Abstract
Background
Vonoprazan is a new potassium-competitive acid blocker (P-CAB) that was recently approved by the FDA. It is associated with a fast onset of action and a longer acid inhibition time. Vonoprazan-containing therapy for helicobacter pylori eradication is highly effective and several studies have demonstrated that a vonoprazan-antibiotic regimen affects gut microbiota. However, the impact of vonoprazan alone on gut microbiota is still unclear.
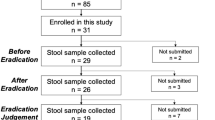
Methods
We conducted a prospective randomized 12-week experimental trial with 18 Wistar rats. Rats were randomly assigned to one of 3 groups: (1) drinking water as negative control group, (2) oral vonoprazan (4 mg/kg) for 12 weeks, and (3) oral vonoprazan (4 mg/kg) for 4 weeks, followed by 8 weeks off vonoprazan. To investigate gut microbiota, we carried out a metagenomic shotgun sequencing of fecal samples at week 0 and week 12.
Results
For alpha diversity metrics at week 12, both long and short vonoprazan groups had lower Pielou’s evenness index than the control group (p = 0.019); however, observed operational taxonomic units (p = 0.332) and Shannon’s diversity index (p = 0.070) were not statistically different between groups. Beta diversity was significantly different in the three groups, using Bray–Curtis (p = 0.003) and Jaccard distances (p = 0.002). At week 12, differences in relative abundance were observed at all levels. At phylum level, short vonoprazan group had less of Actinobacteria (log fold change = − 1.88, adjusted p-value = 0.048) and Verrucomicrobia (lfc = − 1.76, p = 0.009).
At the genus level, long vonoprazan group had more Bacteroidales (lfc = 5.01, p = 0.021) and Prevotella (lfc = 7.79, p = 0.001). At family level, long vonoprazan group had more Lactobacillaceae (lfc = 0.97, p = 0.001), Prevotellaceae (lfc = 8.01, p < 0.001), and less Erysipelotrichaceae (lfc = − 2.9, p = 0.029).
Conclusion
This study provides evidence that vonoprazan impacts the gut microbiota and permits a precise delineation of the composition and relative abundance of the bacteria at all different taxonomic levels.







Similar content being viewed by others
References
Sachs G, Shin JM, Vagin O, Lambrecht N, Yakubov I, Munson K (2007) The gastric H, K atpase as a drug target: past, present, and future. J Clin Gastroenterol 41:S226–S242. https://doi.org/10.1097/MCG.0b013e31803233b7
Chey WD, Mody RR, Izat E (2010) Patient and physician satisfaction with proton pump inhibitors (PPIs): are there opportunities for improvement? Dig Dis Sci 55:3415–3422. https://doi.org/10.1007/s10620-010-1209-2
Luo H-J, Deng W-Q, Zou K (2014) Protonated form: the potent form of potassium-competitive acid blockers. PLoS ONE 9:97688. https://doi.org/10.1371/journal.pone.0097688
Sachs G, Shin JM, Hunt R (2010) Novel approaches to inhibition of gastric acid secretion. Curr Gastroenterol Rep 12:437–447. https://doi.org/10.1007/s11894-010-0149-5
Shin JM, Inatomi N, Munson K, Strugatsky D, Tokhtaeva E, Vagin O, Sachs G (2011) Characterization of a novel potassium-competitive acid blocker of the Gastric H, K-ATPase, 1-[5-(2-Fluorophenyl)-1-(pyridin-3-ylsulfonyl)-1 H-pyrrol-3-yl]-N-ethylmethanamine monofumarate (TAK-438). J Pharmacol Exp Ther 339:412–420. https://doi.org/10.1124/jpet.111.185314
Garnock-Jones KP (2015) Vonoprazan: first global approval. Drugs 75:439–443. https://doi.org/10.1007/s40265-015-0368-z
Chen F, Jiang H, Xu J, Wang S, Meng D, Geng P, Dai D, Zhou Q, Zhou Y (2020) In vitro and in vivo rat model assessments of the effects of vonoprazan on the pharmacokinetics of venlafaxine. DDDT 14:4815–4824. https://doi.org/10.2147/DDDT.S276704
Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R (2012) Diversity, stability and resilience of the human gut microbiota. Nature 489:220–230. https://doi.org/10.1038/nature11550
Kamada N, Chen GY, Inohara N, Núñez G (2013) Control of pathogens and pathobionts by the gut microbiota. Nat Immunol 14:685–690. https://doi.org/10.1038/ni.2608
Ley RE, Turnbaugh PJ, Klein S, Gordon JI (2006) Human gut microbes associated with obesity. Nature 444:1022–1023. https://doi.org/10.1038/4441022a
Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI (2011) Human nutrition, the gut microbiome and the immune system. Nature 474:327–336. https://doi.org/10.1038/nature10213
Qiu P, Ishimoto T, Fu L, Zhang J, Zhang Z, Liu Y (2022) The gut microbiota in inflammatory bowel disease. Front Cell Infect Microbiol 12:733992. https://doi.org/10.3389/fcimb.2022.733992
Kandpal M, Indari O, Baral B, Jakhmola S, Tiwari D, Bhandari V, Pandey RK, Bala K, Sonawane A, Jha HC (2022) Dysbiosis of gut microbiota from the perspective of the gut-brain axis: role in the provocation of neurological disorders. Metabolites 12:1064. https://doi.org/10.3390/metabo12111064
Mei S, Deng Z, Chen Y, Ning D, Guo Y, Fan X, Wang R, Meng Y, Zhou Q, Tian X (2022) Dysbiosis: the first hit for digestive system cancer. Front Physiol 13:1040991. https://doi.org/10.3389/fphys.2022.1040991
Hori Y, Matsukawa J, Takeuchi T, Nishida H, Ka**o M, Inatomi N (2011) A study comparing the antisecretory effect of TAK-438, a novel potassium-competitive acid blocker, with lansoprazole in animals. J Pharmacol Exp Ther 337:797–804. https://doi.org/10.1124/jpet.111.179556
Blanco-Miguez A, Beghini F, Cumbo F, McIver LJ, Thompson KN, Zolfo M, Manghi P, Dubois L, Huang KD, Thomas AM, Piccinno G, Piperni E, Punčochář M, Valles-Colomer M, Tett A, Giordano F, Davies R, Wolf J, Berry SE, Spector TD, Franzosa EA, Pasolli E, Asnicar F, Huttenhower C, Segata N (2022) Extending and improving metagenomic taxonomic profiling with uncharacterized species with MetaPhlAn 4. Bioinformatics 15:1–2
Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet CC, Al-Ghalith GA, Alexander H, Alm EJ, Arumugam M, Asnicar F, Bai Y, Bisanz JE, Bittinger K, Brejnrod A, Brislawn CJ, Brown CT, Callahan BJ, Caraballo-Rodríguez AM, Chase J, Cope EK, Da Silva R, Diener C, Dorrestein PC, Douglas GM, Durall DM, Duvallet C, Edwardson CF, Ernst M, Estaki M, Fouquier J, Gauglitz JM, Gibbons SM, Gibson DL, Gonzalez A, Gorlick K, Guo J, Hillmann B, Holmes S, Holste H, Huttenhower C, Huttley GA, Janssen S, Jarmusch AK, Jiang L, Kaehler BD, Kang KB, Keefe CR, Keim P, Kelley ST, Knights D, Koester I, Kosciolek T, Kreps J, Langille MGI, Lee J, Ley R, Liu Y-X, Loftfield E, Lozupone C, Maher M, Marotz C, Martin BD, McDonald D, McIver LJ, Melnik AV, Metcalf JL, Morgan SC, Morton JT, Naimey AT, Navas-Molina JA, Nothias LF, Orchanian SB, Pearson T, Peoples SL, Petras D, Preuss ML, Pruesse E, Rasmussen LB, Rivers A, Robeson MS, Rosenthal P, Segata N, Shaffer M, Shiffer A, Sinha R, Song SJ, Spear JR, Swafford AD, Thompson LR, Torres PJ, Trinh P, Tripathi A, Turnbaugh PJ, Ul-Hasan S, van der Hooft JJJ, Vargas F, Vázquez-Baeza Y, Vogtmann E, von Hippel M, Walters W, Wan Y, Wang M, Warren J, Weber KC, Williamson CHD, Willis AD, Xu ZZ, Zaneveld JR, Zhang Y, Zhu Q, Knight R, Caporaso JG (2019) Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol 37:852–857. https://doi.org/10.1038/s41587-019-0209-9
Lin H, Peddada SD (2020) Analysis of compositions of microbiomes with bias correction. Nat Commun 11:3514. https://doi.org/10.1038/s41467-020-17041-7
