Abstract
Background
Sepsis is a systemic, inflammatory response to infection associated with significant morbidity and mortality. There is a considerable lack of literature exploring sepsis in neurosurgery. We aimed to identify variables that were correlated with mortality and increased morbidity as defined by readmission and increased length of stay in postoperative neurosurgical patients that met a sepsis diagnosis.
Methods
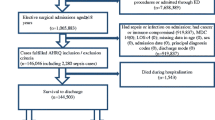
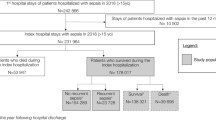
A retrospective chart review was conducted of 105 patients who underwent a neurosurgical operation at our institution from 2012 to 2017 who were discharged with at least one sepsis diagnosis code and who did not have a preoperative infection. We identified variables that were correlated with mortality, readmission, and increased length of stay.
Results
Patients who survived were preferentially distributed towards lower ASA Physical Status Classification scores. A larger percentage of patients who did not survive had cranial surgery, whereas patients who survived were more likely to have undergone spinal surgery. Higher respiratory rates, higher maximum lactic acid levels, positive sputum cultures, and lower incoming Glasgow Coma Scores (GCS) were significantly correlated with mortality. A larger fraction of readmitted patients had positive surgical site cultures but had negative sputum cultures. Length of hospitalization was correlated with incoming GCS, non-elective operations, and Foley catheter, arterial line, central line, and endotracheal tube duration.
Conclusions
Neurosurgical postoperative patients diagnosed with sepsis may be risk stratified for mortality, readmission, and increased length of stay based on certain variables that may help direct their care. Further prospective studies are needed to explore causal relationships.



Similar content being viewed by others
References
Abe T, Ogura H, Kushimoto S, Shiraishi A, Sugiyama T, Deshpande GA, Uchida M, Nagata I, Saitoh D, Fujishima S, Mayumi T, Hifumi T, Shiino Y, Nakada TA, Tarui T, Otomo Y, Okamoto K, Umemura Y, Kotani J, Sakamoto Y, Sasaki J, Shiraishi SI, Takuma K, Tsuruta R, Hagiwara A, Yamakawa K, Masuno T, Takeyama N, Yamashita N, Ikeda H, Ueyama M, Fujimi S, Gando S, group JF (2019) Variations in infection sites and mortality rates among patients in intensive care units with severe sepsis and septic shock in Japan. J Intensive Care 7:28. https://doi.org/10.1186/s40560-019-0383-3
Abouleish AE, Leib ML, Cohen NH (2015) ASA provides examples to each ASA Physical Status Class. ASA Newsletter 79:38–49
Angus DC, van der Poll T (2013) Severe sepsis and septic shock. N Engl J Med 369:840–851. https://doi.org/10.1056/NEJMra1208623
Arrighi-Allisan AE, Neifert SN, Gal JS, Deutsch BC, Caridi JM (2019) Discharge destination as a predictor of postoperative outcomes and readmission following posterior lumbar fusion. World Neurosurg 122:e139–e146. https://doi.org/10.1016/j.wneu.2018.09.147
Bakker J, Postelnicu R, Mukherjee V (2020) Lactate: where are we now? Crit Care Clin 36:115–124. https://doi.org/10.1016/j.ccc.2019.08.009
Bernatz JT, Anderson PA (2015) Thirty-day readmission rates in spine surgery: systematic review and meta-analysis. Neurosurg Focus 39:E7. https://doi.org/10.3171/2015.7.FOCUS1534
Bohl DD, Webb ML, Lukasiewicz AM, Samuel AM, Basques BA, Ahn J, Singh K, Vaccaro AR, Grauer JN (2015) Timing of complications after spinal fusion surgery. Spine (Phila Pa 1976) 40:1527–1535. https://doi.org/10.1097/BRS.0000000000001073
Buchanan IA, Donoho DA, Patel A, Lin M, Wen T, Ding L, Giannotta SL, Mack WJ, Attenello F (2018) Predictors of surgical site infection after nonemergent craniotomy: a nationwide readmission database analysis. World Neurosurg 120:e440–e452. https://doi.org/10.1016/j.wneu.2018.08.102
Burton BN, Hu JQ, Jafari A, Urman RD, Dunn IF, Bi WL, DeConde AS, Gabriel RA (2018) An updated assessment of morbidity and mortality following skull base surgical approaches. Clin Neurol Neurosurg 171:109–115. https://doi.org/10.1016/j.clineuro.2018.06.015
