Abstract
Background and aims
The 30-day readmission rate is a nationally recognized quality measure with nearly one-fifth of patients being readmitted. This study aims to evaluate frailty, as measured by the hospital frailty risk score (HFRS), as a prognostic indicator for 30-day readmission after inpatient ERCP.
Methods
We analyzed weighted discharge records from the 2017 Nationwide Readmissions Database (NRD) to identify patients undergoing ERCP between 01/01/2017 and 11/30/2017. Our primary outcome was the 30-day unplanned readmission rate in frail (defined as HFRS > 5) against non-frail (HFRS < 5) patients. A mixed effects multivariable logistic regression method was employed.
Results
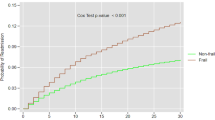
Among 68,206 weighted hospitalized patients undergoing ERCP, 31.3% were frail. Frailty was associated with higher 30-day readmission (OR 1.23, 95% CI [1.16–1.30]). Multivariable analysis showed a greater risk of readmission with cirrhosis (OR 1.26, 95% CI [1.10–1.45]), liver transplantation (OR 1.36, 95% CI [1.08–1.71]), cancer (OR 1.58, 95% CI [1.48–1.69]), and male gender (OR 1.24, 95% CI [1.18–1.31]). Frail patients also had higher mortality rate (1.8% vs 0.6%, p < 0.01)], longer LOS during readmission (6.7 vs 5.6 days, p < 0.01), and incurred more charges from both hospitalizations ($175,620 vs $132,519, p < 0.01). Sepsis was the most common primary indication for both frail and non-frail readmissions but accounted for a greater percentage of frail readmissions (17.9% vs 12.4%, p < 0.01).
Conclusions
Frailty is associated with higher readmission rates, mortality, LOS, and hospital charges for admitted patients undergoing ERCP. Sepsis is the leading cause for readmission. Independent risk factors for readmission include liver transplantation, cancer, cirrhosis, and male gender.


Similar content being viewed by others
Abbreviations
- ASGE:
-
American Society of Gastrointestinal Endoscopy
- AHRQ:
-
Agency for Healthcare Research and Quality
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence interval
- CMS:
-
Centers for Medicare & Medicaid Services
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- GI:
-
Gastroenterology
- HFRS:
-
Hospital frailty risk score
- HCUP:
-
Healthcare cost and utilization project
- ICD-10:
-
International statistical classification of diseases and related health problems version 10
- OR:
-
Odds ratio
References
Meseeha M, Attia M (2022) Endoscopic retrograde cholangiopancreatography. In: StatPearls. StatPearls Publishing, St. Petersburg. http://www.ncbi.nlm.nih.gov/books/NBK493160/. Accessed 2 Dec 2022
Andriulli A, Loperfido S, Napolitano G et al (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102(8):1781–1788. https://doi.org/10.1111/j.1572-0241.2007.01279.x
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360(14):1418–1428. https://doi.org/10.1056/NEJMsa0803563
Krill TS, Crain R, Al-Saadi Y et al (2020) Predictors of 30-day readmission after inpatient endoscopic retrograde cholangiopancreatography: a single-center experience. Dig Dis Sci 65(5):1481–1488. https://doi.org/10.1007/s10620-019-05870-6
Radadiya D, Devani K, Ashhab A et al (2022) US nationwide insight into all-cause 30-day readmissions following inpatient endoscopic retrograde cholangiopancreatography. J Clin Gastroenterol. https://doi.org/10.1097/MCG.0000000000001709
Navaneethan U, Gutierrez NG, Jegadeesan R et al (2013) Delay in performing ERCP and adverse events increase the 30-day readmission risk in patients with acute cholangitis. Gastrointest Endosc 78(1):81–90. https://doi.org/10.1016/j.gie.2013.02.003
Shah R, Haydek C, Mulki R, Qayed E (2018) Incidence and predictors of 30-day readmissions in patients hospitalized with chronic pancreatitis: a nationwide analysis. Pancreatol Off J Int Assoc Pancreatol 18(4):386–393. https://doi.org/10.1016/j.pan.2018.04.006
