Abstract
Sclerostin (SOST) is produced by osteocytes and is known as a negative regulator of bone homeostasis. Parathyroid hormone (PTH) regulates calcium, phosphate as well as vitamin D metabolism, and is a strong inhibitor of SOST synthesis in vitro and in vivo. PTH has two methionine amino acids (positions 8 and 18) which can be oxidized. PTH oxidized at Met18 (Met18(ox)-PTH) continues to be bioactive, whereas PTH oxidized at Met8 (Met8(ox)-PTH) or PTH oxidized at Met8 and Met18 (Met8, Met18(di-ox)-PTH) has minor bioactivity. How non-oxidized PTH (n-oxPTH) and oxidized forms of PTH act on sclerostin synthesis is unknown. The effects of n-oxPTH and oxidized forms of PTH on SOST gene expression were evaluated in UMR106 osteoblast-like cells. Moreover, we analyzed the relationship of SOST with n-oxPTH and all forms of oxPTH in 516 stable kidney transplant recipients using an assay system that can distinguish in clinical samples between n-oxPTH and the sum of all oxidized PTH forms (Met8(ox)-PTH, Met18(ox)-PTH, and Met8, Met18(di-ox)-PTH). We found that both n-oxPTH and Met18(ox)-PTH at doses of 1, 3, 20, and 30 nmol/L significantly inhibit SOST gene expression in vitro, whereas Met8(ox)-PTH and Met8, Met18(di-ox)-PTH only have a weak inhibitory effect on SOST gene expression. In the clinical cohort, multivariate linear regression showed that only n-oxPTH, but not intact PTH (iPTH) nor oxPTH, is independently associated with circulating SOST after adjusting for known confounding factors. In conclusion, only bioactive PTH forms such as n-oxPTH and Met18(ox)-PTH, inhibit SOST synthesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parathyroid hormone (PTH) is a key endocrine regulator of calcium and phosphate homeostasis in vivo [9, 40]. PTH exerts its functions by binding to the PTH-1 receptor (PTH1R), which is primarily expressed on osteoblasts in bone and tubular cells in the kidneys [11]. Sclerostin (SOST) is a secreted glycoprotein product of the SOST gene, which is mainly produced by osteocytes [29]. It is known as a bone formation inhibitor [34]. The negative relationship between PTH and SOST has been reported in both preclinical and clinical studies. It was noted that PTH inhibits the transcription of SOST directly [4, 23, 31, 35, 41], and also impacts the expression of SOST protein in both in vivo and in vitro preclinical studies [4, 13, 31, 53]. In clinical studies, researchers found that circulating SOST is inversely associated with PTH in primary hyperparathyroidism (PHPT) [1, 47, 49] and postmenopausal women [12]. Additionally, a consistent correlation between SOST and PTH was also observed in dialysis patients [7, 21, 52, 54]. Taken together with all previous findings, in animal models and humans, we assume that the anabolic properties of PTH may be mediated at least in part by inhibiting SOST production. Although the molecular mechanisms of the negative relationship of PTH with SOST remain unknown, exploring this interaction may significantly improve our understanding of the effects of PTH on bones. In addition, the inverse relationship between circulating SOST and PTH in vivo should be taken into consideration when using SOST- and PTH-related agents in clinical practice.
As early as 1934, PTH was described as potentially loosing its bioactivity after oxidation [43]. However, for decades, n-oxPTH could not be discriminated from oxPTH in clinical samples using classic PTH assays such as second and third generation assays, until Hocher et al. introduced oxPTH columns, allowing n-oxPTH to be measured fairly easily [19]. Subsequently, the role of n-oxPTH in the clinical setting has been increasingly appreciated. Some studies showed that high n-oxPTH, rather than oxPTH concentrations are associated with adverse outcomes in chronic kidney disease (CKD) [51, 56], graft loss in kidney transplant recipients (KTRs) [48], and a high mortality risk in dialysis patients [42]. Circular dichroism (CD) studies of PTH found that oxidized methionine (Met) within PTH leads to conformational changes which might impact the interaction of PTH and PTH1R [58]. In contrast to non-oxidized PTH (n-oxPTH), oxidized PTH (ox-PTH) has a very low binding affinity to PTH1R due to secondary structure alterations, thus, it fails to stimulate the PTH1R to generate the second messenger cyclic adenosine monophosphate (cAMP) [19]. It is widely accepted that ox-PTH and n-oxPTH possess quite different biological properties [20]. Previously, Hocher et al. studied CKD cohorts with different degree [20]. They found that the ratios of oxPTH/n-oxPTH increases as the degree of CKD. The details are as follows: 3.24-fold in healthy controls (n = 89), 7.75-fold CKD at stage 2–4 (n = 620); 8.45-fold in end-stage renal disease patients on hemodialysis (n = 342); 8.47-fold in kidney transplant recipients (n = 602). This study is a big step for understanding the role of oxPTH in CKD patients. Taken together, the proportion of oxPTH increases from healthy controls to end-stage-kidney disease, thus uremia seems to influence the degree of PTH oxidation [20]. In addition, Hasan et al. recently reviewed many in vitro studies, which showed that oxPTH possesses reduced biological activity in many aspects compared to n-oxPTH, such as activating alkaline phosphatase, as well as relaxing guinea-pig tracheas, constricting blood vessels, stimulating cardiac action, and influencing fibroblast growth factor (FGF23) synthesis in vitro [18].
