Abstract
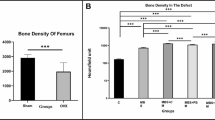
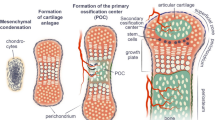
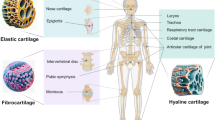
Partial-thickness articular cartilage defects (PTCDs) do not heal spontaneously and are thought to be a predisposing factor for the development of osteoarthritis. Younger and smaller animals have a better healing capacity for many types of injuries including those to articular cartilage. Our aim was to examine the longitudinal histological changes of immature murine articular cartilage after the creation of small PTCDs and to compare them to PTCDs in mature cartilage. Single linear PTCDs were created in 3-week-old and 16-week-old rats in the direction of joint motion. At 6 and 12 weeks after PTCD creation, histological changes were examined in the defect sites and surrounding cartilage. Immature cartilage showed a higher repair capability than mature cartilage. Although repaired immature cartilage had fibrocartilage, it exhibited better quality than any PTCD model, except for a fetus model and comparable quality to full-thickness cartilage defects (FTCD) after bone marrow stimulation. Elucidation of the underlining mechanisms that immature cartilage possesses for repairing PTCDs is necessary in order to aid the prevention or develop treatment for osteoarthritis.




Similar content being viewed by others
References
Alford JW, Cole BJ (2005) Cartilage restoration, part 1: basic science, historical perspective, patient evaluation, and treatment options. Am J Sports Med 33:295–306
Arøen A, Løken S, Heir S, Alvik E, Ekeland A, Granlund OG, Engebretsen L (2004) Articular cartilage lesions in 993 consecutive knee arthroscopies. Am J Sports Med 32:211–215
Brooks PM (2006) The burden of musculoskeletal disease—a global perspective. Clin Rheumatol 25:778–781
Buckwalter JA (2002) Articular cartilage injuries. Clin Orthop Relat Res 402:21–37
Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G (2005) Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults. Arthritis Rheum 52:2033–2039
Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG (1997) Cartilage injuries: a review of 31,516 knee arthroscopies. Atrhroscopy 13:456–460
Dausse Y, Grossin L, Miralles G, Pelletier S, Mainard D, Hubert P, Baptiste D, Gillet P, Dellacherie E, Netter P, Payan E (2003) Cartilage repair using new polysaccharidic biomaterials: macroscopic, histological and biochemical approaches in a rat model of cartilage defect. Osteoarthritis Cartilage 11:16–28
Dowthwaite GP, Bishop JC, Redman SN, Khan IM, Rooney P, Evans DJ, Haughton L, Bayram Z, Boyer S, Thomson B, Wolfe MS, Archer CW (2004) The surface of articular cartilage contains a progenitor cell population. J Cell Sci 117 (Pt 6):889–897
Hanie EA, Sullins KE, Powers BE, Nelson PR (1992) Healing of full-thickness cartilage compared with full-thickness cartilage and subchondral bone defects in the equine third carpal bone. Equine Vet J 24:382–386
Hembry RM, Dyce J, Driesang I, Hunziker EB, Fosang AJ, Tyler JA, Murphy G (2001) Immunolocalization of matrix metalloproteinases in partial-thickness defects in pig articular cartilage. A preliminary report. J Bone Joint Surg Am 83:826–838
Hunziker EB, Quinn TM (2003) Surgical removal of articular cartilage leads to loss of chondrocytes from cartilage bordering the wound edge. J Bone Joint Surg Am 85-A (Suppl 2):85–92
Hunziker EB, Rosenberg LC (1996) Repair of partial-thickness defects in articular cartilage: cell recruitment from the synovial membrane. J Bone Joint Surg Am 78:721–733
Jansen EJ, Emans PJ, Van Rhijn LW, Bulstra SK, Kuijer R (2008) Development of partial-thickness articular cartilage injury in a rabbit model. Clin Orthop Relat Res 466:487–494
