Abstract
Purpose
To assess the benefit of placing a self-expandable metallic stent (SEMS) as a bridge to surgery for obstructive colorectal cancer (OCRC) according to the tumor site.
Methods
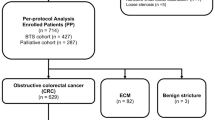
The subjects of this retrospective multicenter cohort study were 201 patients with OCRC, but without initial bowel perforation, who were treated either with a self-expandable metallic stent (SEMS) as a bridge to surgery (n = 109) or with primary surgery (PS; n = 92) between 2014 and 2016. The cohort consisted of 68 patients with right-sided and 133 left-sided OCRC. We evaluated the short-term surgical outcomes for each side.
Results
The SEMS group of patients with left-sided OCRC had significantly higher rates of primary resection, primary resection with anastomosis, stoma-free surgery, and laparoscopic surgery than the PS group of patients with left-sided OCRC. In contrast, the SEMS group of patients with right-sided OCRC had only a significantly higher rate of laparoscopic surgery than the PS group of patients with right-sided OCRC, but they had a longer overall hospital stay. There were no significant differences between the two treatment groups in the rates of morbidity or mortality, for either right-sided or left-sided OCRC.
Conclusion
The benefit of a SEMS as a bridge to surgery may be less for right-sided than for left-sided obstructions in colon cancer patients.
Similar content being viewed by others
References
Phillips RK, Hittinger R, Fry JS, Fielding LP. Malignant large bowel obstruction. Br J Surg. 1985;72:296–302.
Mella J, Biffin A, Radcliffe AG, Stamatakis JD, Steele RJ. Population-based audit of colorectal cancer management in two UK health regions. Colorectal Cancer Working Group, Royal College of Surgeons of England Clinical Epidemiology and Audit Unit. Br J Surg. 1997;84:1731–6.
Runkel NS, Hinz U, Lehnert T, Buhr HJ, Herfarth Ch. Improved outcome after emergency surgery for cancer of the large intestine. Br J Surg. 1998;85:1260–5.
Morita S, Ikeda K, Komori T, Tanida T, Hatano H, Tomimaru Y, et al. Outcomes in colorectal surgeon-driven management of obstructing colorectal cancers. Dis Colon Rectum. 2016;59:1028–33.
Tanis PJ, Paulino Pereira NR, van Hooft JE, Consten EC, Bemelman WA, Dutch Surgical Colorectal Audit. Resection of obstructive left-sided colon cancer at a national level: a prospective analysis of short-term outcomes in 1816 patients. Dig Surg. 2016;32:317–24.
Huang X, Lv B, Zhang S, Meng L. Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg. 2014;18:584–91.
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, et al. European Society of Gastrointestinal Endoscopy. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;46:990–1053.
Haraguchi N, Ikeda M, Miyake M, Yamada T, Sakakibara Y, Mita E, et al. Colonic stenting as a bridge to surgery for obstructive colorectal cancer: advantages and disadvantages. Surg Today. 2016;46:1310–7.
Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, et al. A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015;82:697–707.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Amelung FJ, Consten EC, Siersema PD, Tanis PJ. A population-based analysis of three treatment modalities for malignant obstruction of the proximal colon: acute resection versus stent or stoma as a bridge to surgery. Ann Surg Oncol. 2016;23:3660–8.
Kye BH, Lee YS, Cho HM, Kim JG, Oh ST, Lee IK, et al. Comparison of long-term outcomes between emergency surgery and bridge to surgery for malignant obstruction in right-sided colon cancer: a multicenter retrospective study. Ann Surg Oncol. 2016;23:1867–74.
Yao LQ, Xhong YS, Xu MD, Xu JM, Zhou PH, Cai XL. Self-expanding metallic stents drainage for acute proximal colon obstruction. World J Gastroenterol. 2011;28:3342–6.
Cho YK, Kim SW, Lee BI, Lee KM, Lim CH, Kim JS, et al. Clinical outcomes of self-expandable metal stent placement in the management of malignant proximal colon obstruction. Gut Liver. 2011;5:165–70.
Repici A, Adler DG, Gibbs CM, Malesci A, Preatoni P, Baron TH. Stenting of the proximal colon in patients with malignant large bowel obstruction: techniques and outcomes. Gastrointest Endosc. 2007;66:940–4.
Dronamraju SS, Ramamurthy S, Kelly SB, Hayat M. Role of self-expanding metallic stents in the management of malignant obstruction of the proximal colon. Dis Colon Rectum. 2009;52:1657–61.
Amelung FJ, de Beaufort HW, Siersema PD, Verhijen PM, Consten EC. Emergency resection versus bridge to surgery with stenting in patients with acute right-sided colonic obstruction: a systematic review focusing on mortality and morbidity rates. Int J Colorectal Dis. 2015;30:1147–55.
Kobayashi H, Miyata H, Gotoh M, Baba H, Kimura W, Kitagawa Y, et al. Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol. 2014;49:1047–55.
Acknowledgements
We thank the collaborators in the institutions belonging to the CSGO: M. Miyake (National Hospital Organization, Osaka National Hospital), N. Miyoshi (Osaka International Cancer Institute), H. Tamagawa (Otemae Hospital), H. Ohta (Ikeda Municipal Hospital), Y. Nushijima (Suita Municipal Hospital), K. Danno (Osaka General Medical Center), H. Takemoto (Kinki Central Hospital of the Mutual Aid Association of Public School Teachers), Y. Fumimoto (Tondabayashi Hospital), and I. Ohashi (Hannan Chuo Hospital).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Shunji Morita and his co-authors have no conflicts of interest to declare.
Additional information
The members of “Clinical Study Group of Osaka University (CSGO), Colorectal Group” are listed in acknowledgement section.
Rights and permissions
About this article
Cite this article
Morita, S., Yamamoto, K., Ogawa, A. et al. Benefits of using a self-expandable metallic stent as a bridge to surgery for right- and left-sided obstructive colorectal cancers. Surg Today 49, 32–37 (2019). https://doi.org/10.1007/s00595-018-1701-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1701-4