PTH (1–84) contains two Met amino acids at positions 8 (Met8-PTH) and 18 (Met18-PTH) that are prone to oxidation in vivo [19, 20]. It has been reported that Met8-PTH is less likely oxidized due to its location in a hydrophobic pocket [8] and a substantial change of secondary structure that is needed for the conversion to its oxidized form [58]. Contrastingly, Met18-PTH [8] is more likely to be oxidized and oxidation causes a relatively small conformation change [58]. Moreover, it is known that Met18(ox)-PTH has residual biological activity when tested separately [8, 45]. In addition, oxidation of both Met8 and 18 had the biggest conformation changes when compared with individual oxidations [58]. Accordingly, the bioactive sequence of different ox-PTH forms are as follows: Met18(ox)PTH > Met8(ox)PTH > Met8, Met18 (di-ox) PTH [58].
In a prior study we observed that only n-oxPTH, but not iPTH or oxPTH, statistically correlated with FGF23 in CKD patients [56]. Furthermore, this study found in in vitro experiments in UMR106 cells that different forms of oxPTH stimulate fibroblast growth factor (FGF23) with varying intensities of stimulation [56]. However, this study did not explore the association between SOST and n-oxPTH [56]. Considering the significant clinical importance of the relationship between PTH and SOST based on previous studies, we aimed to further investigate the effects of different forms and concentrations of PTH on the expression of SOST in both in vitro experiments in UMR106 rat osteoblast-like cells and in vivo studies in a cohort of kidney transplant recipients (KTRs).
Materials and methods
Cell cultures
UMR106 rat osteoblast-like cells (CRL-166; ATCC, USA) were cultured under standard culture conditions [2]. The medium consisted of Dulbecco’s Modified Eagle Medium (DMEM) with 4,5 g/L glucose (L-glutamine) (Invitrogen, USA), supplemented with 10% fetal calf serum (FCS) (Life Technologies, Germany), penicillin (100u/ml) and streptomycin (100ug/ml) (Sigma-Aldrich, Germany) at 5% CO2 and 37 °C. Cells were seeded in six-well plates (0.6 × 106 per cell). UMR106 cells were grown for 24 h and then removed from the previous medium before adding an equal volume of fresh culture medium into each well. The cells were treated with or without the different types of PTH 1–34 derivatives, as indicated, for an additional 24 h. Thereafter, the supernatant and cells were harvested for subsequent experiments.
In the study, we used the four types of PTH peptides to activate UMR106 cells, namely n-oxPTH, Met8(ox)-PTH, Met18(ox)-PTH, and Met8, Met18(di-ox)-PTH at 1, 3, 20, 30 nmol/L. In the control group no PTH peptide stimulation was used. All PTH peptides were purchased from JPT Peptide Technologies GmbH, as used by Zeng et al. recently [56]. Each experiment was repeated six times.
Quantitative real-time polymerase chain reaction
We isolated total RNA from UMR106 cells using TRIzol reagent (Life Technologies, Germany). Then, 1.0 μg thereof was used for cDNA synthesis using a high-capacity cDNA reverse transcription kit (4368814, Fisher Scientific GmbH, Schwerte, Germany). Subsequently, 3.5 uL cDNA was added to quantitative real-time PCR (qRT-PCR). Next, we applied the TaqMan assays method to quantify relative transcript levels. The qRT-PCR reaction mix contained 0.5 uL cDNA, 10 uL TaqMan Advanced Master Mix (4444557, Fisher Scientific GmbH, Schwerte, Germany), 1 uL rat TaqMan assays, and 8.5 uL nuclease-free H2O per well according to the manufacturer’s instructions (50 °C for 2 min, 95 °C for 2 min, followed by 40 cycles of 95 °C for 1 s, 60 °C for 20 s). As for negative controls, nuclease-free water was used. The relevant rat TaqMan assays were actin (Actb, 4453320, Rn00667869_m1) and SOST (4453320, Rn00577971_m1), both from Fisher Scientific GmbH, Schwerte, Germany. The whole qRT-PCR procedure was performed using the ABI Step-One Plus Real-Time PCR Systems (Applied Biosystems, USA).
Population
We collected clinical data and analyzed plasma samples of a kidney transplant patient cohort from the Transplant Clinic of Charité-Mitte, Berlin, Germany. This study was approved by the Ethics Commission of Charité University, Berlin, Germany.