Jackson MA, Verdi S, Maxan M-E, Shin CM, Zierer J, Bowyer RCE, Martin T, Williams FMK, Menni C, Bell JT, Spector TD, Steves CJ (2018) Gut microbiota associations with common diseases and prescription medications in a population-based cohort. Nat Commun 9:2655. https://doi.org/10.1038/s41467-018-05184-7
Jackson MA, Goodrich JK, Maxan M-E, Freedberg DE, Abrams JA, Poole AC, Sutter JL, Welter D, Ley RE, Bell JT, Spector TD, Steves CJ (2016) Proton pump inhibitors alter the composition of the gut microbiota. Gut 65:749–756. https://doi.org/10.1136/gutjnl-2015-310861
MetaHIT consortium, Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, Prifti E, Vieira-Silva S, Gudmundsdottir V, Krogh Pedersen H, Arumugam M, Kristiansen K, Yvonne Voigt A, Vestergaard H, Hercog R, Igor Costea P, Roat Kultima J, Li J, Jørgensen T, Levenez F, Dore J, Bjørn Nielsen H, Brunak S, Raes J, Hansen T, Wang J, Dusko Ehrlich S, Bork P, Pedersen O (2015) Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528:262–266. https://doi.org/10.1038/nature15766
Dethlefsen L, Relman DA (2011) Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci USA 108:4554–4561. https://doi.org/10.1073/pnas.1000087107
Imhann F, Vich Vila A, Bonder MJ, Lopez Manosalva AG, Koonen DPY, Fu J, Wijmenga C, Zhernakova A, Weersma RK (2017) The influence of proton pump inhibitors and other commonly used medication on the gut microbiota. Gut Microbes 8:351–358. https://doi.org/10.1080/19490976.2017.1284732
Hojo M, Asahara T, Nagahara A, Takeda T, Matsumoto K, Ueyama H, Matsumoto K, Asaoka D, Takahashi T, Nomoto K, Yamashiro Y, Watanabe S (2018) Gut Microbiota Composition Before and After Use of Proton Pump Inhibitors. Dig Dis Sci 63:2940–2949. https://doi.org/10.1007/s10620-018-5122-4
Imhann F, Bonder MJ, Vich Vila A, Fu J, Mujagic Z, Vork L, Tigchelaar EF, Jankipersadsing SA, Cenit MC, Harmsen HJM, Dijkstra G, Franke L, Xavier RJ, Jonkers D, Wijmenga C, Weersma RK, Zhernakova A (2016) Proton pump inhibitors affect the gut microbiome. Gut 65:740–748. https://doi.org/10.1136/gutjnl-2015-310376
Yang Y-CSH, Chang H-W, Lin I-H, Chien L-N, Wu M-J, Liu Y-R, Chu PG, **e G, Dong F, Jia W, Chang VHS, Yen Y (2020) Long-term proton pump inhibitor administration caused physiological and microbiota changes in rats. Sci Rep 10:866. https://doi.org/10.1038/s41598-020-57612-8
Zhernakova A, Kurilshikov A, Bonder MJ, Tigchelaar EF, Schirmer M, Vatanen T, Mujagic Z, Vila AV, Falony G, Vieira-Silva S, Wang J, Imhann F, Brandsma E, Jankipersadsing SA, Joossens M, Cenit MC, Deelen P, Swertz MA, LifeLines cohort study, Weersma RK, Feskens EJM, Netea MG, Gevers D, Jonkers D, Franke L, Aulchenko YS, Huttenhower C, Raes J, Hofker MH, Xavier RJ, Wijmenga C, Fu J (2016) Population-based metagenomics analysis reveals markers for gut microbiome composition and diversity. Science 352:565–569. https://doi.org/10.1126/science.aad3369
Ashida K, Sakurai Y, Hori T, Kudou K, Nishimura A, Hiramatsu N, Umegaki E, Iwakiri K (2016) Randomised clinical trial: vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the healing of erosive oesophagitis. Aliment Pharmacol Ther 43:240–251. https://doi.org/10.1111/apt.13461
Hori Y, Imanishi A, Matsukawa J, Tsukimi Y, Nishida H, Arikawa Y, Hirase K, Ka**o M, Inatomi N (2010) 1-[5-(2-Fluorophenyl)-1-(pyridin-3-ylsulfonyl)-1 H -pyrrol-3-yl]- N-methylmethanamine Monofumarate (TAK-438), a novel and potent potassium-competitive acid blocker for the treatment of acid-related diseases. J Pharmacol Exp Ther 335:231–238. https://doi.org/10.1124/jpet.110.170274
