Abstract
Purpose
Preoperative malnutrition is associated with postoperative complications, prolonged intensive care unit stay, and mortality, leading to functional disability after non-cardiac surgery. However, its effects on cardiac and thoracic aortic surgery outcomes remain unknown. We examined the effects of preoperative malnutrition on disability-free survival after surgery and assessed the perioperative 12-item World Health Organization Disability Assessment Schedule 2.0 (WHODAS2.0) score based on the preoperative nutritional status.
Methods
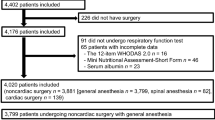
We included individuals aged ≥ 55 years who underwent elective cardiac and/or thoracic aortic surgery between April 1, 2016 and December 28, 2018 in a tertiary center. The nutritional status was assessed preoperatively using the Mini Nutritional Assessment Short Form, with scores < 12 points indicating a poor nutritional status. The JapanSCORE2 was calculated for surgical risk prediction. Our primary outcome was disability-free survival 1 year after surgery (WHODAS2.0 score: < 16%). The odds ratio of poor nutritional status for disability-free survival was calculated using multiple logistic regression analysis after adjusting for age, JapanSCORE2, and duration of surgery.
Results
One hundred patients were followed up for 1 year. Preoperatively, 41 of them had a poor nutritional status. The disability-free survival rates 1 year postoperatively were 46.3% (19/41) and 64.4% (38/59) in patients with and without poor preoperative nutritional status, respectively. The adjusted odds ratio of poor nutritional status for disability-free survival at 1 year after surgery was 0.42 (95% confidence interval, 0.17–0.99).
Conclusion
Patients with a poor preoperative nutritional status had less likely to show disability-free survival 1 year after cardiac and thoracic aortic surgery.


Similar content being viewed by others
Data availability
Data pertaining to this study are available as a spreadsheet file upon reasonable request.
References
Chan PG, Seese L, Aranda-Michel E, Sultan I, Gleason TG, Wang Y, Thoma F, Kilic A. Operative mortality in adult cardiac surgery: is the currently utilized definition justified? J Thorac Dis. 2021;13:5582–91.
Writing Committee for the VISION Study Investigators, Devereaux PJ, Biccard BM, Sigamani A, Xavier D, Chan MTV, Srinathan SK, Walsh M, Abraham V, Pearse R, Wang CY, Sessler DI, Kurz A, Szczeklik W, Berwanger O, Villar JC, Malaga G, Garg AX, Chow CK, Ackland G, Patel A, Borges FK, Belley-Cote EP, Duceppe E, Spence J, Tandon V, Williams C, Sapsford RJ, Polanczyk CA, Tiboni M, Alonso-Coello P, Faruqui A, Heels-Ansdell D, Lamy A, Whitlock R, LeManach Y, Roshanov PS, McGillion M, Kavsak P, McQueen MJ, Thabane L, Rodseth RN, Buse GL, Bhandari M, Garutti I, Jacka MJ, Schünemann HJ, Cortes OL, Coriat P, Dvirnik N, Botto F, Pettit S, Jaffe AS, Guyatt GH. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317:1642–51.
Myles P, Bellomo R, Corcoran T, Forbes A, Wallace S, Peyton P, Christophi C, Story D, Leslie K, Serpell J, McGuinness S, Parke R, Australian and New Zealand College of Anaesthetists Clinical Trials Network, and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Restrictive versus liberal fluid therapy in major abdominal surgery (RELIEF): rationale and design for a multicentre randomised trial. BMJ Open. 2017;7:e015358.93.
Joosten A, Delaporte A, Mortier J, Ickx B, Van Obbergh L, Vincent J, Cannesson M, Rinehart J, Van der Linden P. Long-term impact of crystalloid versus colloid solutions on renal function and disability-free survival after major abdominal surgery. Anesthesiology. 2019;130:227–36.
Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, Laviano A, Ljungqvist O, Lobo DN, Martindale R, Waitzberg DL, Bischoff SC, Singer P. ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 2017;36:623–50.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony P, Charlton KE, Maggio M, Tsai AC, Grathwohl D, Vellas B, Sieber CC, MNA-International Group. Validation of the Mini Nutritional Assessment short-form (MNASF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13:782–8.
Kanemoto M, Ida M, Naito Y, Kawaguchi M. The impact of preoperative nutrition status on abdominal surgery outcomes: a prospective cohort study. Nutr Clin Pract. 2022. https://doi.org/10.1002/ncp.10932.
Ida M, Naito Y, Tanaka Y, Inoue S, Kawaguchi M. Factors associated with functional disability or mortality after elective noncardiac surgery: a prospective cohort study. Can J Anaesth. 2022;69:704–14.