The inclusion criteria included: (1) kidney transplant recipients, (2) recipients’ age ≧18 years, (3) stable and functional graft. The exclusion criteria were as follows: (1) graft loss, (2) acute infection, (3) acute rejection, (4) acute myocardial infarction, (5) malignancy, (6) pulmonary edema, (7) heart failure at baseline, (8) patients with incomplete data for variables such as SOST, n-oxPTH, ox-PTH, and iPTH. In total, 516 stable KTRs met these criteria and were included in the study. All participants were informed and signed the informed consent. In our study, clinical and laboratory parameters included the donor’s age, the recipients’ gender and age, time after transplantation, time on dialysis, cold ischemia time, HLA mismatches, estimated glomerular filtration rate (eGFR), underlying renal disease, fasting blood glucose as well as plasma SOST, osteoprotegerin (OPG), ox-PTH, n-oxPTH, iPTH, calcium, phosphate, creatinine, albumin, calcitriol (1,25(OH)2D), alkaline phosphatase, and total plasma cholesterol.
Laboratory methods
At study entry, blood samples were collected and stored at -20 ℃ until the following measurements were made. Baseline laboratory measurements, such as fasting blood glucose, plasma calcium, phosphate, creatinine, albumin, 1,25(OH)2D, alkaline phosphatase, and total cholesterol were measured by standardized laboratory methods. The eGFR was calculated based on the CKD-EPI equation.
N-oxPTH was measured using the intact-PTH electrochemiluminescence immunoassay (ECLIA; Roche PTH, Intact [iPTH]), which used two types of monoclonal antibodies. One is a biotinylated monoclonal antibody, which can react with amino acids 26–32, and the other is a capture ruthenium-complexed monoclonal antibody targeting amino acids 55–64. The assay was performed on a Roche Modular E 170®. Therein, any oxidized forms of PTH (1–84) at positions of Met8 and/or Met18 were removed through a specific chromatography column where anti-human-oxPTH monoclonal antibodies were contained. Moreover, iPTH was analyzed directly by classical third generation iPTH sandwich assays (in short iPTH assay), which, as a limitation, cannot differentiate n-oxPTH from ox-PTH. Details were described in our previous studies [19, 42].
SOST concentration was measured using a commercial enzyme-linked immunosorbent assay (ELISA) (BI-20492, Biomedica Medizinprodukte GmbH &Co KG, Vienna, Austria), and OPG concentration was also measured using a commercial ELISA (BI-20403, Biomedica Medizinprodukte GmbH &Co KG, Vienna, Austria). Plasma SOST and OPG samples were measured according to the manufacturer’s instructions as described in the studies of Zeng et al. [56, 57]. Briefly, in the first step, 150 uL assay buffer was pipetted into wells, which were pre-coated with goat polyclonal anti-SOST/OPG antibodies. Then, 20 uL/well of standards, samples or controls were added in duplicate into the plates. Next, 50 uL/well of biotinylated anti-SOST/OPG antibodies were added into the plates. The plates were incubated at room temperature (RT) (18–24 °C) for 4 h for biotinylated anti-OPG antibody, but overnight in the dark for biotinylated anti-SOST antibody. After washing, a conjugate (200 uL/well) was pipetted into all wells and the plates were incubated for 1 h at room temperature (RT), then, washed as before. After a final washing, 200 uL/well of substrate solution were added into the plates, which were then incubated for 30 min at RT in the dark. The reaction was stopped by adding a stop solution (50 uL/well), and the absorbance was read at 450 nm with a correction wavelength of 630 nm using a microplate reader (Bio-Rad 680, USA).
Statistics
The data on the relative gene expression of SOST in cultured UMR106 cells treated with the four types of PTH peptides was non-normally distributed, therefore, the Kruskal–Wallis test followed by Dunn’s post-hoc test was performed. In the clinical cohort, quantitative variables were given as medians (interquartile range, IQR) due to non-normal distribution, and categorical variables were presented as n (%). The Spearman correlation analysis was used to evaluate the correlations between plasma SOST and n-oxPTH, oxPTH, and iPTH, along with other clinical and blood biochemical parameters. Then, we selected clinical variables with p < 0.05, as well as iPTH and oxPTH, into a multivariate linear regression model (Method: stepwise regression analysis), where we further assessed the relationship between plasma SOST and PTH forms. All data were analyzed using SPSS software version 26.0 (IBM, New York, USA) and GraphPad Prism 9.0 (GraphPad Software, Inc. La Jolla. California, USA). Significance was defined at a two-sided p-value < 0.05.
Results
In vitro studies
To investigate how n-oxPTH, Met18(ox)-PTH, Met8-Met18(di-ox)-PTH, and Met8(ox)-PTH influence SOST gene expression, we conducted an in vitro experiment in UMR106 osteoblast-like cells.
