Abstract
Background
Malignant spinal cord compression (MSCC) has been noted in 3–5% of children with primary tumours. MSCC can be associated with permanent neurological deficits and prompt treatment is necessary. Our aim was to perform a systematic review on MSCC in children < 18 years to help formulate national guidelines.
Methods
A systematic review of the English language was undertaken using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Search criteria included ‘MSCC in children, paediatric and metastases’ for papers published between January1999 and December 2022. Isolated case reports/case series with < 10 patients were excluded.
Results
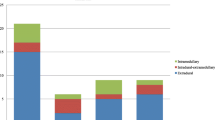
From a total of 17 articles identified, a final 7 were analysed (Level III/IV). Neuroblastoma constituted the most common cause for MSCC in children (62.7%) followed by sarcoma (14.2%). Soft tissue sarcomas were the most frequent cause of MSCC in children > 5 years old, while for neuroblastomas, the mean age of presentation was 20 months. The median age at time of diagnosis for the entire cohort of patients was 50.9 months (14.8–139). The median follow-up duration was 50.7 months (0.5–204).
Motor deficits were the presenting symptom in 95.6% of children followed by pain in 65.4% and sphincter disturbance in 24%. There was a delay of about 26.05 days (7–600) between the onset of symptoms and diagnosis.
A multimodality approach to treatment was utilised depending on the primary tumour. The prognosis for neurological recovery was found to be inversely proportional to the degree of neurological deficits and duration of symptoms in four studies.
Conclusion
Neuroblastoma is the most common cause for MSCC in children (62.7%) followed by sarcoma (14.2%), whilst soft tissue sarcomas constituted the most frequent cause of MSCC in children > 5 years old. The majority of patients presented with motor deficit, followed by pain. In children with neuroblastoma /lymphoma, chemotherapy was the primary treatment. Early surgery should be a consideration with rapid deterioration of neurology despite chemotherapy. A multimodality approach including chemo-radiotherapy and surgery should be the treatment of choice in metastatic sarcomas. It is worth noting that multi-level laminectomy/decompression and asymmetrical radiation to the spine can lead to spinal column deformity in the future.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Code availability
Not applicable.
References
Lewis DW et al (1986) Incidence, presentation, and outcome of spinal cord disease in children with systemic cancer. Pediatrics 78(3):438–443
Klein SL, Sanford RA, Muhlbauer MS (1991) Pediatric spinal epidural metastases. J Neurosurg 74(1):70–75
Lucia DM, Piero S, Simona V et al (2019) Symptomatic malignant spinal cord compression in children: a single-center experience. Ital J Pediatr 45:80
Tasdemiroglu E, Patchell RA (2001) Spinal cord compression caused by solid malignant tumours in children. Turk Neurosurg 11:101–107
Martino LD, Spennato P, Vetrella S et al (2019) Symptomatic malignant spinal cord compression in children: a single–center experience. Ital J Pediatr 45:80
Fawzy M, El-Beltagy M, El-Shafei M et al (2015) Intraspinal neuroblastoma: treatment options and neurological outcome of spinal cord compression. Oncol Lett 9:907–911
Katzenstein HM, Kent PM, London WB, Cohn SL (2001) Treatment and Outcome of 83 children with intraspinal neuroblastoma: the pediatric oncology group experience. J Clin Oncol 19(4):1047–1055. https://doi.org/10.1200/JCO.2001.19.4.1047
Tantawy A, Fatma SE, Mahmoud MA, Shepl OE (2013) Spinal cord compression in childhood pediatric malignancies: multicentric Egyptian study. J Pediatr Hematol Oncol 35:232–236
De Bernardi B, Pianca C, Pistamiglio P et al (2001) Neuroblastoma with symptomatic spinal cord compression at diagnosis: treatment and results with 76 cases. J Clin Oncol 19(1):183–190. https://doi.org/10.1200/JCO.2001.19.1.183
Pollono D, Tomarchia S, Drut R et al (2013) Spinal cord compression: a review of 70 pediatric patients. Pediatr Hematol Oncol 20(6):457–466
Abrahm JL (2004) Assessment and treatment of patients with malignant spinal cord compression. J Support Oncol 2:377–401
De Bernardi B, Balwierz W, Bejent J et al (2005) Epidural compression in neuroblastoma: diagnostic and therapeutic aspects. Cancer Lett 228:283–299
Siegal T (1995) Spinal cord compression: from laboratory to clinic. Eur J Cancer 31A:1748–1753
Raffel C, Neave VC, Lavine S, McComb JG (1991) Treatment of spinal cord compression by epidural malignancy in childhood. Neurosurgery 28:349–352
Mayfield JK, Riseborough EJ, Jaffe N et al (1981) Spinal deformity in children treated for neuroblastoma. J Bone Joint Surg 63:183–193
Vijay MR, Ilyas M, Meic H, Douglas L (2016) Primary osseous tumors of the pediatric spinal column: review of pathology and surgical decision making. Neurosurg Focus 41(2):E3
Punt J, Pritchard J, Pincott JR et al (1980) Neuroblastoma: a review of 21 cases presenting with intraspinal cord compression. Cancer 45:3095–3101
Hesketh E, Eden OB, Gattamaneni HR et al (1998) Spinal cord compression: do we miss it? Acta Paediatr 87:452–454
Sun H, Nemecek AN (2010) Optimal management of malignant epidural spinal cord compression. Hematol Oncol Clin North Am 24:537–551
Loblaw DA, Laperriere NJ (1998) Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol 16:1613–1624
Hell AK, Kühnle I, Lorenz HM, Braunschweig L, Lüders KA, Bock HC, Kramm CM, Ludwig HC, Tsaknakis K (2020) Spinal deformities after childhood tumors. Cancers 12(12):3555
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MAH, NP and NQ contributed to the study conception and design. Data collection and analysis were performed by MAH and NP. The first draft of the manuscript was written by MAH and NP, and all authors commented on previous versions of the manuscript. Final version of the article reviewed by NQ and MAH.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Consent for publication
Not applicable
Consent to participate
Not applicable
Ethical approval
Not applicable
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quraishi, N.A., Palliyil, N., Hassanin, M.A. et al. Malignant spinal cord compression in the paediatric population—a systematic review, meta-analysis. Eur Spine J 32, 4306–4313 (2023). https://doi.org/10.1007/s00586-023-07820-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07820-3