Abstract
Background
Studies have demonstrated that non-acid reflux (NAR) is associated with esophageal squamous cell carcinoma (ESCC). Esophageal dysmotility is associated with NAR but few studies have focused on the esophageal motility of ESCC patients. We explored the relationship between ESCC, NAR and esophageal dysmotility with the aid of multichannel intraluminal impedance and pH (MII-pH) and high-resolution manometry (HRM).
Methods
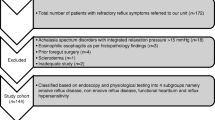
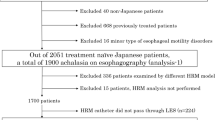
From Jan 2021 to Oct 2022, 20 patients with superficial ESCC were enrolled as the ESCC group, while 20 age and gender matched individuals without gastroesophageal reflux disease (GERD) symptoms and 20 age and gender matched patients with GERD symptoms were recruited as the control groups. Patients received 24 h MII-pH and HRM procedure before endoscopic submucosal dissection (ESD), and the data were then collected to identify the type of reflux and esophageal dysmotility.
Results
Prevalence of esophageal dysmotility was significantly different among the three groups, 75.0% in the ESCC group, 35.0% in the non-GERD group and 70.0% in the GERD group (P = 0.029). NAR episodes at 15 cm above the lower esophageal sphincter (LES) in the ESCC group were significantly higher than that in the non-GERD group (6.5 (3.5–9.3) vs 1.0 (0.8–4.0), P = 0.001) and were similar with that in the GERD group (6.5 (3.5–9.3) vs 5.5 (3.0–10.5), P > 0.05). NAR episodes at 5 cm above LES was significantly higher in the ESCC group than that in the non-GERD group (38.0 (27.0–60.0) vs 18.0 (11.8–25.8), P = 0.001) and was significantly higher than that in the GERD group (38.0 (27.0–60.0) vs 20.0 (9.8–30.5)), P = 0.010). Prevalence of pathologic non-acid reflux was significantly different among the three groups, 30.0% in the ESCC group, 0.0% in the non-GERD group and 10.0% in the GERD group (P < 0.001).
Conclusion
Our study found NAR and esophageal dysfunction frequently occur in ESCC patients. NAR and esophageal dysmotility may be associated with ESCC.
Clinical trial registration number
ChiCTR2200061456.



Similar content being viewed by others
Data availability
All data included in this study are available upon request by contact with the corresponding author.
References
Banki F et al (2005) Barrett’s esophagus in females: a comparative analysis of risk factors in females and males. Am J Gastroenterol 100(3):560–567
Brandt MG, Darling GE, Miller L (2004) Symptoms, acid exposure and motility in patients with Barrett’s esophagus. Can J Surg 47(1):47–51
Cook MB et al (2010) Serum pepsinogens and Helicobacter pylori in relation to the risk of esophageal squamous cell carcinoma in the alpha-tocopherol, beta-carotene cancer prevention study. Cancer Epidemiol Biomarkers Prev 19(8):1966–1975
de Vries AC et al (2009) Increased risk of esophageal squamous cell carcinoma in patients with gastric atrophy: independent of the severity of atrophic changes. Int J Cancer 124(9):2135–2138
Endoscopic Classification Review Group (2005) Update on the Paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy 37(6):570–578
Freedman ND et al (2007) A prospective study of tobacco, alcohol, and the risk of esophageal and gastric cancer subtypes. Am J Epidemiol 165(12):1424–1433
Furuta GT, Katzka DA (2015) Eosinophilic esophagitis. N Engl J Med 373(17):1640–1648
Gyawali CP et al (2018) Modern diagnosis of GERD: the Lyon consensus. Gut 67(7):1351–1362
Hachem C, Shaheen NJ (2016) Diagnosis and management of functional heartburn. Am J Gastroenterol 111(1):53–61
Herregods TV, Bredenoord AJ, Smout AJ (2015) Pathophysiology of gastroesophageal reflux disease: new understanding in a new era. Neurogastroenterol Motil 27(9):1202–1213
Iijima K et al (2010) Gastric hyposecretion in esophageal squamous-cell carcinomas. Dig Dis Sci 55(5):1349–1355
Kgomo M, Mokoena TR, Ker JA (2017) Non-acid gastro-oesophageal reflux is associated with squamous cell carcinoma of the oesophagus. BMJ Open Gastroenterol 4(1):e000180
Lagergren J et al (1999) Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med 340(11):825–831
Lagergren J et al (2017) Oesophageal cancer. Lancet 390(10110):2383–2396