All investigated concentrations of n-oxPTH suppressed the expression of SOST significantly (P < 0.001). A dose-dependence was not detectable with a clear suppression of SOST expression down to a basal level already at the lowest concentration of 1 nmol/L. Met18(ox)-PTH inhibited SOST expression dose-dependently at all concentrations (1, 3, 20, 30 nmol/L) (P < 0.001), but the extent of this suppression was less marked than with n-oxPTH compared. Met8, Met18(di-ox)-PTH also showed a dose-dependent but comparatively much weaker inhibition of SOST expression at all concentrations. Met8(ox)-PTH, on the other hand, inhibited SOST expression even weaker and only at concentrations of 20 and 30 nmol/L. In addition, the inhibition of SOST expression was different in the distinct concentrations of Met8(ox)-PTH in the culture medium with concentrations of 1 and 30 nmol/L (P < 0.05). (Fig. 1 a–d).
The effects of n-oxPTH and various forms of oxPTH on SOST gene expression in UMR106 rat osteoblast-like cells (a–d). We cultured the cells for the first 24 h, then, treated them with or without PTH 1–34 derivatives for another 24 h at 1, 3, 20, and 30 nmol/L, respectively. The experiment was repeated six times and the levels of SOST expression were measured by qRT-PCR. a and b Both n-oxPTH and Met18(ox)-PTH peptides, at all dosages caused a significant decrease in SOST gene expression when compared with negative controls (P < 0.001), however n-ox PTH had a maximum inhibitory effect already at 1 nmol/L; an extent of inhibition, that was not reached even with a dose of 30 nmol/L Met18(ox)-PTH peptides. c A similar trend was also observed in the Met18(di-ox)-PTH peptides, despite a relatively slight inhibition in comparison to negative controls (P < 0.05). d However, the Met8(ox)-PTH peptides inhibited the SOST mRNA synthesis even to a lesser extent and only at 20 and 30 nmol/L (P < 0.05), but not at 1 and 3 nmol/L, when compared with negative controls. The x-axis shows the different concentrations. The y-axis represents the relative SOST gene expression. Data was analyzed using the Kruskal–Wallis test followed by Dunn’s post-hoc test. * P < 0.05, ** P < 0.01, *** P < 0.001 vs. control group. # P < 0.05, 1 nmol/L vs. 3 nmol/L Met8(ox)-PTH peptides. Abbreviations: iPTH, intact PTH; n-oxPTH, non-oxidized PTH; oxPTH, oxidized PTH; PTH, parathyroid hormone; SOST, sclerostin
Clinical study
A total of 516 stable KTRs, with 314 (61%) males and 202 (39%) females, were included in this study. The median age of the cohort was 54.7 years (IQR 45.6–67.2 y). Demographics and characteristics of the study population are presented in Table 1. At study entry, the median of plasma SOST, iPTH, ox-PTH, and n-oxPTH levels were 47.0 (35.7–61.9) pmol/L, 77.3 (49.1–128.1) pg/mL, 68.7 (42.1–116.1) pg/mL, and 8.6 (5.4–12.9) pg/mL, respectively.
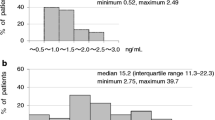
The distribution of iPTH, oxPTH, n-oxPTH, and SOST concentrations is shown in Fig. 2. The distribution of actual iPTH, oxPTH, and n-oxPTH concentrations in the KTR cohort were not normally distributed, but the distribution of SOST concentration was nearly normally distributed. Thus, we analysed the relationship of plasma SOST to other relevant clinical and biochemical variables in adult KTRs using the Spearman correlation analysis, as described in Table 2. After primary correlation analysis, only n-oxPTH (n = 516, rs = −0.095, P = 0.030), but not iPTH (n = 516, rs = −0.066, P = 0.136) nor oxPTH (n = 516, rs = −0.056, P = 0.202), were associated with plasma SOST (P < 0.05). Moreover, clinical variables including the recipients’ gender (n = 516, rs = −0.152, P < 0.001), age at study entry (n = 515, rs = 0.258, P < 0.001), plasma phosphate (n = 508, rs = 0.160, P < 0.001), plasma creatinine (n = 514, rs = 0.258, P < 0.001), eGFR (n = 498, rs = −0.250, P < 0.001) and plasma OPG (n = 516, rs = 0.235, P < 0.001) were correlated with plasma SOST.
Histogram showing the frequency distribution of plasma iPTH (a), oxPTH (b), n-oxPTH (c), and Sclerostin (d) in 516 stable kidney transplant recipients. The actual concentrations of iPTH, oxPTH, and n-oxPTH in the study population are not normally distributed, except for SOST concentration, which is similar to a normal distribution. Abbreviations: iPTH, intact PTH; n-oxPTH, non-oxidized PTH; oxPTH, oxidized PTH; PTH, parathyroid hormone; SOST, sclerostin
Due to the moderately skewed distributions of actual SOST and n-oxPTH concentrations in the study population, we calculated ln-SOST and ln-n-oxPTH to achieve a similar normal distribution (ln-SOST Kolmogorov–Smirnov Test: D = 0.040, P = 0.048; ln-n-oxPTH Kolmogorov–Smirnov Test: D = 0.038, P = 0.075, respectively). Then, we further analyzed the correlation between n-oxPTH and SOST using the Pearson correlation analysis. A significant negative correlation was observed between n-oxPTH and SOST concentrations (r = −0.121, P < 0.05) (Fig. 3).