Kurth TB, Dell'accio F, Crouch V, Augello A, Sharpe PT, De Bari C (2011) Functional mesenchymal stem cell niches in adult mouse knee joint synovium in vivo. Arthritis Rheum 63:1289–1300
Lu Y, Markel MD, Swain C, Kaplan LD (2006) Development of partial thickness articular cartilage injury in an ovine model. J Orthop Res 24:1974–1982
Mankin HJ (1982) The response of articular cartilage to mechanical injury. J Bone Joint Surg Am 64:460–466
Mankin HJ, Dorfman H, Lippiello L, Zarins A (1971) Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips: correlation of morphology with biochemical and metabolic data. J Bone Joint Surg Am 53:523–537
Mastbergen SC, Marijnissen AC, Vianen ME, Roermund PM van, Bijlsma JW, Lafeber FP (2006) The canine “groove” model of osteoarthritis is more than simply the expression of surgically applied damage. Osteoarthritis Cartilage 14:39–46
Milentijevic D, Rubel IF, Liew AS, Helfet DL, Torzilli PA (2005) An in vivo rabbit model for cartilage trauma: a preliminary study of the influence of impact stress magnitude on chondrocyte death and matrix damage. J Orthop Trauma 19:466–473
Mizuta H, Kudo S, Nakamura E, Otsuka Y, Takagi K, Hiraki Y (2004) Active proliferation of mesenchymal cells prior to the chondrogenic repair response in rabbit full-thickness defects of articular cartilage. Osteoarthritis Cartilage 12:586–596
Mizuta H, Kudo S, Nakamura E, Takagi K, Hiraki Y (2006) Expression of the PTH/PTHrP receptor in chondrogenic cells during the repair of full-thickness defects of articular cartilage. Osteoarthritis Cartilage 14:944–952
Mrugala D, Bony C, Neves N, Caillot L, Fabre S, Moukoko D, Jorgensen C, Noël D (2008) Phenotypic and functional characterisation of ovine mesenchymal stem cells: application to a cartilage defect model. Ann Rheum Dis 67:288–295
Namba RS, Meuli M, Sullivan KM, Le AX, Adzick NS (1998) Spontaneous repair of superficial defects in articular cartilage in a fetal lamb model. J Bone Joint Surg Am 80:4–10
Nixon AJ, Begum L, Mohammed HO, Huibregtse B, O'Callaghan MM, Matthews GL (2011) Autologous chondrocyte implantation drives early chondrogenesis and organized repair in extensive full- and partial-thickness cartilage defects in an equine model. J Orthop Res 29:1121–1130
Ueda H (1997) Effect of physical exercise for the rat at the growth stage on bone tissue—on cortex of diaphysis of tibia. J Kyushu Dent 51:383–405
Wakitani S, Goto T, Pineda SJ, Young JM, Mansour RG, Caplan AI, Goldberg VM (1994) Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am 76:579–592
Watrin-Pinzano A, Loeuille D, Goebel JC, Lapicque F, Walter F, Robert P, Netter P, Corot C, Gillet P, Blum A (2008) Quantitative dynamic contrast enhanced MRI of experimental synovitis in the rabbit knee: comparison of macromolecular blood pool agents vs. gadolinium-DOTA. Biomed Mater Eng 18:261–272
Wei X, Messner K (1999) Maturation-dependent durability of spontaneous cartilage repair in rabbit knee joint. J Biomed Mater Res 46:539–548
Wei X, Gao J, Messner K (1997) Maturation-dependent repair of untreated osteochondral defects in the rabbit knee joint. J Biomed Mater Res 34:63–72
Yoshioka M, Kubo T, Coutts RD, Hirasawa Y (1998) Differences in the repair process of longitudinal and transverse injuries of cartilage in the rat knee. Osteoarthritis Cartilage 6:66–75
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by a Grant-in Aid for Scientific Research (C) of the Japan Society for the Promotion of Science (JPJS), grant number 2591675.
Rights and permissions
About this article
Cite this article
Tsuruoka, H., Sasho, T., Yamaguchi, S. et al. Maturation-dependent spontaneous healing of partial thickness cartilage defects in infantile rats. Cell Tissue Res 346, 263–271 (2011). https://doi.org/10.1007/s00441-011-1259-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-011-1259-6