Abstract
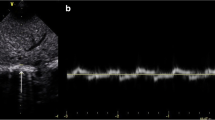
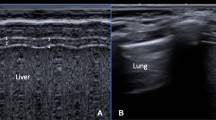
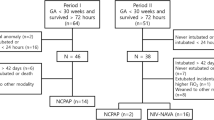
NIV-NAVA mode for respiratory support in preterm infants is not well-studied. This study aimed to describe the diaphragmatic function, diaphragmatic excursion (DE), and thickness fraction (DTF), in preterm infants < 30 weeks’ gestation supported by NIV-NAVA compared to NIPPV using bedside ultrasonography. In this consecutive prospective study, DE, diaphragmatic thickness at end of expiration (DTexp), end of inspiration (DTins), and DTF were assessed using bedside ultrasound. Lung aeration evaluation using lung ultrasound score (LUS) was performed for the two groups. Diaphragmatic measurements and LUS were compared for the 2 groups (NIV-NAVA group versus NIPPV group). Statistical analyses were conducted using the SPSS software version 22. Out of 70 infants evaluated, 40 were enrolled. Twenty infants were on NIV-NAVA and 20 infants on NIPPV with a mean [SD] study age of 25.7 [0.9] weeks and 25.1 [1.4] weeks respectively (p = 0.15). Baseline characteristics and respiratory parameters at the time of the scan showed no significant difference between groups. DE was significantly higher in NIV-NAVA with a mean SD of 4.7 (1.5) mm versus 3.5 (0.9) mm in NIPPV, p = 0.007. Additionally, the mean (SD) of DTF for the NIV-NAVA group was 81.6 (30) % vs 78.2 (27) % for the NIPPV group [p = 0.71]. Both groups showed relatively high LUS but no significant difference between groups [12.8 (2.6) vs 12.6 (2.6), p = 0.8].
Conclusion: Preterm infants managed with NIV-NAVA showed significantly higher DE compared to those managed on NIPPV. This study raises the hypothesis that NIV-NAVA could potentially improve diaphragmatic function due to its synchronization with patients’ own breathing. Longitudinal studies to assess diaphragmatic function over time are needed.
Trial registry: Clinicaltrials.gov (NCT05079412). Date of registration September 30, 2021.
What is Known: • NIV-NAVA utilizes diaphragmatic electrical activity to provide synchronized breathing support. • Evidence for the effect of NIV-NAVA on diaphragmatic thickness fraction (DTF) and excursion (DE) is limited. | |
What is New: • Ultrasonographic assessment of diaphragmatic function (DTF and DE) is feasible. • In preterm infants, DE was significantly higher in infants supported with NIV-NAVA compared to those supported with NIPPV. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, avoidance of invasive mechanical ventilation (IMV) and promoting of the use of non-invasive ventilation (NIV) in infants born prematurely has been accepted as a standard of care to reduce lung injury and subsequent development of bronchopulmonary dysplasia (BPD) [1]. Although nasal continuous positive airway pressure (nCPAP) is the most frequently used NIV mode for infants born before 32 weeks gestation, NIPPV was found to decrease the incidence of reintubation within 2–7 days of life compared to nCPAP [2]. Furthermore, synchronized NIPPV is considered the most effective NIV in preventing extubation failure in preterm neonates with respiratory distress syndrome [3]. The advantages of NIPPV over nCPAP include the ability to deliver higher mean airway pressure (MAP) and carbon dioxide (CO2) clearance [4, 5].
Recently, neurally adjusted ventilatory assist (NAVA) for invasive and non-invasive ventilation (NIV-NAVA) has emerged as a new respiratory support mode for preterm infants with respiratory insufficiency. Typically, NAVA mode (invasive and non-invasive) uses the electrical activity (Edi) of the diaphragm to trigger, set the amount of pressure, and cycle off the ventilator which in turn reduces asynchrony during NIV [6, 7]. In comparison to NIPPV, several studies have reported that NIV-NAVA is associated with a higher success rate of preventing reintubation [8,9,10], alongside fewer episodes of bradycardia and apnea of prematurity per day [11]. However, data regarding the effect of NIV-NAVA compared to NIPPV on diaphragmatic function and dimensions in preterm infants remains unknown.