Scatterplot showing the correlation between SOST and n-oxPTH plasma concentrations in kidney transplant recipients. As actual plasma SOST and n-oxPTH concentrations were moderately skewed in the study, we calculated ln-SOST and ln-n-oxPTH. After data transformation, both ln-SOST and ln-n-oxPTH were close to being normally distributed. We used Pearson correlation analysis to assess the associations between ln-SOST and ln-n-oxPTH. Our findings showed that ln-SOST was significantly negatively associated with ln-n-oxPTH (P < 0.05). Abbreviations: n-oxPTH, non-oxidized PTH; PTH, parathyroid hormone; SOST, sclerostin
To further investigate the correlation of plasma SOST with n-oxPTH, we carried out a multivariate linear regression analysis using the stepwise method (Table 3). Plasma n-oxPTH, oxPTH, iPTH, recipients’ gender and age at study entry, plasma phosphate, plasma creatinine, eGFR, plasma OPG, and plasma SOST were included in the model. Our findings showed that plasma n-oxPTH (95%CI: −0.829- −0.355; P < 0.001), plasma creatinine (95%CI: 6.392–13.065; P < 0.001), recipients’ gender (95%CI: −9.657- −0.209; P = 0.040) and age at study entry (95%CI: 0.228–0.508; P < 0.001) were independently associated with the levels of circulating SOST.
Discussion
This study demonstrates that non-oxidized and oxidized forms of PTH have different biological effects on SOST expression in vitro. N-oxPTH and Met18(ox)-inhibit SOST mRNA expression in UMR106 cells, whereas Met8(ox)-PTH and Met8, Met18(di-ox)-PTH don’t do this. In adult kidney transplant recipients, only n-oxPTH, but not oxPTH (a measure of all oxidized forms of PTH) nor iPTH (a measure of all PTH forms), is independently inversely associated with SOST concentrations after adjusting for known confounding factors.
In 2005, the hypothesis that PTH directly downregulates SOST expression was initially proven through in vivo and in vitro experiments [23]. A reduction of SOST expression in the femur bone was also observed in vivo [23]. Subsequently, further independent studies obtained consistent results that the addition of PTH impeded SOST expression in vitro and in vivo [4, 35, 41]. Our study is in line with the previous studies, but demonstrate for the first time that only bioactive forms of PTH (n-oxPTH as well as Met18(ox)-PTH) but not Met8(ox)-PTH and Met8, Met18(di-ox)-PTH do suppress SOST gene expression. Our finding that oxidation of PTH matters with regard to its biological activity is supported by the following points:
-
(1)
Compared to n-oxPTH, oxPTH (the authors tested a mixture of oxidized PTH forms) had a significantly lower binding affinity to PTHR, resulting in a lower biological activity of oxPTH, which presented itself as a reduction in regulation of calcium and phosphate metabolisms in vivo [20].
-
(2)
Previous studies have proven that methionine amino acids at position 18 are more likely to be oxidized in vivo than those at position 8, see [8]. Methionine residue 8 is in a hydrophobic pocket, which leads to a more difficult oxidation [45]. Only oxidized forms of PTH at position 18 still have residual biological activity, shown when the activity of oxidized forms of PTH are separately tested [14, 45]. This is because PTH with an oxidized methionine residue at position 18 has a more similar structure to n-oxPTH, which has a full biological function [45]. This evidence supports our findings that Met18(ox)-PTH has the by far strongest effects on inhibiting SOST expression among the oxidized PTH forms.
Although the mechanisms of PTH downregulating SOST are not completely understood, possible underlying mechanisms are as follows; Firstly, PTH probably inhibits SOST expression through inducing proteasomal degradation of Runx2 [5] which is a SOST-dependent gene and can upregulate sclerostin production [39]. Secondly, PTH downregulates osteocyte-specific SOST expression by inhibiting the activity and/or expression of MEF2 in osteocytes [26, 30], which is important for the transcriptional activation of the SOST bone enhancer [10, 25, 30]. Expression of MEF2 and SOST are co-localized in osteoblasts, and the expression of three types of MEF2 genes including MEF2A, MEF2C, and MEF2D has been proven to be necessary for endogenous SOST expression in UMR-106 cells [30]. Lastly, many in vitro studies have proven that PTH-induced inhibition of SOST mRNA and SOST protein levels is direct and primarily mediated by the activation of the cAMP/PKA signaling pathway downstream of PTH1R [4, 23, 26].