Kim B-R, Shin J, Guevarra RB, Lee JH, Kim DW, Seol K-H, Lee J-H, Kim HB, Isaacson RE (2017) Deciphering diversity indices for a better understanding of microbial communities. J Microbiol Biotechnol 27:2089–2093. https://doi.org/10.4014/jmb.1709.09027
Hu Y, Xu X, Ouyang Y, He C, Li N, **e C, Peng C, Zhu Z, **e Y, Shu X, Lu N, Zhu Y (2022) Analysis of oral microbiota alterations induced by Helicobacter pylori infection and vonoprazan-amoxicillin dual therapy for Helicobacter pylori eradication. Helicobacter. https://doi.org/10.1111/hel.12923
Suzuki S, Gotoda T, Takano C, Horii T, Sugita T, Ogura K, Ichijima R, Kusano C, Ikehara H (2021) Long term impact of vonoprazan-based Helicobacter pylori treatment on gut microbiota and its relation to post-treatment body weight changes. Helicobacter. https://doi.org/10.1111/hel.12851
Kakiuchi T, Yamamoto K, Imamura I, Hashiguchi K, Kawakubo H, Yamaguchi D, Fujioka Y, Okuda M (2021) Gut microbiota changes related to Helicobacter pylori eradication with vonoprazan containing triple therapy among adolescents: a prospective multicenter study. Sci Rep 11:755. https://doi.org/10.1038/s41598-020-80802-3
Zhang M, Yang X-J (2016) Effects of a high fat diet on intestinal microbiota and gastrointestinal diseases. WJG 22:8905. https://doi.org/10.3748/wjg.v22.i40.8905
Horii T, Suzuki S, Takano C, Shibuya H, Ichijima R, Kusano C, Ikehara H, Gotoda T (2021) Lower impact of vonoprazan–amoxicillin dual therapy on gut microbiota for Helicobacter pylori eradication. J Gastro Hepatol 36:3314–3321. https://doi.org/10.1111/jgh.15572
Cornejo-Pareja I, Martín-Núñez G, Roca-Rodríguez M, Cardona F, Coin-Aragüez L, Sánchez-Alcoholado L, Gutiérrez-Repiso C, Muñoz-Garach A, Fernández-García J, Moreno-Indias I, Tinahones F (2019) H. pylori eradication treatment alters gut microbiota and GLP-1 secretion in humans. JCM 8:451. https://doi.org/10.3390/jcm8040451
Scheperjans F, Aho V, Pereira PAB, Koskinen K, Paulin L, Pekkonen E, Haapaniemi E, Kaakkola S, Eerola-Rautio J, Pohja M, Kinnunen E, Murros K, Auvinen P (2015) Gut microbiota are related to Parkinson’s disease and clinical phenotype. Mov Disord 30:350–358. https://doi.org/10.1002/mds.26069
Sanada K, Nakajima S, Kurokawa S, Barceló-Soler A, Ikuse D, Hirata A, Yoshizawa A, Tomizawa Y, Salas-Valero M, Noda Y, Mimura M, Iwanami A, Kishimoto T (2020) Gut microbiota and major depressive disorder: A systematic review and meta-analysis. J Affect Disord 266:1–13. https://doi.org/10.1016/j.jad.2020.01.102
Barandouzi ZA, Starkweather AR, Henderson WA, Gyamfi A, Cong XS (2020) Altered Composition of gut microbiota in depression: a systematic review. Front Psychiatry 11:541. https://doi.org/10.3389/fpsyt.2020.00541
Reeves AE, Theriot CM, Bergin IL, Huffnagle GB, Schloss PD, Young VB (2011) The interplay between microbiome dynamics and pathogen dynamics in a murine model of Clostridium difficile Infection. Gut Microbes 2:145–158. https://doi.org/10.4161/gmic.2.3.16333
Funding
This study was internally funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Rasa Zarnegar works as a consultant for Bard (BD). Drs. Haythem Najah, Rodrigo C.L. Edelmuth, Maria Cristina Riascos, Alex Grier, Hala Al Asadi, Jacques A. Greenberg, Ileana Miranda, Carl V. Crawford, Brendan M. Finnerty, and Thomas J. Fahey III have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Najah, H., Edelmuth, R.C.L., Riascos, M.C. et al. Long-term potassium-competitive acid blockers administration causes microbiota changes in rats. Surg Endosc 37, 7980–7990 (2023). https://doi.org/10.1007/s00464-023-10269-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10269-6