Abstract
Purpose
This in vitro biomechanical study compares residual lumbar range of motion (ROM) and rod strain after lumbopelvic instrumentation using 2 rods, 4 rods and interbody cages.
Methods
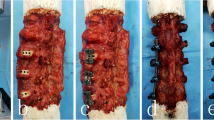
Seven human cadaveric specimens were instrumented from L1 to sacrum, and pelvic screws were implanted. The pelvis was constrained and moments up to 7.5 Nm were applied to T12. Segmental L1–S1 ROM was analyzed by tracking radiopaque balls implanted in each vertebra using biplanar radiographs. Deformation within principal rods was measured by strain gauges. Four configurations were compared: 2 rods (2R), 4 rods (4R), 4 rods + ALIF at L4–L5 and L5–S1 (4R + ALIF), 2 rods + ALIF (2R + ALIF).
Results
Intact average global L1–S1 ROM was 42.9° (27.9°–66.0°) in flexion–extension (FE), 35.2° (26.8°–51.8°) in lateral bending (LB), 18.6° (6.7°–47.8°) in axial rotation (AR). In FE, average ROM was 1.9° with both 4-rod configurations versus 2.5° with 2R and 2.8° with 2R + ALIF (p < 0.05). In LB, ROM ranged between 1.2° and 1.5° without significant differences. In AR, ROM was 2.5° with both 4-rod configurations versus 2.9° with 2R (p = 0.07) and 3.1° with 2R ALIF (p = 0.01). In FE, strain decreased by 64% and 65% in principal rods at L3–L4 with 4-rod. When comparing 2-rod configurations, strain decreased by 1% in flexion and increased by 22% in extension at L3–L4 when adding an ALIF at L4–L5 and L5–S1.
Conclusions
Double rods and interbody cages decrease residual ROM in FE and AT. Double rods seem efficient in limiting strain in principal rods. The use of single rods with cages at the lumbosacral junction increases strain at the first adjacent level without cage.





Similar content being viewed by others
References
Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP, Hostin R, Fu KM, Burton D, Akbarnia B, Gupta M, Hart R, Bess S, Lafage V, International Spine Study Group (2013) Change in classification grade by the SRS-Schwab Adult Spinal Deformity Classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976) 38(19):1663–1671
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V, International Spine Study Group (ISSG) (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38(13):E803–E812
Kelly MP, Lenke LG, Bridwell KH, Agarwal R, Godzik J, Koester L (2013) Fate of the adult revision spinal deformity patient: a single institution experience. Spine (Phila Pa 1976) 38(19):E1196–E1200
Zhu F, Bao H, Liu Z, Bentley M, Zhu Z, Ding Y, Qiu Y (2014) Unanticipated revision surgery in adult spinal deformity: an experience with 815 cases at one institution. Spine (Phila Pa 1976) 39(26 Spec No.):B36–B44
Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D (2012) Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976) 37(8):693–700
Blamoutier A, Guigui P, Charosky S, Roussouly P, Chopin D (2012) Surgery of lumbar and thoracolumbar scolioses in adults over 50. Morbidity and survival in a multicenter retrospective cohort of 180 patients with a mean follow-up of 4.5 years. Orthop Traumatol Surg Res 98(5):528–535
Riouallon G, Bouyer B, Wolff S (2016) Risk of revision surgery for adult idiopathic scoliosis: a survival analysis of 517 cases over 25 years. Eur Spine J 25(8):2527–2534
Volkheimer D, Reichel H, Wilke H-J, Lattig F (2017) Is pelvic fixation the only option to provide additional stability to the sacral anchorage in long lumbar instrumentation? A comparative biomechanical study of new techniques. Clin Biomech Bristol Avon 43:34–39
Schwab FJ, Hawkinson N, Lafage V, Smith JS, Hart R, Mundis G, Burton DC, Line B, Akbarnia B, Boachie-Adjei O, Hostin R, Shaffrey CI, Arlet V, Wood K, Gupta M, Bess S, Mummaneni PV, International Spine Study Group (2012) Risk factors for major peri-operative complications in adult spinal deformity surgery: a multi-center review of 953 consecutive patients. Eur Spine J 21(12):2603–2610
Yamato Y, Matsuyama Y, Hasegawa K, Aota Y, Akazawa T, Iida T, Ueyama K, Uno K, Kanemura T, Kawakami N, Kotani T, Takaso M, Takahashi J, Tanaka M, Taneichi H, Tsuji T, Hosoe H, Mochida J, Shimizu T, Yonezawa I, Watanabe K, Matsumoto M, Committee for Adult Deformity, Japanese Scoliosis Society (2017) A Japanese nationwide multicenter survey on perioperative complications of corrective fusion for elderly patients with adult spinal deformity. J Orthop Sci 22(2):237–242