Lung ultrasound (LU) has been increasingly used in neonates as a non-invasive and radiation-free imaging modality to assess lung aeration and diaphragm function. Moreover, there is a growing interest among researchers in using ultrasound to monitor the evolution of diaphragmatic contractility and dimensions during IMV, for clinical and research purposes [41].
We acknowledge our study limitations. First, we had a small sample size that could be attributed to interrupted/low recruitment rate due to the COVID-19 pandemic. Second, the study design was based on consecutive recruitment of all eligible patients but lacked randomization. Thirdly, we did not do a serial ultrasonographic assessment to evaluate the changes of diaphragmatic dimensions and functions over time while infants were supported by these two types of NIV. Another limitation is that infants in the NIV-NAVA group were scanned after short duration post transitioning from NIPPV and the risk of “carryover effect” cannot be ruled out completely. Finally, diaphragm ultrasound is operator dependent; therefore, some variations in the measurements are not uncommon. However, our study results have shown high interobserver reliability which validate, to some degree, the study findings.
Conclusion
In infants born at < 30 weeks’ gestation, NIV-NAVA was associated with significantly higher DE compared to NIPPV reflecting improvement in the diaphragmatic functions. There were no significant differences regarding other measurement such as DTexp, DTins, DTF, and LUS. Further studies, with a larger sample size and serial assessment of the diaphragm are needed to draw a firm conclusion.
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Abbreviations
- DE:
-
Diaphragm excursion
- DTexp :
-
Diaphragm thickness at end of expiration
- DTF:
-
Diaphragm thickness fraction
- DTins :
-
Diaphragm thickness at end of inspiration
- ICC:
-
Intraclass correlation coefficient
- IMV:
-
Invasive mechanical ventilation
- LU:
-
Lung ultrasound
- LUS:
-
Lung ultrasound score
- NAVA:
-
Neurally adjusted ventilatory assist
- nCPAP:
-
Nasal continuous positive airway pressure
- NICU:
-
Neonatal intensive care unit
- NIPPV:
-
Nasal intermittent positive pressure ventilation
- NIV:
-
Non-invasive ventilation
- RCT:
-
Randomized control trial
- SD:
-
Standard deviation
References
Stein H, Beck J, Dunn M (2016) Non-invasive ventilation with neurally adjusted ventilatory assist in newborns. Semin Fetal Neonatal Med 21:154–161
Lemyre B, Davis PG, De Paoli AG, Kirpalani H (2017) Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev 2:Cd003212
Ramaswamy VV, More K, Roehr CC, Bandiya P, Nangia S (2020) Efficacy of noninvasive respiratory support modes for primary respiratory support in preterm neonates with respiratory distress syndrome: systematic review and network meta-analysis. Pediatr Pulmonol 55:2940–2963
Mukerji A, Belik J (2015) Neonatal nasal intermittent positive pressure ventilation efficacy and lung pressure transmission. J Perinatol 35:716–719
Latremouille S, Bhuller M, Shalish W, Sant’Anna G (2021) Cardiorespiratory effects of NIV-NAVA, NIPPV, and NCPAP shortly after extubation in extremely preterm infants: A randomized crossover trial. Pediatr Pulmonol 56:3273–3282
Firestone KS, Beck J, Stein H (2016) Neurally adjusted ventilatory assist for noninvasive support in neonates. Clin Perinatol 43:707–724
Treussart C, Decobert F, Tauzin M, Bourgoin L, Danan C, Dassieu G, Carteaux G, Mekontso-Dessap A, Louis B, Durrmeyer X (2022) Patient-ventilator synchrony in extremely premature neonates during non-invasive neurally adjusted ventilatory assist or synchronized intermittent positive airway pressure: a randomized crossover pilot trial. Neonatology 119:386–393
Makker K, Cortez J, Jha K, Shah S, Nandula P, Lowrie D, Smotherman C, Gautam S, Hudak ML (2020) Comparison of extubation success using noninvasive positive pressure ventilation (NIPPV) versus noninvasive neurally adjusted ventilatory assist (NI-NAVA). J Perinatol 40:1202–1210