Cardozo Junior LC, Silva RR (2014) Sepsis in intensive care unit patients with traumatic brain injury: factors associated with higher mortality. Rev Bras Ter Intensiva 26:148–154. https://doi.org/10.5935/0103-507x.20140022
Chang DW, Tseng CH, Shapiro MF (2015) Rehospitalizations Following sepsis: common and costly. Crit Care Med 43:2085–2093. https://doi.org/10.1097/CCM.0000000000001159
Corral L, Javierre CF, Ventura JL, Marcos P, Herrero JI, Manez R (2012) Impact of non-neurological complications in severe traumatic brain injury outcome. Crit Care 16:R44. https://doi.org/10.1186/cc11243
Cutler NS (2020) Diagnosing sepsis: qSOFA is not the tool we’re looking for. Am J Med 133:265–266. https://doi.org/10.1016/j.amjmed.2019.07.048
Dasenbrock HH, Liu KX, Devine CA, Chavakula V, Smith TR, Gormley WB, Dunn IF (2015) Length of hospital stay after craniotomy for tumor: a National Surgical Quality Improvement Program analysis. Neurosurg Focus 39:E12. https://doi.org/10.3171/2015.10.FOCUS15386
Dasenbrock HH, Smith TR, Rudy RF, Gormley WB, Aziz-Sultan MA, Du R (2018) Reoperation and readmission after clip** of an unruptured intracranial aneurysm: a National Surgical Quality Improvement Program analysis. J Neurosurg 128:756–767. https://doi.org/10.3171/2016.10.JNS161810
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R, Surviving Sepsis Campaign Guidelines Committee including the Pediatric S (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41:580–637. https://doi.org/10.1097/CCM.0b013e31827e83af
Deyo RA, Hickam D, Duckart JP, Piedra M (2013) Complications after surgery for lumbar stenosis in a veteran population. Spine (Phila Pa 1976) 38:1695–1702. https://doi.org/10.1097/BRS.0b013e31829f65c1
Donoho DA, Wen T, Babadjouni RM, Schwartzman W, Buchanan IA, Cen SY, Zada G, Mack WJ, Attenello FJ (2018) Predictors of 30- and 90-day readmission following craniotomy for malignant brain tumors: analysis of nationwide data. J Neurooncol 136:87–94. https://doi.org/10.1007/s11060-017-2625-3
Elias AC, Matsuo T, Grion CM, Cardoso LT, Verri PH (2012) Incidence and risk factors for sepsis in surgical patients: a cohort study. J Crit Care 27:159–166. https://doi.org/10.1016/j.jcrc.2011.08.001
Elixhauser A, Friedman B, Stranges E (2011) Septicemia in U.S. Hospitals, 2009: Statistical Brief #122. In: Healthcare Cost and Utilization Project (HCUP) statistical briefs. Rockville (MD). https://www.ncbi.nlm.nih.gov/books/NBK65391. Accessed 5 Jan 2020
Elsamadicy AA, Sergesketter A, Adogwa O, Ongele M, Gottfried ON (2018) Complications and 30-day readmission rates after craniotomy/craniectomy: a single Institutional study of 243 consecutive patients. J Clin Neurosci 47:178–182. https://doi.org/10.1016/j.jocn.2017.09.021
Fu KM, Smith JS, Polly DW Jr, Ames CP, Berven SH, Perra JH, RE MC, Knapp DR Jr, Shaffrey CI, Scoliosis Research Society M, Mortality C (2011) Correlation of higher preoperative American Society of Anesthesiology grade and increased morbidity and mortality rates in patients undergoing spine surgery. J Neurosurg Spine 14:470–474. https://doi.org/10.3171/2010.12.SPINE10486
Giannakopoulos K, Hoffmann U, Ansari U, Bertsch T, Borggrefe M, Akin I, Behnes M (2017) The use of biomarkers in sepsis: a systematic review. Curr Pharm Biotechnol 18:499–507. https://doi.org/10.2174/1389201018666170601080111
Jiang J, Yang J, Mei J, ** Y, Lu Y (2018) Head-to-head comparison of qSOFA and SIRS criteria in predicting the mortality of infected patients in the emergency department: a meta-analysis. Scand J Trauma Resusc Emerg Med 26:56. https://doi.org/10.1186/s13049-018-0527-9
Karhade AV, Vasudeva VS, Dasenbrock HH, Lu Y, Gormley WB, Groff MW, Chi JH, Smith TR (2016) Thirty-day readmission and reoperation after surgery for spinal tumors: a National Surgical Quality Improvement Program analysis. Neurosurg Focus 41:E5. https://doi.org/10.3171/2016.5.FOCUS16168
Koo AB, Elsamadicy AA, David WB, Zogg CK, Santarosa C, Sujijantarat N, Robert SM, Kundishora AJ, Cord BJ, Hebert R, Bahrassa F, Malhotra A, Matouk CC (2020) Thirty- and 90-day readmissions after treatment of traumatic subdural hematoma: a national trend analysis. World Neurosurg. https://doi.org/10.1016/j.wneu.2020.03.168
