Abstract
Purpose
To perform a systematic review on financial toxicity of breast cancer–related lymphedema.
Methods
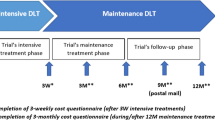
Seven databases were searched on September 11, 2022. Eligible studies were identified, analyzed, and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. Empirical studies were appraised by the Joanna Briggs Institute (JBI) tools. The Mixed Methods Appraisal Tool version 2018 was used to assess the mixed method studies.
Results
A total of 963 articles were identified, but only 7 articles reporting on 6 studies met the eligibility criteria. A 2-year treatment for lymphedema was approximately USD$14,877 to USD$23,167 in America. In Australia, the average out-of-pocket costs ranged from A$207 to A$1400 (USD$156.26 to USD$1056.83) per year. Outpatient visits, compressed clothing, and hospital admissions were the dominant costs. The financial toxicity was associated with the severity of lymphedema, and patients with heavy financial burden had to reduce other expenses or even forgo the treatment.
Conclusion
Breast cancer–related lymphedema aggravated the economic burden of patients. The included studies showed great variation in the methods used and therefore differences in cost results. The national government should further improve the healthcare system and increase the insurance coverage of lymphedema treatment to alleviate this burden. More research is needed to focus on financial toxicity experience of breast cancer patients with lymphedema.
Implications for cancer survivors
The cost of the ongoing treatment of breast cancer–related lymphedema influences patients’ economic situation and quality of life. Survivors need to be informed early about the potential financial burden associated with lymphedema treatment.

Similar content being viewed by others
Data availability
All data generated for this review are included in the manuscript and/or the supplementary files.
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34. https://doi.org/10.3322/caac.21551
Hong R, Xu B (2022) Breast cancer: an up-to-date review and future perspectives. Cancer Commun 42(10):913–936. https://doi.org/10.1002/cac2.12358
Ezzo J, Manheimer E, McNeely ML et al (2015) Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev 5:CD003475. Published 2015 May 21. https://doi.org/10.1002/14651858.CD003475.pub2
Sayegh HE, Asdourian MS, Swaroop MN et al (2017) Diagnostic methods, risk factors, prevention, and management of breast cancer-related lymphedema: past, present, and future directions. Curr Breast Cancer Rep 9(2):111–121. https://doi.org/10.1007/s12609-017-0237-8
DiSipio T, Rye S, Newman B et al (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515. https://doi.org/10.1016/S1470-2045(13)70076-7
Boeer B, Seller A, Schoenfisch B et al (2022) The impact of rehabilitation sport on breast cancer-related lymphoedema and quality of life [published online ahead of print, 2022 Jul 26]. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-022-06609-x
Mete Civelek G, Akinci MG, Dalyan M (2022) Evaluation of sleep quality, depression, and quality of life in patients with breast cancer related lymphedema [published online ahead of print, 2022 Sep 29]. Lymphat Res Biol. https://doi.org/10.1089/lrb.2022.0031
Coughlin SS, Ayyala DN, Tingen MS, Cortes JE (2020) Financial distress among breast cancer survivors. Curr Cancer Rep 2(1):48–53. https://doi.org/10.25082/CCR.2020.01.004
Dean LT, Moss SL, Rollinson SI, Frasso Jaramillo L, Paxton RJ, Owczarzak JT (2019) Patient recommendations for reducing long-lasting economic burden after breast cancer. Cancer 125(11):1929–1940. https://doi.org/10.1002/cncr.32012
Abrams HR, Durbin S, Huang CX et al (2021) Financial toxicity in cancer care: origins, impact, and solutions. Transl Behav Med 11(11):2043–2054. https://doi.org/10.1093/tbm/ibab091
Smile TD, Tendulkar R, Schwarz G et al (2018) A review of treatment for breast cancer-related lymphedema: paradigms for clinical practice. Am J Clin Oncol 41(2):178–190. https://doi.org/10.1097/COC.0000000000000355
Cheng MH, Ho OA, Tsai TJ, Lin YL, Kuo CF (2022) Breast cancer-related lymphedema correlated with incidence of cellulitis and mortality. J Surg Oncol 126(7):1162–1168. https://doi.org/10.1002/jso.27054
Roberson ML, Strassle PD, Fasehun LO, Erim DO, Deune EG, Ogunleye AA (2021) Financial burden of lymphedema hospitalizations in the United States. JAMA Oncol 7(4):630–632. https://doi.org/10.1001/jamaoncol.2020.7891
De Vrieze T, Nevelsteen I, Thomis S et al (2020) What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Support Care Cancer 28(2):439–449. https://doi.org/10.1007/s00520-019-05101-8
Mercier G, Pastor J, Clément V, Rodts U, Moffat C, Quéré I (2019) Out-of-pocket payments, vertical equity and unmet medical needs in France: a national multicenter prospective study on lymphedema. PLoS One 14(5):e0216386. https://doi.org/10.1371/journal.pone.0216386
Moffatt CJ, Franks PJ, Doherty DC et al (2003) Lymphoedema: an underestimated health problem. QJM 96(10):731–738. https://doi.org/10.1093/qjmed/hcg126