Yonehara K, Ogawa R, Kamei Y, Oda A, Kokubo M, Hiroma T, Nakamura T (2018) Non-invasive neurally adjusted ventilatory assist versus nasal intermittent positive-pressure ventilation in preterm infants born before 30 weeks’ gestation. Pediatr Int 60:957–961
Shin SH, Shin SH, Kim SH, Song IG, Jung YH, Kim EK, Kim HS (2022) Noninvasive neurally adjusted ventilation in postextubation stabilization of preterm infants: a randomized controlled study. J Pediatr 247:53-59.e51
Tabacaru CR, Moores RR Jr, Khoury J, Rozycki HJ (2019) NAVA-synchronized compared to nonsynchronized noninvasive ventilation for apnea, bradycardia, and desaturation events in VLBW infants. Pediatr Pulmonol 54:1742–1746
Zhao XQ, Tang ZJ, **a B (2021) Clinical application of ultrasound in paediatric diaphragmatic dysfunction. Pediatr Dimens 6:1–6
Kharasch SJ, Dumas H, O’Brien J, Shokoohi H, Al Saud AA, Liteplo A, Schleifer J, Kharasch V (2021) Detecting ventilator-induced diaphragmatic dysfunction using point-of-care ultrasound in children with long-term mechanical ventilation. J Ultrasound Med 40:845–852
Wait JL, Johnson RL (1997) Patterns of shortening and thickening of the human diaphragm. J Appl Physiol 83:1123–1132
Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen JA, Watson JC, Sorenson EJ (2013) Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve 47:884–889
Ferrari G, De Filippi G, Elia F, Panero F, Volpicelli G, Aprà F (2014) Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit Ultrasound J 6:8
Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM (2011) Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 39:2627–2630
Bahgat E, El-Halaby H, Abdelrahman A, Nasef N, Abdel-Hady H (2021) Sonographic evaluation of diaphragmatic thickness and excursion as a predictor for successful extubation in mechanically ventilated preterm infants. Eur J Pediatr 180:899–908
Yeung T, Mohsen N, Ghanem M, Ibrahim J, Shah J, Kajal D, Shah PS, Mohamed A (2022) Diaphragmatic thickness and excursion in preterm infants with bronchopulmonary dysplasia compared with term or near term infants: a prospective observational study. Chest
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
El-Halaby H, Abdel-Hady H, Alsawah G, Abdelrahman A, El-Tahan H (2016) Sonographic evaluation of diaphragmatic excursion and thickness in healthy infants and children. J Ultrasound Med 35:167–175
El-Mogy M, El-Halaby H, Attia G, Abdel-Hady H (2018) Comparative study of the effects of continuous positive airway pressure and nasal high-flow therapy on diaphragmatic dimensions in preterm infants. Am J Perinatol 35:448–454
Grosu HB, Lee YI, Lee J, Eden E, Eikermann M, Rose KM (2012) Diaphragm muscle thinning in patients who are mechanically ventilated. Chest 142:1455–1460
Cohn D, Benditt JO, Eveloff S, McCool FD (1997) Diaphragm thickening during inspiration. J Appl Physiol 83:291–296
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, Brochard LJ, Bolz SS, Rubenfeld GD, Kavanagh BP, Ferguson ND (2015) Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med 41:642–649
Umbrello M, Formenti P, Longhi D, Galimberti A, Piva I, Pezzi A, Mistraletti G, Marini JJ, Iapichino G (2015) Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study. Crit Care 19:161
Mohamed A, Mohsen N, Diambomba Y, Lashin A, Louis D, Elsayed Y, Shah PS (2021) Lung ultrasound for prediction of bronchopulmonary dysplasia in extreme preterm neonates: a prospective diagnostic cohort study. J Pediatr 238:187-192.e182
Brat R, Yousef N, Klifa R, Reynaud S, Shankar Aguilera S, De Luca D (2015) Lung ultrasonography score to evaluate oxygenation and surfactant need in neonates treated with continuous positive airway pressure. JAMA Pediatr 169:e151797
Hayat A, Khan A, Khalil A, Asghar A (2017) Diaphragmatic excursion: does it predict successful weaning from mechanical ventilation? J Coll Physicians Surg Pak 27:743–746
Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A (2017) Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med 43:29–38
Hadda V, Pahuja S, Mittal S, Madan K, Khan MA, Mohan A, Guleria R (2022) Effects of neurally adjusted ventilation assist (NAVA) and conventional modes of mechanical ventilation on diaphragm functions: a randomized controlled trial. Heart Lung 53:36–41