Vaz K, Verma K, Protopsaltis T, Schwab F, Lonner B, Errico T (2010) Bone grafting options for lumbar spine surgery: a review examining clinical efficacy and complications. SAS J 4(3):75–86
Mummaneni PV, Dhall SS, Eck JC, Groff MW, Ghogawala Z, Watters WC, Dailey AT, Resnick DK, Choudhri TF, Sharan A, Wang JC, Kaiser MG (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 11: interbody techniques for lumbar fusion. J Neurosurg Spine 21(1):67–74
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1(1):2–18
Hyun S-J, Lenke LG, Kim Y-C, Koester LA, Blanke KM (2014) Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 39(22):1899–1904
Merrill RK, Kim JS, Leven DM, Kim JH, Cho SK (2017) Multi-rod constructs can prevent rod breakage and pseudarthrosis at the lumbosacral junction in adult spinal deformity. Glob Spine J 7(6):514–520
Daniels AH, DePasse JM, Durand W, Hamilton DK, Passias P, Kim HJ, Protopsaltis T, Reid DBC, LaFage V, Smith JS, Shaffrey C, Gupta M, Klineberg E, Schwab F, Burton D, Bess S, Ames C, Hart RA, International Spine Study Group (2018) Rod fracture after apparently solid radiographic fusion in adult spinal deformity patients. World Neurosurg 117:e530–e537
Guevara-Villazón F, Boissiere L, Hayashi K, Larrieu D, Ghailane S, Vital J-M, Gille O, Pointillart V, Obeid I, Bourghli A (2020) Multiple-rod constructs in adult spinal deformity surgery for pelvic-fixated long instrumentations: an integral matched cohort analysis. Eur Spine J 29(4):886–895
Gupta S, Eksi MS, Ames CP, Deviren V, Durbin-Johnson B, Smith JS, Gupta MC (2018) A novel 4-rod technique offers potential to reduce rod breakage and pseudarthrosis in pedicle subtraction osteotomies for adult spinal deformity correction. Oper Neurosurg (Hagerstown) 14(4):449–456
Humbert L, De Guise JA, Aubert B, Godbout B, Skalli W (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31(6):681–687
Mitton D, Deschênes S, Laporte S, Godbout B, Bertrand S, de Guise JA, Skalli W (2006) 3D reconstruction of the pelvis from bi-planar radiography. Comput Methods Biomech Biomed Eng 9(1):1–5
Ghostine B, Sauret C, Assi A, Bakouny Z, Khalil N, Skalli W, Ghanem I (2017) Influence of patient axial malpositioning on the trueness and precision of pelvic parameters obtained from 3D reconstructions based on biplanar radiographs. Eur Radiol 27(3):1295–1302
Muth-seng C, Brauge D, Soriau N, Sandoz B, Van den Abbeele M, Skalli W, Laporte S (2019) Experimental analysis of the lower cervical spine in flexion with a focus on facet tracking. J Biomech 93:220–225
Wilke HJ, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 7(2):148–154
Lertudomphonwanit T, Kelly MP, Bridwell KH, Lenke LG, McAnany SJ, Punyarat P, Bryan TP, Buchowski JM, Zebala LP, Sides BA, Steger-May K, Gupta MC (2018) Rod fracture in adult spinal deformity surgery fused to the sacrum: prevalence, risk factors, and impact on health-related quality of life in 526 patients. Spine J 18(9):1612–1624
La Barbera L, Galbusera F, Wilke H-J, Villa T (2016) Preclinical evaluation of posterior spine stabilization devices: can the current standards represent basic everyday life activities? Eur Spine J 25(9):2909–2918
La Barbera L, Galbusera F, Wilke H-J, Villa T (2017) Preclinical evaluation of posterior spine stabilization devices: can we compare in vitro and in vivo loads on the instrumentation? Eur Spine J 26(1):200–209
Banno T, Hasegawa T, Yamato Y, Togawa D, Yoshida G, Kobayashi S, Yasuda T, Arima H, Oe S, Mihara Y, Ushirozako H, Matsuyama Y (2019) Multi-rod constructs can increase the incidence of iliac screw loosening after surgery for adult spinal deformity. Asian Spine J 13(3):500–510
Pearcy M, Portek I, Shepherd J (1984) Three-dimensional X-ray analysis of normal movement in the lumbar spine. Spine (Phila Pa 1976) 9(3):294–297
Pearcy MJ, Tibrewal SB (1984) Axial rotation and lateral bending in the normal lumbar spine measured by three-dimensional radiography. Spine (Phila Pa 1976) 9(6):582–587
Dvorák J, Panjabi MM, Chang DG, Theiler R, Grob D (1991) Functional radiographic diagnosis of the lumbar spine. Flexion-extension and lateral bending. Spine (Phila Pa 1976) 16(5):562–571
Hayes MA, Howard TC, Gruel CR, Kopta JA (1989) Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine (Phila Pa 1976) 14(3):327–331
Panjabi MM, Oxland TR, Yamamoto I, Crisco JJ (1994) Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg Am 76(3):413–424
