative spine: a focus on spinal fusion. Eur J Nucl Med Mol Imaging 44(12):2094–2104. https://doi.org/10.1007/s00259-017-3765-6
Barros G, McGrath L, Gelfenbeyn M (2019) Sacroiliac joint dysfunction in patients with low back pain. Fed Pract 36(8):370–375
Buchanan P, Vodapally S, Lee DW, Hagedorn JM, Bovinet C, Strand N, Sayed D, Deer T (2021) Successful diagnosis of sacroiliac joint dysfunction. J Pain Res 14:3135–3143. https://doi.org/10.2147/JPR.S327351
Büker N, Akkaya S, Gökalp O, Kıtış A, Savkın R, Kıter AE (2014) Middle-term therapeutic effect of the sacroiliac joint blockade in patients with lumbosacral fusion-related sacroiliac pain. Acta Orthop Traumatol Turc 48(1):61–66. https://doi.org/10.3944/AOTT.2014.3190
Cheung JPY (2020) The importance of sagittal balance in adult scoliosis surgery. Ann Transl Med 8(2):35–35. https://doi.org/10.21037/atm.2019.10.19
Cho D-Y, Shin M-H, Hur J-W, Ryu K-S, Park C-K (2013) Sagittal sacropelvic morphology and balance in patients with sacroiliac joint pain following lumbar fusion surgery. J Korean Neurosurg Soc 54(3):201–206. https://doi.org/10.3340/jkns.2013.54.3.201
Ciarpaglini R, Maestretti G (2014) Sacroiliac Joint Syndrome 10 Years after Lumbar Arthroplasty: The Importance of Spinopelvic Alignment. Glob Spine J 23(6):720–724. https://doi.org/10.1007/s00586-014-3547-9
Colò G, Cavagnaro L, Alessio-Mazzola M, Zanirato A, Felli L, Formica M (2020) Incidence, diagnosis and management of sacroiliitis after spinal surgery: a systematic review of the literature. Musculoskelet Surg 104(2):111–123. https://doi.org/10.1007/s12306-019-00607-0
Crow WT, Willis DR (2009) Estimating cost of care for patients with acute low back pain: a retrospective review of patient records. J Am Osteopath Assoc 109(4):229–233. https://doi.org/10.7556/jaoa.2009.109.4.229
Cummings J, Capobianco RA (2013) Minimally invasive sacroiliac joint fusion: one-year outcomes in 18 patients. Ann Surg Innov Res 7(12):1–7. https://doi.org/10.1186/1750-1164-7-12
Deng H, Yue JK, Ordaz A, Suen CG, Sing DC (2021) Elective lumbar fusion in the United States: national trends in inpatient complications and cost from 2002–2014. J Neurosurg Sci 65(5):503–512. https://doi.org/10.23736/S0390-5616.19.04647-2
Endres S, Ludwig E (2013) Outcome of distraction interference arthrodesis of the sacroiliac joint for sacroiliac arthritis. Indian J Orthop 47(5):437–442. https://doi.org/10.4103/0019-5413.118197
Gartenberg A, Nessim A, Cho W (2021) Sacroiliac joint dysfunction: pathophysiology, diagnosis, and treatment. Eur Spine J 30(10):2936–2943. https://doi.org/10.1007/s00586-021-06927-9
Guan F, Sun Y, Zhu L, Guan G, Chen M, Chi Z, Tian D, Gu J, Yu Z (2018) Risk factors of postoperative sacroiliac joint pain for posterior lumbar surgery: ≥2-year follow-up retrospective study. World Neurosurg 110:546–551. https://doi.org/10.1016/j.wneu.2017.11.053
Hudyana H, Maes A, Vandenberghe T, Fidlers L, Sathekge M, Nicolai D, Van de Wiele C (2016) Accuracy of bone SPECT/CT for identifying hardware loosening in patients who underwent lumbar fusion with pedicle screws. Eur J Nucl Med Mol Imaging 43(2):349–354. https://doi.org/10.1007/s00259-015-3158-7
Jung MW, Schellhas K, Johnson B (2020) Use of diagnostic injections to evaluate sacroiliac joint pain. Int J Spine Surg 14(1):30–34. https://doi.org/10.14444/6081
Kalidindi KKV, Bansal K, Vishwakarma G, Chhabra HS (2021) New onset sacroiliac joint pain after transforaminal interbody fusion: what are the culprits? Glob Spine J 13(3):677–682. https://doi.org/10.1177/21925682211003852
Kim HS, Kim SH, Ju CI, Kim SW, Lee SM, Shin H (2010) The role of bone cement augmentation in the treatment of chronic symptomatic osteoporotic compression fracture. J Korean Neurosurg Soc 48(6):490–495
King W, Ahmed SU, Baisden J, Patel N, Kennedy DJ, MacVicar J, Duszynski B (2015) Diagnosis and treatment of posterior sacroiliac complex pain: a systematic review with comprehensive analysis of the published data. Pain Med 16(2):257–265
Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP (2021) Low back pain. Lancet Lond Engl 398(10294):78–92
Le Huec JC, Tsoupras A, Leglise A, Heraudet P, Celarier G, Sturresson B (2019) The sacro-iliac joint: a potentially painful enigma. Update on the diagnosis and treatment of pain from micro-trauma. Orthop Traumatol Surg Res 105(1, Supplement):S31–S42
Lee YC, Lee R, Harman C (2019) The incidence of new onset sacroiliac joint pain following lumbar fusion. J Spine Surg Hong Kong 5(3):310–314