Lee TY et al (2008) Barrett’s esophagus and severe reflux esophagitis share common pathophysiological characteristics among Chinese in Taiwan. Intern Med 47(20):1767–1773
Lord RV et al (2009) Hiatal hernia, lower esophageal sphincter incompetence, and effectiveness of Nissen fundoplication in the spectrum of gastroesophageal reflux disease. J Gastrointest Surg 13(4):602–610
Oikawa T et al (2010) Deficient aldehyde dehydrogenase 2 is associated with increased risk for esophageal squamous cell carcinoma in the presence of gastric hypochlorhydria. Scand J Gastroenterol 45(11):1338–1344
Porter RF et al (2012) Fragmented esophageal smooth muscle contraction segments on high resolution manometry: a marker of esophageal hypomotility. Neurogastroenterol Motil 24(8):763-e353
Reddy CA et al (2019) High-resolution manometry diagnosis of ineffective esophageal motility is associated with higher reflux burden. Dig Dis Sci 64(8):2199–2205
Roman S et al (2017) Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: update of the Porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil 29(10):1–15
Savarino E et al (2011) Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 34(4):476–486
Savarino E, Giacchino M, Savarino V (2013) Dysmotility and reflux disease. Curr Opin Otolaryngol Head Neck Surg 21(6):548–556
Segawa K et al (1988) Chronic alcohol abuse leads to gastric atrophy and decreased gastric secretory capacity: a histological and physiological study. Am J Gastroenterol 83(4):373–379
Soroush A, Etemadi A, Abrams JA (2022) Non-acid fluid exposure and esophageal squamous cell carcinoma. Dig Dis Sci 67(7):2754–2762
Takahashi K et al (2017) Changes in esophageal motility after endoscopic submucosal dissection for superficial esophageal cancer: a high-resolution manometry study. Dis Esophagus 30(11):1–8
Takeda T et al (2018) Effect of esophageal endoscopic submucosal dissection on motility and symptoms: a prospective study. Gastroenterol Res Pract 2018:3735473
Triadafilopoulos G et al (2016) Clinical and pH study characteristics in reflux patients with and without ineffective oesophageal motility (IEM). BMJ Open Gastroenterol 3(1):e000126
Uno K et al (2011) Direct measurement of gastroesophageal reflux episodes in patients with squamous cell carcinoma by 24-h pH-impedance monitoring. Am J Gastroenterol 106(11):1923–1929
Wild CP et al (2020) World cancer report: cancer research for cancer prevention. International Agency for Research on Cancer, Lyon. http://publications.iarc.fr/586
Yadlapati R et al (2021) Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil 33(1):e14058
Yokoyama A et al (2009) Chronic atrophic gastritis and metachronous gastric cancer in Japanese alcoholic men with esophageal squamous cell carcinoma. Alcohol Clin Exp Res 33(5):898–905
Zerbib F et al (2006) Esophageal pH-impedance monitoring and symptom analysis in GERD: a study in patients off and on therapy. Am J Gastroenterol 101(9):1956–1963
Zerbib F et al (2020) Ineffective esophageal motility and bolus clearance. A study with combined high-resolution manometry and impedance in asymptomatic controls and patients. Neurogastroenterol Motil 32(9):e13876
Funding
This work was supported in part by the National Natural Science Foundation of China (NSFC) under Grants 82100567and 81770540, in part by the Key Research and Development Projects of Shaanxi Province under Grants 2021sf-135.
Author information
Authors and Affiliations
Contributions
Design: JW, NL, and BQ. Conception: BQ, BZ, and YH. Data extraction: YH and XX. Data analysis and drafting of the manuscript: YH, MW and YZ. Statistical analysis: YH, XJ, and QR.
Corresponding authors
Ethics declarations
Conflict of interest
There was no conflict of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yujie Hao and Mo Wang are equally contributed to this work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hao, Y., Wang, M., Jiang, X. et al. Non-acid reflux and esophageal dysmotility is associated with early esophageal squamous cell carcinoma. J Cancer Res Clin Oncol 149, 8327–8334 (2023). https://doi.org/10.1007/s00432-023-04772-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04772-5