In the clinical cohort study, only n-oxPTH in adult KTRs, but not iPTH nor oxPTH, is independently inversely associated with SOST after multivariate linear regression analysis. The clinical data in KTRs are in good agreement with a recent study showing that plasma SOST levels are negatively correlated with PTH concentrations after, (bioactive) PTH treatment in postmenopausal women [12, 49]. Similarly, the negative association can be seen in patients with primary hyperparathyroidism [1, 31, 47]. It might be assumed – but still needs to be proven—that the parathyroid gland in patients with hyperparathyroidism mainly secretes bioactive forms of PTH, since hypercalcemia, a biological consume of increase bioactive PTH, is often seen in this patient population. In CKD patients on dialysis, an inverse relationship between SOST and PTH was also reported. However, these studies did not investigate whether this association was independent of confounding factors [7, 21, 52, 54]. In our clinical study we likewise saw an inverse relationship between iPTH and n-oxPTH on the one hand and SOST on the other hand. However, only n-oxPTH has a significant inverse correlation with SOST after adjusting confounding factors, although the R2 value in the Fig. 3 is low. We considered that PTH peptides are only one of many factors influencing SOST in kidney transplant patients. Additionally, it is feasible that SOST concentrations in kidney transplant recipients might be influenced by glucocorticoids [3, 6, 15, 24, 28, 32, 38, 46, 50], but only less than 10% of patients in our study received corticosteroids in an actually as low as possible dose after renal transplant. The patients in this cohort received renal transplantation a very long time ago. The policy in our center is to withdraw steroids after 1 year of kidney transplants when patients are stable because of the severe side effects of steroids. Thus, steroids play a very limited role in our study population.
Compared with previous studies, our study separately tested oxidized and non-oxidized forms of PTH in vitro and analyzed their different associations with SOST in KTRs. Our results emphasized the importance of separately measuring n-oxPTH, as a bioactive form of PTH, in the clinical setting. In this study, circulating oxPTH concentrations are much higher than that of n-oxPTH (68.7 (42.1–116.1) pg/mL vs. 8.6 (5.4–12.9) pg/mL, respectively), suggesting that the majority of PTH is oxidized in vivo. Moreover, previous studies have documented that Met18(ox)-PTH is prone to be oxidized in the organisms compared with Met8(ox)-PTH [8]. Thus, we assume that blood Met18(ox)-PTH levels are higher than that of Met8(ox)-PTH under conditions of oxidative stress as it is seen in dialysis patients, which is consistent with the hypothesis of Ursem et al. [45]. Met18(ox)-PTH had a smaller impact on conformation change than Met8(ox)-PTH did [58], resulting in the residual biological activity of Met18(ox)-PTH [44, 45]. These findings support also our in vitro finding that Met18(ox)-PTH peptide is still able to downregulate SOST generation.
In contrast to dialysis patients, in our kidney transplant population study, we did not saw a significant association of SOST with either ox-PTH or iPTH, suggesting that in this population Met8(ox)-PTH and Met8, Met18(di-ox)-PTH are the predominant forms of oxPTH in vivo and weaken this relationship. Met18(ox)-PTH with preserved bioactivity seems to play a minor role. This hypothesis, however, can only be proven with clinical assay systems that can differentiate the various oxidized forms of PTH. The clinical assay system that we used in our study is not able to do this, it just measures the sum of all oxidized forms of PTH.
It has been reported that SOST is a risk factor for abdominal aortic calcification [17] and coronary artery calcification [27]. In patients on dialysis, many studies found a relationship between SOST with cardiovascular mortality [16, 22] and all-cause mortality [16]. A possible explanation is that SOST is an inhibitor of the Wnt signaling pathway, which is related to vascular calcification and the development of cardiovascular events [37]. In addition, our prior study confirmed that SOST is independently associated with all-cause mortality in transplanted patients [57]. Over half of the KTRs died from cardiovascular event [33, 55]. These study findings indicate that controlling SOST levels in a proper range is essential in CKD patients and KTRs. Some anti-sclerostin antibodies, such as romosozumab and blosozumab, are being tested in clinical trials for the treatment of postmenopausal osteoporosis via neutralizing SOST, and the relevant trial outcomes are promising [36]. We hypothesize that a bioactive PTH-associated agent may be a promising approach to regulating SOST in kidney-related diseases to reduce the risk of cardiovascular diseases or relevant mortality. The interaction between SOST and PTH in vivo, especially n-oxPTH, should be taken into consideration when using either PTH or SOST-relevant drugs in CKD populations.