Alam MJ, Roy S, Iktidar MA, Padma FK, Nipun KI, Chowdhury S, Nath RK, Rashid HO (2022) Diaphragm ultrasound as a better predictor of successful extubation from mechanical ventilation than rapid shallow breathing index. Acute Crit Care 37:94–100
Lee BK, Shin SH, Jung YH, Kim E-K, Kim H-S (2019) Comparison of NIV-NAVA and NCPAP in facilitating extubation for very preterm infants. BMC Pediatr 298
Yagui AC, Gonçalves PA, Murakami SH, Santos AZ, Zacharias RSB, Rebello CM (2021) Is noninvasive neurally adjusted ventilatory assistance (NIV-NAVA) an alternative to NCPAP in preventing extubation failure in preterm infants? J Matern Fetal Neonatal Med 34:3756–3760
Soreze Y, Motte E, Dell’Orto V, Yousef N, De Luca D (2018) Use of neurally adjusted ventilator assist in postsurgical hemidiaphragmatic paralysis. Arch Dis Child Fetal Neonatal Ed 103:F86-f87
Gentili A, Masciopinto F, Mondardini MC, Ansaloni S, Reggiani ML, Baroncini S (2013) Neurally adjusted ventilatory assist in weaning of neonates affected by congenital diaphragmatic hernia. J Matern Fetal Neonatal Med 26:598–602
Roosens S, Derriks F, Cools F (2016) Case report: Non-invasive neurally adjusted ventilatory assist in a newborn with unilateral diaphragmatic paralysis. Pediatr Pulmonol 51:E37-e39
Rehan VK, Laipraset J, Wallach M, McCool FD (1999) Effects of CPAP on diaphragm dimensions in the neonate. Pediatr Res 45:317–317
Alonso-Ojembarrena A, Lubián-López SP (2019) Lung ultrasound score as early predictor of bronchopulmonary dysplasia in very low birth weight infants. Pediatr Pulmonol 54:1404–1409
Loi B, Vigo G, Baraldi E, Raimondi F, Carnielli VP, Mosca F, De Luca D (2021) Lung ultrasound to monitor extremely preterm infants and predict bronchopulmonary dysplasia. A multicenter longitudinal cohort study. Am J Respir Crit Care Med 203:1398–1409
Oulego-Erroz I, Alonso-Quintela P, Terroba-Seara S, Jiménez-González A, Rodríguez-Blanco S (2021) Early assessment of lung aeration using an ultrasound score as a biomarker of develo** bronchopulmonary dysplasia: a prospective observational study. J Perinatol 41:62–68
Acknowledgements
We would also like to thank the families, nurses, and respiratory therapists in Mount Sinai Hospital who helped us complete our study.
Guarantor
AM, who takes responsibility for the content of the manuscript, including the data and analysis (Original Research).
Author information
Authors and Affiliations
Contributions
ME and LT has equal contribution to the study design, data collection, and manuscript writing. AM had full access to all of the data and takes responsibility for the content of this manuscript, including study design, data, and data analysis. The study design was conducted by LT, ME, JI, NN, and AM; data collection was performed by JI, ME, and AM. Data analysis was performed by NN and AM. The manuscript was prepared by ME and LT then edited by JI, NN, and AM. All authors of this study approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Local research ethics approval was obtained (Mount Sinai Hospital REB (19–0324-E), Toronto, ON, Canada.
Consent to participate
Written informed consent was obtained from parents or guardians.
Consent for publication
All the authors have seen the final version of the manuscript and gave their full consent for the publication.
Conflicts of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abstract publication/presentation
Portions of this paper were presented at the Pediatric Academic Society (PAS) meeting in Denver, USA, in May 2022 a as poster presentation as well as at the 4th Neonatal Research Day- Toronto, Canada, on April 2022 as an oral presentation.
Rights and permissions
About this article
Cite this article
Elkhouli, M., Tamir-Hostovsky, L., Ibrahim, J. et al. Ultrasonographic assessment of diaphragmatic function in preterm infants on non-invasive neurally adjusted ventilatory assist (NIV-NAVA) compared to nasal intermittent positive-pressure ventilation (NIPPV): a prospective observational study. Eur J Pediatr 182, 731–739 (2023). https://doi.org/10.1007/s00431-022-04738-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04738-8