Lomivorotov VV, Efremov SM, Boboshko VA, Nikolaev DA, Vedernikov PE, Deryagin MN, Lomivorotov VN, Karaskov AM. Prognostic value of nutritional screening tools for patients scheduled for cardiac surgery. Interact Cardiovasc Thorac Surg. 2013;16:612–8.
Lim SL, Ong KCB, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. 2012;31:345–50.
Motomura N, Miyata H, Tsukihara H, Takamoto S, Japan Cardiovascular Surgery Database Organization. Risk model of valve surgery in Japan using the Japan Adult Cardiovascular Surgery Database. J Heart Valve Dis. 2010;19:684–91.
World Health Organization. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). Geneva. 2010. https://apps.who.int/iris/bitstream/handle/10665/43974/9789241547598_eng.pdf?sequence=1&isAllowed=y. Accessed December 2022
Shulman MA, Kasza J, Myles PS. Defining the minimal clinically important difference and patient-acceptable symptom state score for disability assessment in surgical patients. Anesthesiology. 2020;132:1362–70.
McIsaac DI, Taljaard M, Bryson GL, Beaulé PE, Gagné S, Hamilton G, Hladkowicz E, Huang A, Joanisse JA, Lavallée LT, MacDonald D, Moloo H, Thavorn K, van Walraven C, Yang H, Forster AJ. Frailty as a predictor of death or new disability after surgery: a prospective cohort study. Ann Surg. 2020;271:283–9.
McIsaac DI, Taljaard M, Bryson GL, Beaulé PE, Gagne S, Hamilton G, Hladkowicz E, Huang A, Joanisse J, Lavallée LT, MacDonald D, Moloo H, Thavorn K, van Walraven C, Yang H, Forster AJ. Frailty and long-term postoperative disability trajectories: a prospective multicentre cohort study. Br J Anaesth. 2020;125:704–11.
Shimakura K, Minami K, Yoshitani K, Ohnishi Y, Iida H. Cardiac surgery improves the postoperative frailty score of frail patients. J Anesth. 2022;36:186–93.
Milne B, de Carvalho JL, Ayis S, Chaubey S, Khan H, Kunst G. Frailty and perioperative patient-reported disability in patients undergoing cardiac surgery: a pilot study. Br J Anaesth. 2022;128:949–58.
McGrail K, Bryan S, Davis J. Let’s all go to the PROM: the case for routine patient-reported outcome measurement in Canadian healthcare. Healthc Pap. 2011;11:8–18.
Lopez-Delgado JC, Muñoz-Del Rio G, Flordelís-Lasierra JL, Putzu A. Nutrition in adult cardiac surgery: preoperative evaluation, management in the postoperative period, and clinical implications for outcomes. J Cardiothorac Vasc Anesth. 2019;33:3143–62.
Knight SR, Qureshi AU, Drake TM, Lapitan MCM, Maimbo M, Yenli E, Tabiri S, Ghosh D, Kingsley PA, Sundar S, Shaw C, Valparaiso AP, Bhangu A, Brocklehurst P, Magill L, Morton DG, Norrie J, Roberts TE, Theodoratou E, Weiser TG, Burden S, Harrison EM. The impact of preoperative oral nutrition supplementation on outcomes in patients undergoing gastrointestinal surgery for cancer in low- and middle-income countries: a systematic review and meta-analysis. Sci Rep. 2022;12:12456.
Gerdessen L, Meybohm P, Choorapoikayil S, Herrmann E, Taeuber I, Neef V, Raimann FJ, Zacharowski K, Piekarski F. Comparison of common perioperative blood loss estimation techniques: a systematic review and meta-analysis. J Clin Monit Comput. 2021;35:245–58.
Stoppe C, Whitlock R, Arora RC, Heyland DK. Nutrition support in cardiac surgery patients: be calm and feed on! J Thorac Cardiovasc Surg. 2019;158:1103–8.
Acknowledgements
Ozu Naoki (Department of Medical Statistics, Nara Medical University, Nara, Japan) advised and assisted with the statistical planning and analysis. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This study was funded by the Nara Medical University Grant-in-Aid for a large-scale prospective cohort study on healthy life expectancies. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
HK: data collection and draft writing. MI: Study coordinator, study conception and design, interpretation of data, and revision of the draft. YN: Study conception and design, interpretation of data, and manuscript revision. MK: Study conception and design, interpretation of data, and manuscript revision. All authors critically reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kawanishi, H., Ida, M., Naito, Y. et al. Effects of preoperative nutritional status on disability-free survival after cardiac and thoracic aortic surgery: a prospective observational study. J Anesth 37, 401–407 (2023). https://doi.org/10.1007/s00540-023-03178-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03178-4