Li H, Shan-Shan Z, Jian-Qiang K, Ling Y, Fang L (2020) Predictive value of C-reactive protein and NT-pro-BNP levels in sepsis patients older than 75 years: a prospective, observational study. Aging Clin Exp Res 32:389–397. https://doi.org/10.1007/s40520-019-01244-0
Lopez Ramos C, Brandel MG, Rennert RC, Wali AR, Steinberg JA, Santiago-Dieppa DR, Burton BN, Pannell JS, Olson SE, Khalessi AA (2018) Clinical risk factors and postoperative complications associated with unplanned hospital readmissions after cranial neurosurgery. World Neurosurg 119:e294–e300. https://doi.org/10.1016/j.wneu.2018.07.136
Mahboubi H, Haidar YM, Moshtaghi O, Ziai K, Ghavami Y, Maducdoc M, Lin HW, Djalilian HR (2016) Postoperative complications and readmission rates following surgery for cerebellopontine angle schwannomas. Otol Neurotol 37:1423–1427. https://doi.org/10.1097/MAO.0000000000001178
Malik AT, Jain N, Scharschmidt TJ, Mayerson JL, Khan SN (2018) Factors associated with post-operative sepsis following surgery for spinal tumors: an analysis of the ACS-NSQIP database. Clin Neurol Neurosurg 172:1–7. https://doi.org/10.1016/j.clineuro.2018.06.019
Manoharan SR, Baker DK, Pasara SM, Ponce B, Deinlein D, Theiss SM (2016) Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Spine J 16:862–866. https://doi.org/10.1016/j.spinee.2016.03.014
Marcus LP, McCutcheon BA, Noorbakhsh A, Parina RP, Gonda DD, Chen C, Chang DC, Carter BS (2014) Incidence and predictors of 30-day readmission for patients discharged home after craniotomy for malignant supratentorial tumors in California (1995-2010). J Neurosurg 120:1201–1211. https://doi.org/10.3171/2014.1.JNS131264
McDonald SJ, Sharkey JM, Sun M, Kaukas LM, Shultz SR, Turner RJ, Leonard AV, Brady RD, Corrigan F (2020) Beyond the brain: peripheral interactions after traumatic brain injury. J Neurotrauma 37:770–781. https://doi.org/10.1089/neu.2019.6885
McGirt MJ, Parker SL, Chotai S, Pfortmiller D, Sorenson JM, Foley K, Asher AL (2017) Predictors of extended length of stay, discharge to inpatient rehab, and hospital readmission following elective lumbar spine surgery: introduction of the Carolina-Semmes Grading Scale. J Neurosurg Spine 27:382–390. https://doi.org/10.3171/2016.12.SPINE16928
Narain AS, Hijji FY, Haws BE, Khechen B, Kudaravalli KT, Yom KH, Singh K (2020) American Society of Anesthesiologists score is not predictive of complication incidence after minimally invasive posterior lumbar spine procedures. Int J Spine Surg 14:32–37. https://doi.org/10.14444/7004
Neifert SN, Gal JS, Chapman EK, Caridi JM (2020) Nonhome discharge as an independent risk factor for adverse events and readmission in patients undergoing anterior cervical discectomy and fusion. Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000961
Reponen E, Korja M, Niemi T, Silvasti-Lundell M, Hernesniemi J, Tuominen H (2015) Preoperative identification of neurosurgery patients with a high risk of in-hospital complications: a prospective cohort of 418 consecutive elective craniotomy patients. J Neurosurg 123:594–604. https://doi.org/10.3171/2014.11.JNS141970
Reponen E, Tuominen H, Korja M (2014) Evidence for the use of preoperative risk assessment scores in elective cranial neurosurgery: a systematic review of the literature. Anesth Analg 119:420–432. https://doi.org/10.1213/ANE.0000000000000234
Rolston JD, Han SJ, Lau CY, Berger MS, Parsa AT (2014) Frequency and predictors of complications in neurological surgery: national trends from 2006 to 2011. J Neurosurg 120:736–745. https://doi.org/10.3171/2013.10.JNS122419
Saklad M, M.D. (1941) Grading of patients for surgical procedures. Anesthesiology: The Journal of the American Society of Anesthesiologists 2:281–284
Selassie AW, Fakhry SM, Ford DW (2011) Population-based study of the risk of in-hospital death after traumatic brain injury: the role of sepsis. J Trauma 71:1226–1234. https://doi.org/10.1097/TA.0b013e318226ecfc
Serafim R, Gomes JA, Salluh J, Povoa P (2018) A comparison of the quick-SOFA and systemic inflammatory response syndrome criteria for the diagnosis of sepsis and prediction of mortality: a systematic review and meta-analysis. Chest 153:646–655. https://doi.org/10.1016/j.chest.2017.12.015