Several limitations should be considered in this study when interpreting its findings. To begin with, we could not separate various forms of oxPTH, such as Met18(ox)-PTH, Met8(ox)-PTH, and Met8, Met18(di-ox)-PTH, in the clinical study due to the restrictions of the current measuring technique. Consistent with previous findings [44, 45], our experimental data also confirmed that Met18(ox)-PTH had the biological activity in vitro. However, current techniques cannot separately measure circulating Met18(ox)-PTH, Met8(ox)-PTH, and Met8, Met18(di-ox)-PTH levels in KTRs, therefore, whether the bioactive Met18(ox)-PTH is also associated with SOST or not in vivo continues to be unclear. Secondly, we observed various effects of n-oxPTH, Met18(ox)-PTH, Met8(ox)-PTH, and Met8, Met18(di-ox)-PTH peptides on SOST mRNA expression in our in vitro experiment. However, we did not assess the effects of different PTH peptides on the SOST protein expression levels. Thus, a further study examining the effects of various forms of PTH on SOST protein levels would be recommended. Lastly, this study is from a single center and the association between n-oxPTH and SOST concentrations was analyzed only in a KTR cohort. Therefore, the findings of this study need to be verified in multiple centers and other kidney diseases in the future.
To conclude, bioactive PTH, such as n-oxPTH and Met18(ox)-PTH, markedly inhibits SOST gene expression in vitro. In the cohort study, we demonstrate an independent association between circulating n-oxPTH, but not iPTH and oxPTH, and SOST, which is consistent with our in vitro results. Given the fact that the majority of PTH in vivo is oxidized, which lacks partial or entire bioactivity, such as the corresponding Met18(ox)-PTH or Met18(ox)-PTH, thus, assay systems that can measure all bioactive forms of PTH separately would be beneficial for clinical use to make proper clinical decisions.
Data availability
The data that support the findings of this study are available on request from the corresponding author (B.H.).
Abbreviations
- cAMP:
-
Cyclic adenosine monophosphate
- CKD:
-
Chronic kidney disease
- DMEM:
-
Dulbecco’s modified eagle medium
- eGFR:
-
Estimated glomerular filtration rate
- HLA:
-
Human leukocyte antigen
- hPTH:
-
Human PTH
- iPTH:
-
Intact PTH
- KTR(s):
-
Kidney transplant recipient(s)
- Met:
-
Methionine
- Met8(ox)-PTH:
-
PTH oxidized at Met8
- Met18(ox)-PTH:
-
PTH oxidized at Met18;
- Met8, Met18(di-ox)-PTH:
-
PTH oxidized at Met8 and Met18
- MEF2:
-
Myocyte enhancer factor 2
- n-oxPTH:
-
Non-oxidized PTH
- ox-PTH:
-
Oxidized PTH
- OPG:
-
Osteoprotegerin
- PTH:
-
Parathyroid hormone
- SOST:
-
Sclerostin
References
Ardawi MS, Al-Sibiany AM, Bakhsh TM et al (2012) Decreased serum sclerostin levels in patients with primary hyperparathyroidism: a cross-sectional and a longitudinal study. Osteoporos Int 23(6):1789–1797. https://doi.org/10.1007/s00198-011-1806-8
Bär L, Hase P, Föller M (2019) PKC regulates the production of fibroblast growth factor 23 (FGF23). PLoS One 14(2019):e0211309. https://doi.org/10.1371/journal.pone.0211309
Belaya ZE, Rozhinskaya LY, Melnichenko GA et al (2013) Serum extracellular secreted antagonists of the canonical Wnt/β-catenin signaling pathway in patients with Cushing’s syndrome. Osteoporos Int 24(8):2191–9. https://doi.org/10.1007/s00198-013-2268-y
Bellido T, Ali AA, Gubrij I et al (2005) Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: a novel mechanism for hormonal control of osteoblastogenesis. Endocrinology 146(11):4577–4583. https://doi.org/10.1210/en.2005-0239
Bellido T, Ali AA, Plotkin LI et al (2003) Proteasomal degradation of Runx2 shortens parathyroid hormone-induced anti-apoptotic signaling in osteoblasts. A putative explanation for why intermittent administration is needed for bone anabolism. J Biol Chem 278(50):50259–50272. https://doi.org/10.1074/jbc.M307444200
BrabnikovaMaresova K, Pavelka K, Stepan JJ et al (2013) Acute effects of glucocorticoids on serum markers of osteoclasts, osteoblasts, and osteocytes. Calcif Tissue Int 92(4):354–61. https://doi.org/10.1007/s00223-012-9684-4
Cejka D, Herberth J, Branscum AJ et al (2011) Sclerostin and Dickkopf-1 in renal osteodystrophy. Clin J Am Soc Nephrol 6(4):877–882. https://doi.org/10.2215/CJN.06550810
Chu JW, Yin J, Wang DI et al (2004) A structural and mechanistic study of the oxidation of methionine residues in hPTH(1–34) via experiments and simulations. Biochemistry 43(44):14139–14148. https://doi.org/10.1021/bi049151v
