Abstract
Purpose
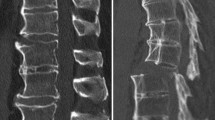
The goal of this study was to evaluate the results and feasibility of primary anterior cervical discectomy and fusion (ACDF) with plating for unstable traumatic spondylolisthesis of the axis, the so-called hangman’s fracture, via the standard anterior retropharyngeal approach.
Methods
The clinical and radiological records of 17 patients (14 males and 3 females, mean age: 51 years, range 17–73 years) with unstable hangman’s fracture who were treated between January 1996 and June 2012 were reviewed retrospectively. ACDF with plating at C2–3 level was performed in all patients (type II fracture: 12 patients, type IIA fracture: 3 patients and type III fracture: 2 patients, based on the Levine and Edwards classification). Combined morbidity, complications, neurological improvement and fusion rate were assessed.
Results
Seventeen patients underwent fusion surgery via the standard anterior retropharyngeal approach. Four patients required an additional posterior arthrodesis to augment the anterior procedure. Patients wore a Philadelphia collar for 4–6 weeks and fusion at C2–3 was achieved in all patients. Two cases of complications were observed during treatment, comprising of one case of non-union and one case of transient dysphagia that resolved after 3 months. However, none of the patients experienced worsening of the neurological function post-operatively. There were no cases of permanent nerve injury or infection.
Conclusions
Treatment of the hangman’s fracture is dependent on the stability of the injury. Although the treatment for unstable hangman’s fracture is still controversial, we carefully suggest that primary ACDF with plating via the standard anterior retropharyngeal approach may be a feasible treatment option. It provides immediate stability and allows for early ambulation while promoting a stable bone union with minimal morbidity.


Similar content being viewed by others
References
Hadley MN, Dickman CA, Browner CM, Sonntag VK (1989) Acute axis fractures: a review of 229 cases. J Neurosurg 71:642–647
Bucholz RD, Cheung KC (1989) Halo vest versus spinal fusion for cervical injury: evidence from an outcome study. J Neurosurg 70:884–892
Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R (1981) Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br 63(B):313–318
Levine AM, Edwards CC (1985) The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 67:217–226
Tian W, Weng C, Liu B, Li Q, Hu L, Li ZY, Liu YJ, Sun YZ (2012) Posterior fixation and fusion of unstable Hangman’s fracture by using intraoperative three-dimensional fluoroscopy-based navigation. Eur Spine J 21:863–871
Xu H, Zhao J, Yuan J, Wang C (2010) Anterior discectomy and fusion with internal fixation for unstable hangman’s fracture. Int Orthop 34:85–88
Boullosa JL, Colli BO, Carlotti CG Jr, Tanaka K, dos Santos MB (2004) Surgical management of axis’ traumatic spondylolisthesis (Hangman’s fracture). Arq Neuropsiquiatr 62:821–826
Tuite GF, Papadopoulos SM, Sonntag VK (1992) Caspar plate fixation for the treatment of complex hangman’s fractures. Neurosurgery 30:761–764
Koller H, Kathrein A (2006) Letter to the Editor concerning: A systematic review of the management of hangman’s fractures by **n-Feng Li et al (2006) Eur Spine J 15: 257–269, author reply 1419–1421
Verheggen R, Jansen J (1998) Hangman’s fracture: arguments in favor of surgical therapy for type II and III according to Edwards and Levine. Surg Neurol 49:253–261 discussion 261-252
Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK (1997) Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 22:1843–1852
Moon MS, Moon JL, Moon YW, Sun DH, Choi WT (2001) Traumatic spondylolisthesis of the axis: 42 cases. Bull Hosp Jt Dis 60:61–66
Coric D, Wilson JA, Kelly DL Jr (1996) Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg 85:550–554
Vaccaro AR, Madigan L, Bauerle WB, Blescia A, Cotler JM (2002) Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976) 27:2229–2233
Watanabe M, Nomura T, Toh E, Sato M, Mochida J (2005) Residual neck pain after traumatic spondylolisthesis of the axis. J Spinal Disord Tech 18:148–151
Li XF, Dai LY, Lu H, Chen XD (2006) A systematic review of the management of hangman’s fractures. Eur Spine J 15:257–269
Borne GM, Bedou GL, Pinaudeau M (1984) Treatment of pedicular fractures of the axis. A clinical study and screw fixation technique. J Neurosurg 60:88–93
Ma W, Xu R, Liu J, Sun S, Zhao L, Hu Y, Jiang W, Liu G, Gu Y (2011) Posterior short-segment fixation and fusion in unstable Hangman’s fractures. Spine (Phila Pa 1976) 36: 529–533
Abumi K, Kaneda K (1997) Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 22:1853–1863
Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Nakashima H, Machino M (2009) Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J 18:1293–1299
Duggal N, Chamberlain RH, Perez-Garza LE, Espinoza-Larios A, Sonntag VK, Crawford NR (2007) Hangman’s fracture: a biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976) 32:182–187
Wilson AJ, Marshall RW, Ewart M (1999) Transoral fusion with internal fixation in a displaced hangman’s fracture. Spine (Phila Pa 1976) 24:295–298
Park SH, Sung JK, Lee SH, Park J, Hwang JH, Hwang SK (2007) High anterior cervical approach to the upper cervical spine. Surg Neurol 68:519–524 discussion 524
Hald J, Andreassen UK (1994) Submandibular gland excision: short- and long-term complications. ORL J Otorhinolaryngol Relat Spec 56:87–91
Skaf GS, Sabbagh AS, Hadi U (2007) The advantages of submandibular gland resection in anterior retropharyngeal approach to the upper cervical spine. Eur Spine J 16:469–477
Park SA, Lee JH, Nam YS, An X, Han SH, Ha KY (2013) Topographical anatomy of the anterior cervical approach for c2–3 level. Eur Spine J 22:1497–1503
Acknowledgments
This research was financially supported by Chonnam National University, 2011.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hur, H., Lee, JK., Jang, JW. et al. Is it feasible to treat unstable hangman’s fracture via the primary standard anterior retropharyngeal approach?. Eur Spine J 23, 1641–1647 (2014). https://doi.org/10.1007/s00586-014-3311-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3311-1