Guan Y, Yoganandan N, Moore J, Pintar FA, Zhang J, Maiman DJ, Laud P (2007) Moment–rotation responses of the human lumbosacral spinal column. J Biomech 40(9):1975–1980
Heuer F, Schmidt H, Klezl Z, Claes L, Wilke H-J (2007) Stepwise reduction of functional spinal structures increase range of motion and change lordosis angle. J Biomech 40(2):271–280
Charles YP, Persohn S, Steib J-P, Mazel C, Skalli W (2011) Influence of an auxiliary facet system on lumbar spine biomechanics. Spine (Phila Pa 1976) 36(9):690–699
Hlubek RJ, Godzik J, Newcomb AGUS, Lehrman JN, de Andrada B, Bohl MA, Farber SH, Kelly BP, Turner JD (2019) Iliac screws may not be necessary in long-segment constructs with L5–S1 anterior lumbar interbody fusion: cadaveric study of stability and instrumentation strain. Spine J 9(5):942–950
Scheer JK, Tang JA, Deviren V, Buckley JM, Pekmezci M, McClellan RT, Ames CP (2011) Biomechanical analysis of revision strategies for rod fracture in pedicle subtraction osteotomy. Neurosurgery 69(1):164–172
Hallager DW, Gehrchen M, Dahl B, Harris JA, Gudipally M, Jenkins S, Wu AM, Bucklen BS (2016) Use of supplemental short pre-contoured accessory rods and cobalt chrome alloy posterior rods reduces primary rod strain and range of motion across the pedicle subtraction osteotomy level: an in vitro biomechanical study. Spine (Phila Pa 1976) 41(7):E388–E395
Dahl BT, Harris JA, Gudipally M, Moldavsky M, Khalil S, Bucklen BS (2017) Kinematic efficacy of supplemental anterior lumbar interbody fusion at lumbosacral levels in thoracolumbosacral deformity correction with and without pedicle subtraction osteotomy at L3: an in vitro cadaveric study. Eur Spine J 26(11):2773–2781
La Barbera L, Brayda-Bruno M, Liebsch C, Villa T, Luca A, Galbusera F, Wilke HJ (2018) Biomechanical advantages of supplemental accessory and satellite rods with and without interbody cages implantation for the stabilization of pedicle subtraction osteotomy. Eur Spine J 27(9):2357–2366
La Barbera L, Wilke H-J, Liebsch C, Villa T, Luca A, Galbusera F, Brayda-Bruno M (2020) Biomechanical in vitro comparison between anterior column realignment and pedicle subtraction osteotomy for severe sagittal imbalance correction. Eur Spine J 29(1):36–44
Seyed Vosoughi A, Joukar A, Kiapour A, Parajuli D, Agarwal AK, Goel VK, Zavatsky J (2019) Optimal satellite rod constructs to mitigate rod failure following pedicle subtraction osteotomy (PSO): a finite element study. Spine J 19(5):931–941
Luca A, Ottardi C, Lovi A, Brayda-Bruno M, Villa T, Galbusera F (2017) Anterior support reduces the stresses on the posterior instrumentation after pedicle subtraction osteotomy: a finite-element study. Eur Spine J 26(Suppl 4):450–456
Luca A, Ottardi C, Sasso M, Prosdocimo L, La Barbera L, Brayda-Bruno M, Galbusera F, Villa T (2017) Instrumentation failure following pedicle subtraction osteotomy: the role of rod material, diameter, and multi-rod constructs. Eur Spine J 26(3):764–770
Godzik J, Hlubek RJ, Newcomb AGUS, Lehrman JN, de Andrada Pereira B, Farber SH, Lenke LG, Kelly BP, Turner JD (2019) Supplemental rods are needed to maximally reduce rod strain across the lumbosacral junction with TLIF but not ALIF in long constructs. Spine J 19(6):1121–1131
Kleck CJ, Illing D, Lindley EM, Noshchenko A, Patel VV, Barton C, Baldini T, Cain CMJ, Burger EL (2017) Strain in posterior instrumentation resulted by different combinations of posterior and anterior devices for long spine fusion constructs. Spine Deform 5(1):27–36
Kleck CJ, Illing D, Lindley EM, Noshchenko A, Patel VV, Barton C, Baldini T, Cain CMJ, Burger EL (2018) Reply to Letter to Editor: strain in posterior instrumentation resulted by different combinations of posterior and anterior devices for long spine fusion constructs. Spine Deform 6(3):335–340
Acknowledgements
The authors would like to acknowlege Clariance Spine for technical and financial support and Société Française de Chirurgie du Rachis (SFCR) for research grant.
Funding
A research grant was obtained from the Société Française de Chirurgie Rachidienne (SFCR). Technical and financial support was provided by Clariance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ntilikina, Y., Charles, Y.P., Persohn, S. et al. Influence of double rods and interbody cages on quasistatic range of motion of the spine after lumbopelvic instrumentation. Eur Spine J 29, 2980–2989 (2020). https://doi.org/10.1007/s00586-020-06594-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06594-2