Carrera PM, Kantarjian HM, Blinder VS (2018) The financial burden and distress of patients with cancer: understanding and step**-up action on the financial toxicity of cancer treatment. CA Cancer J Clin 68(2):153–165. https://doi.org/10.3322/caac.21443
Bygrave A, Whittaker K, Paul C, Fradgley EA, Varlow M, Aranda S (2021) Australian experiences of out-of-pocket costs and financial burden following a cancer diagnosis: a systematic review. Int J Environ Res Public Health 18(5):2422. https://doi.org/10.3390/ijerph18052422
Gutknecht M, Herberger K, Klose K, Purwins S, Dietz D, Blome C, Augustin M (2017) Cost-of-illness of patients with lymphoedema. J Eur Acad Dermatol Venereol 31(11):1930–1935. https://doi.org/10.1111/jdv.14442
The Joanna Briggs Institute (2016) Joanna Briggs Institute reviewers' manual. The Joanna Briggs Institute, Austrilia
Hong QN, Gonzalez-Reyes A, Pluye P (2018) Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract 24(3):459–467. https://doi.org/10.1111/jep.12884
Shih YC, Xu Y, Cormier JN et al (2009) Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol 27(12):2007–2014. https://doi.org/10.1200/JCO.2008.18.3517
Basta MN, Fox JP, Kanchwala SK et al (2016) Complicated breast cancer-related lymphedema: evaluating health care resource utilization and associated costs of management. Am J Surg 211(1):133–141. https://doi.org/10.1016/j.amjsurg.2015.06.015
Boyages J, Xu Y, Kalfa S et al (2017) Financial cost of lymphedema borne by women with breast cancer. Psychooncology 26(6):849–855. https://doi.org/10.1002/pon.4239
Dean LT, Moss SL, Ransome Y et al (2019) “It still affects our economic situation”: long-term economic burden of breast cancer and lymphedema. Support Care Cancer 27(5):1697–1708. https://doi.org/10.1007/s00520-018-4418-4
Dean LT, Ransome Y, Frasso-Jaramillo L et al (2019) Drivers of cost differences between US breast cancer survivors with or without lymphedema. J Cancer Surviv 13(5):804–814. https://doi.org/10.1007/s11764-019-00799-1
De Vrieze T, Gebruers N, Nevelsteen I et al (2021) Breast cancer-related lymphedema and its treatment: how big is the financial impact? Support Care Cancer 29(7):3801–3813. https://doi.org/10.1007/s00520-020-05890-3
Pitr K (2021) Economic and social aspects of secondary lymphedema following treatment of breast cancer. CSWHI 12(2):35–38. https://doi.org/10.22359/cswhi_12_2_06
Hens W, Vissers D, Annemans L, Gielen J, Van Gaal L, Taeymans J, Verhaeghe N (2018) Health-related costs in a sample of premenopausal non-diabetic overweight or obese females in Antwerp region: a cost-of-illness analysis. Arch Public Health 30(76):42. https://doi.org/10.1186/s13690-018-0285-1
Villar RR, Fernández SP, Garea CC, Pillado MTS, Barreiro VB, Martín CG (2017) Quality of life and anxiety in women with breast cancer before and after treatment. Rev Lat Am Enfermagem 25:e2958. Published 2017 Dec 21. https://doi.org/10.1590/1518-8345.2258.2958
Kalemikerakis I, Evaggelakou A, Kavga A, Vastardi M, Konstantinidis T, Govina O (2021) Diagnosis, treatment and quality of life in patients with cancer-related lymphedema. J BUON 26(5):1735–1741
Zhu Z, **ng W, Zhang X, Hu Y, So WKW (2020) Cancer survivors’ experiences with financial toxicity: a systematic review and meta-synthesis of qualitative studies. Psychooncology 29(6):945–959. https://doi.org/10.1002/pon.5361
Donkor A, Atuwo-Ampoh VD, Yakanu F, Torgbenu E, Ameyaw EK, Kitson-Mills D, Vanderpuye V, Kyei KA, Anim-Sampong S, Khader O, Khader J (2022) Financial toxicity of cancer care in low- and middle-income countries: a systematic review and meta-analysis. Support Care Cancer 30(9):7159–7190. https://doi.org/10.1007/s00520-022-07044-z
Boby JM, Rajappa S, Mathew A (2021) Financial toxicity in cancer care in India: a systematic review. Lancet Oncol 22(12):e541–e549. https://doi.org/10.1016/S1470-2045(21)00468-X
Weiss R (2016) Cost of a lymphedema treatment mandate-10 years of experience in the Commonwealth of Virginia. Health Econ Rev 6(1):42. https://doi.org/10.1186/s13561-016-0117-3 Epub 2016 Sep 2. Erratum in: Health Econ Rev. 2016 Dec;6(1):47. PMID: 27590738; PMCID: PMC5010541
Duygu Yildiz E, Bakar Y, Keser I (2022) What do lymphedema patients expect from a treatment and what do they achieve? A descriptive study. J Vasc Nurs 40(1):59–65. https://doi.org/10.1016/j.jvn.2022.01.002
Acknowledgements
The authors thank P.P. Wu, S.R. Wang, and Z.H. Zhao, for their kindly assistance with the methodological guidance.
Author information
Authors and Affiliations
Contributions
**gru Bian: conceptualization, data curation, formal analysis, writing — original draft, writing — review and editing; Aomei Shen: conceptualization, formal analysis, writing — review and editing; Wanwan Yang: data curation, formal analysis; Liyuan Zhang: data curation, formal analysis; Wanmin Qiang: supervision, writing — review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
As this is a systematic review reporting on existing data, ethics approval was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bian, J., Shen, A., Yang, W. et al. Financial toxicity experienced by patients with breast cancer-related lymphedema: a systematic review. Support Care Cancer 31, 354 (2023). https://doi.org/10.1007/s00520-023-07800-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07800-9