Abstract
Purpose
Morphine infusion through Intrathecal Drug Delivery System (IDDS) is widely used to relieve refractory cancer pain. However, continuous escalation of morphine dose caused by opioid tolerance and/or progress of cancer was commonly observed. Combining morphine with medications of different analgesic mechanisms is applied to blunt the rate of morphine increase. The purpose of this study was to determine the analgesic efficacy and safety of combining gabapentin with morphine after IDDS implantation.
Methods
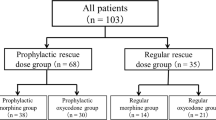
This study compared patients that received IDDS implantation from January 1, 2017 to November 10, 2018 in our institute. Key outcomes included change in mean pain score, dose of morphine used in patients, percentage of patients with 30% and 50% reduction in mean pain score, Patient Global Impression of Change scores, breakthrough pain characters and side effects.
Results
34 patients in the combination group (morphine + gabapentin) and 40 patients in the monotherapy group(morphine)were analyzed. The results showed that both therapy groups achieved similar analgesic efficacy, demonstrated by Numerical rating scale (2.42 ± 0.88 vs 2.57 ± 0.85; Combination vs Monotherapy), PGIC and responder status. Mean daily dose of morphine was significantly lower in combination group compared to monotherapy group (3.54 ± 1.29 mg vs 4.64 ± 1.28 mg, P = 0.007). More patients experienced dizziness and somnolence after receiving combination therapy compared to morphine-alone treatment although no statistical significance was found (P = 0.49).
Conclusion
Addition of gabapentin achieved similar analgesic efficacy with lower dose of morphine compared to morphine alone accompanying with higher incidence of dizziness and somnolence.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
IBM SPSS 24.0 software for Windows (SPSS, Inc., Chicago, IL, USA).
References
van den Beuken-van Everdingen MH et al (2007) Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 18(9):1437–1449
Mastenbroek TC et al (2017) Multimodal intrathecal analgesia in refractory cancer pain. Scand J Pain 14:39–43
Carvajal G et al (2018) Intrathecal Drug delivery systems for refractory pancreatic cancer pain: observational follow-up study over an 11-year period in a comprehensive cancer center. Anesth Analg 126(6):2038–2046
Smith TJ et al (2005) An implantable drug delivery system (IDDS) for refractory cancer pain provides sustained pain control, less drug-related toxicity, and possibly better survival compared with comprehensive medical management (CMM). Ann Oncol 16(5):825–833
Lavand’homme P, Steyaert A (2017) Opioid-free anesthesia opioid side effects: tolerance and hyperalgesia. Best Pract Res Clin Anaesthesiol 31(4):487–498
Capozza MA et al (2021) Narrative review of intrathecal drug delivery (IDD): indications, devices and potential complications. Ann Transl Med 9(2):186
McGeeney BE (2008) Adjuvant agents in cancer pain. Clin J Pain 24(Suppl 10):S14-20
Kiatchai T et al (2017) Effects of pregabalin on postoperative pain after hysterectomy under spinal anesthesia with intrathecal morphine: a randomized controlled trial. J Anesth 31(6):861–868
Jiang Y et al (2018) The efficacy of gabapentin in reducing pain intensity and morphine consumption after breast cancer surgery: a meta-analysis. Medicine (Baltimore) 97(38): e11581
Han C et al (2017) The efficacy of preoperative gabapentin in spinal surgery: a meta-analysis of randomized controlled trials. Pain Physician 20(7):649–661
Smith TJ et al (2002) Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol 20(19):4040–4049
Gierthmühlen J, Baron R (2016) Neuropathic pain. Semin Neurol 36(5):462–468
Kukkar A et al (2013) Implications and mechanism of action of gabapentin in neuropathic pain. Arch Pharm Res 36(3):237–251
Funding
The work was supported by Funding of Harbin Scientific-Technology Bureau (2016RAQXJ213) and Heilongjiang Postdoctoral Research Developmental Funding (LBH-Q14214).
Author information
Authors and Affiliations
Contributions
Protocol design, and manuscript writing: Huichao Zou; clinical practice: Lei Teng, Liuyuan Zhao, Hongxue Shao, Shiyan Lin, Wenhui Zhang; statistical analysis of data and manuscript.
review: Junzhu Dai.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was approved by the Institutional Review Board of Harbin Medical University Cancer Hospital. Written informed consent for participation was obtained from patients.
Consent for publication
All authors have read this manuscript and would like to have it considered exclusively for publication in Supportive Care in Cancer.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teng, L., Dai, J., Shao, H. et al. Gabapentin enhances the antinociceptive effect of intrathecal morphine in refractory cancer pain patients. Support Care Cancer 29, 7611–7616 (2021). https://doi.org/10.1007/s00520-021-06350-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06350-2