Xue QL (2011) The frailty syndrome: definition and natural history. Clin Geriatr Med 27(1):1–15. https://doi.org/10.1016/j.cger.2010.08.009
Gilbert T, Neuburger J, Kraindler J et al (2018) Development and validation of a hospital frailty risk score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet Lond Engl 391(10132):1775–1782. https://doi.org/10.1016/S0140-6736(18)30668-8
Martin L, Strom JB (2019) Utilization frailty and association with 30-day readmission and patient mortality under the hospital readmissions reduction program–part II. American College of Cardiology. https://www.acc.org/Latest-in-Cardiology/Articles/2019/12/10/06/54/Utilization-Frailty-and-Association-with-30-day-Readmission-and-Patient-Mortality-Under-the-Hospital-Readmissions-Reduction-Program-Part-II. Accessed 2 Dec 2022
Qian AS, Nguyen NH, Elia J, Ohno-Machado L, Sandborn WJ, Singh S (2021) Frailty is independently associated with mortality and readmission in hospitalized patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 19(10):2054-2063.e14. https://doi.org/10.1016/j.cgh.2020.08.010
Voora RS, Qian AS, Kotha NV et al (2022) Frailty index as a predictor of readmission in patients with head and neck cancer. Otolaryngology 167(1):89–96. https://doi.org/10.1177/01945998211043489
Zhou H, Della PR, Roberts P, Goh L, Dhaliwal SS (2016) Utility of models to predict 28-day or 30-day unplanned hospital readmissions: an updated systematic review. BMJ Open 6(6):e011060. https://doi.org/10.1136/bmjopen-2016-011060
Unal NG, Tekin F (2017) A new accurate model for predicting mortality up to 12 months after ERCP. Turk J Gastroenterol 28(3):235–237
Agency for Healthcare Research and Quality (2019) Introduction to the HCUP Nationwide Readmissions Database (NRD) 2010–2017. Healthcare Cost and Utilization Project (HCUP). https://www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2017.pdf
Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A (2019) Charlson Comorbidity Index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits 12(4):188–197
U.S. Centers for Medicare & Medicaid Services (2022) Hospital readmissions reduction program. cms.gov. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HRRP/Hospital-Readmission-Reduction-Program. Accessed 2 Dec 2022
Hao Q, Zhou L, Dong B, Yang M, Dong B, Weil Y (2019) The role of frailty in predicting mortality and readmission in older adults in acute care wards: a prospective study. Sci Rep 9(1):1207. https://doi.org/10.1038/s41598-018-38072-7
ASGE Standards of Practice Committee, Khashab MA, Chithadi KV et al (2015) Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 81(1):81–89. https://doi.org/10.1016/j.gie.2014.08.008
Jehan F, Khan M, Kulvatunyou N et al (2019) Day of hospital admission and effect on outcomes: the weekend effect in acute gallstone pancreatitis. J Surg Res 233:192–198. https://doi.org/10.1016/j.jss.2018.07.070
Hakim S, Aneese AM, Edhi A et al (2020) A statistically significant reduction in length of stay and hospital costs with equivalent quality of care metrics for ERCPs performed during the weekend versus postponed to weekdays: a 6-year study of 533 ERCPs at four teaching hospitals. Dig Dis Sci 65(11):3132–3142. https://doi.org/10.1007/s10620-020-06066-z
Martin JA (2020) Non-emergent weekend ERCP: it makes sense-now, make it work. Dig Dis Sci 65(11):3057–3060. https://doi.org/10.1007/s10620-020-06312-4
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Khanh Hoang Nicholas Le, Alexander S. Qian, Mimi Nguyen, Edmund Qiao, Phuong Nguyen, Siddharth Singh, and Mary Lee Krinsky have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le, K.H.N., Qian, A.S., Nguyen, M. et al. The hospital frailty risk score as a predictor of readmission after ERCP. Surg Endosc 38, 260–269 (2024). https://doi.org/10.1007/s00464-023-10531-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10531-x