Shaftel KA, Cole TS, Little AS (2020) National trends in hospital readmission following transsphenoidal surgery for pituitary lesions. Pituitary 23:79–91. https://doi.org/10.1007/s11102-019-01007-0
Sherrod BA, Johnston JM, Rocque BG (2016) Risk factors for unplanned readmission within 30 days after pediatric neurosurgery: a nationwide analysis of 9799 procedures from the American College of Surgeons National Surgical Quality Improvement Program. J Neurosurg Pediatr 18:350–362. https://doi.org/10.3171/2016.2.PEDS15604
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315:801–810. https://doi.org/10.1001/jama.2016.0287
Snyder DJ, Neifert SN, Gal JS, Deutsch BC, Caridi JM (2019) Posterior cervical decompression and fusion: assessing risk factors for nonhome discharge and the impact of disposition on postdischarge outcomes. World Neurosurg 125:e958–e965. https://doi.org/10.1016/j.wneu.2019.01.214
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2:81–84. https://doi.org/10.1016/s0140-6736(74)91639-0
Torio CM, Andrews RM (2013) National inpatient hospital costs: the most expensive conditions by Payer, 2011: Statistical brief #160. In: Healthcare Cost and Utilization Project (HCUP) statistical briefs. Rockville (MD). https://www.ncbi.nlm.nih.gov/books/NBK169005. Accessed 5 Jan 2020
Udekwu P, Kromhout-Schiro S, Vaslef S, Baker C, Oller D (2004) Glasgow Coma Scale score, mortality, and functional outcome in head-injured patients. J Trauma 56:1084–1089. https://doi.org/10.1097/01.ta.0000124283.02605.a5
Vincent JL, Quintairos ESA, Couto L Jr, Taccone FS (2016) The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care 20:257. https://doi.org/10.1186/s13054-016-1403-5
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K, Investigators EIGo (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302:2323–2329. https://doi.org/10.1001/jama.2009.1754
Whitmore RG, Stephen JH, Vernick C, Campbell PG, Yadla S, Ghobrial GM, Maltenfort MG, Ratliff JK (2014) ASA grade and Charlson Comorbidity Index of spinal surgery patients: correlation with complications and societal costs. Spine J 14:31–38. https://doi.org/10.1016/j.spinee.2013.03.011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We confirm that authorship requirements have been met and the final manuscript was
approved by all authors. We confirm also that this manuscript has not been published elsewhere and is not under consideration by another journal.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Georgetown University Medical Center) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Our Institutional Review Board approved this single-center retrospective study (IRB # 2018-0021).
Informed consent
Given retrospective nature of this study, formal consent is not required.
Additional information
Comments
Only very few studies have been conducted on the prevalence of sepsis following neurosurgery, let alone the risk factors for poor outcomes with this complication. In this retrospective single-center study of 105 patients recorded with sepsis after neurosurgery, the prevalence was recorded at 1.5% of all cases of neurosurgery. The single independent risk factor for readmission to hospital was a positive culture at the surgical site, whereas a medical history of cancer and a high maximum percentage of neutrophils emerged as independent predictors of death.
Kirsten Moeller
Copenhagen, Denmark
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous Presentation: Congress of Neurological Surgeons 2019 Annual Meeting, San Francisco, CA
This article is part of the Topical Collection on Neurosurgical Intensive Care
Rights and permissions
About this article
Cite this article
Rotter, J., Dowlati, E., Cobourn, K. et al. A cross-sectional analysis of variables associated with morbidity and mortality in postoperative neurosurgical patients diagnosed with sepsis. Acta Neurochir 162, 2837–2848 (2020). https://doi.org/10.1007/s00701-020-04586-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04586-1