Loh E, Agur AM, Burnham RS (2022) Ultrasound-guided radiofrequency ablation for SI joint pain: an observational study. Interv Pain Med 1(3):100118
Matsuki Y, Mizogami M, Shigemi K (2017) Successful treatment of failed back surgery syndrome with an ultrasound-guided sacroiliac joint block: a report of two cases. Anaesth. Pain Intensive Care 21(4):479–481
Nessim A, Cho W, Yang XA, Applebaum A, Sekerak R, Brill S, Kim SY (2021) Infra-adjacent segment disease after lumbar fusion: an analysis of pelvic parameters. Spine 46(16):E888–E892
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev. https://doi.org/10.1186/s13643-016-0384-4
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Park J, Ham D-W, Kwon B-T, Park S-M, Kim H-J, Yeom JS (2020) Minimally invasive spine surgery: techniques, technologies, and indications. Asian Spine J 14(5):694–701
Pizones J, García-Rey E (2020) Pelvic motion the key to understanding spine–hip interaction. EFORT Open Rev 5(9):522–533
Rainov NG, Schneiderhan R, Heidecke V (2019) Triangular titanium implants for sacroiliac joint fusion. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 28(4):727–734
Savarese LG, Menezes-Reis R, Bonugli GP, da Herrero CFPS, Defino HLA, Nogueira-Barbosa MH (2020) Spinopelvic sagittal balance: what does the radiologist need to know? Radiol Bras 53(3):175–184
Slinkard N, Agel J, Swiontkowski MF (2013) Documentation of outcomes for sacroiliac joint fusion: does prior spinal fusion influence the outcome? Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(10):2318–2324
Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, Kleiner J, Mody MG, Shamie AN (2013) Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 7(1):14
Tonosu J, Kurosawa D, Nishi T, Ito K, Morimoto D, Musha Y, Ozawa H, Murakami E (2019) The association between sacroiliac joint-related pain following lumbar spine surgery and spinopelvic parameters: a prospective multicenter study. Eur Spine J 28(7):1603–1609
Tseng C, Chen K-T, Fong Y-C, Lin C-W, Sun L-W, Chen C-M, Wang G-C (2023) Biportal endoscopic radiofrequency ablation of the sacroiliac joint complex in the treatment of chronic low back pain: a technical note with 1-year follow-up. Diagn Basel Switz 13(2):229
Unoki E, Abe E, Murai H, Kobayashi T, Abe T (2016) Fusion of multiple segments can increase the incidence of sacroiliac joint pain after lumbar or lumbosacral fusion. Spine 41(12):999–1005
Unoki E, Miyakoshi N, Abe E, Kobayashi T, Abe T, Shimada Y (2017) Sacroiliac joint pain after multiple-segment lumbar fusion: a long-term observational study-non-fused sacrum vs. fused sacrum. Spine Surg Relat Res 1(2):90–95
Urits I, Burshtein A, Sharma M et al (2019) Low back pain, a comprehensive review: pathophysiology, diagnosis, and treatment. Curr Pain Headache Rep 23(3):23
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH (2012) The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat 221(6):537–567
Wang J, Zhang Q, Liu F, Yuan H, Zhang Y, Wang X, Li J (2022) Predicting the ideal apex of lumbar lordosis based on individual pelvic incidence and inflection point in asymptomatic adults. Front Surg 9:912357
Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, Davies P, Kleijnen J, Churchill R (2016) ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 69:225–234
Yao Z, Li L, Zhang P, Yang L, Bai X, Peng S, Lai Y (2022) Biomechanics evaluation of sacroiliac joint pain after lumbosacral fusion: a finite element analysis. J Orthop Res Off Publ Orthop Res Soc. https://doi.org/10.1002/jor.25411
Yoshihara H (2012) Sacroiliac joint pain after lumbar/lumbosacral fusion: current knowledge. Eur Spine J 21(9):1788–1796
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. HK and RR performed an independent blinded review of publications for inclusion. SP resolved any discrepancies as a third blinded reviewer. All the authors participated in the construction and revision of the manuscript, and all provided the final approval for submission.
Corresponding author
Ethics declarations
Ethics approval
The manuscript does not contain clinical studies or patient data.
Consent to participate
The manuscript does not contain clinical studies or patient data.
Consent for publication
The manuscript does not contain clinical studies or patient data.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karimi, H., Rodrigues, R., Patel, S. et al. A systematic review and update on diagnosis and treatment of new onset sacroiliac joint dysfunction after lumbar fusion. Acta Neurochir 166, 43 (2024). https://doi.org/10.1007/s00701-024-05918-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05918-1