Civitelli R, Ziambaras K (2011) Calcium and phosphate homeostasis: concerted interplay of new regulators. J Endocrinol Invest 34(7 Suppl):3–7. https://doi.org/10.1007/BF03346687
Collette NM, Genetos DC, Economides AN et al (2012) Targeted deletion of Sost distal enhancer increases bone formation and bone mass. Proc Natl Acad Sci U S A 109(35):14092–14097. https://doi.org/10.1073/pnas.1207188109
Costa AG, Bilezikian JP (2012) Sclerostin: therapeutic horizons based upon its actions. Curr Osteoporos Rep 10(1):64–72. https://doi.org/10.1007/s11914-011-0089-5
Datta NS, Abou-Samra AB (2009) PTH and PTHrP signaling in osteoblasts. Cell Signal 21(8):1245–1254. https://doi.org/10.1016/j.cellsig.2009.02.012
Drake MT, Srinivasan B, Mödder UI et al (2010) Effects of parathyroid hormone treatment on circulating sclerostin levels in postmenopausal women. J Clin Endocrinol Metab 95(11):5056–5062. https://doi.org/10.1210/jc.2010-0720
Dutra EH, O’Brien MH, Gutierrez T et al (2017) PTH [1–34]-induced alterations predispose the mandibular condylar cartilage to mineralization. Orthod Craniofac Res 20 Suppl 1:162–166. https://doi.org/10.1111/ocr.12157
Frelinger AL 3rd, Zull JE (1984) Oxidized forms of parathyroid hormone with biological activity. Separation and characterization of hormone forms oxidized at methionine 8 and methionine 18. J Biol Chem 259(9):5507–5513. https://doi.org/10.1016/S0021-9258(18)91041-0
Gifre L, Ruiz-Gaspà S, Monegal A et al (2013) Effect of glucocorticoid treatment on Wnt signalling antagonists (sclerostin and Dkk-1) and their relationship with bone turnover. Bone 57(1):272–6. https://doi.org/10.1016/j.bone.2013.08.016
Gonçalves FL, Elias RM, dos Reis LM et al (2014) Serum sclerostin is an independent predictor of mortality in hemodialysis patients. BMC Nephrol 15:190. https://doi.org/10.1186/1471-2369-15-190
Hampson G, Edwards S, Conroy S et al (2013) The relationship between inhibitors of the Wnt signalling pathway (Dickkopf-1(DKK1) and sclerostin), bone mineral density, vascular calcification and arterial stiffness in post-menopausal women. Bone 56(1):42–47. https://doi.org/10.1016/j.bone.2013.05.010
Hasan AA, Hocher CF, Kleuser B et al (2022) Biological activity of different forms of oxidized parathyroid hormone. Int J Mol Sci 23(20):12228. https://doi.org/10.3390/ijms232012228
Hocher B, Armbruster FP, Stoeva S et al (2012) Measuring parathyroid hormone (PTH) in patients with oxidative stress–do we need a fourth generation parathyroid hormone assay? PLoS ONE 7(7):e40242. https://doi.org/10.1371/journal.pone.0040242
Hocher B, Oberthür D, Slowinski T et al (2013) Modeling of oxidized PTH (oxPTH) and non-oxidized PTH (n-oxPTH) receptor binding and relationship of oxidized to non-oxidized PTH in children with chronic renal failure, adult patients on hemodialysis and kidney transplant recipients. Kidney Blood Press Res 37(4–5):240–251. https://doi.org/10.1159/000350149
Ishimura E, Okuno S, Ichii M et al (2014) Relationship between serum sclerostin, bone metabolism markers, and bone mineral density in maintenance hemodialysis patients. J Clin Endocrinol Metab 99(11):4315–4320. https://doi.org/10.1210/jc.2014-2372
Kalousová M, Dusilová-Sulková S, Kuběna AA et al (2019) Sclerostin levels predict cardiovascular mortality in long-term hemodialysis patients: A prospective observational cohort study. Physiol Res 68(4):547–558. https://doi.org/10.33549/physiolres.934034
Keller H, Kneissel M (2005) SOST is a target gene for PTH in bone. Bone 37(2):148–158. https://doi.org/10.1016/j.bone.2005.03.018
Klein GL, Herndon DN, Le PT et al (2015) The effect of burn on serum concentrations of sclerostin and FGF23. Burns 41(7):1532–5. https://doi.org/10.1016/j.burns.2015.04.001
Kramer I, Baertschi S, Halleux C et al (2012) Mef2c deletion in osteocytes results in increased bone mass. J Bone Miner Res 27(2):360–373. https://doi.org/10.1002/jbmr.1492
Kramer I, Keller H, Leupin O et al (2010) Does osteocytic SOST suppression mediate PTH bone anabolism? Trends Endocrinol Metab 21 (4):237–244. https://doi.org/10.1016/j.tem.2009.12.002.
Kuipers AL, Miljkovic I, Carr JJ et al (2015) Association of circulating sclerostin with vascular calcification in Afro-Caribbean men. Atherosclerosis 239(1):218–223. https://doi.org/10.1016/j.atherosclerosis.2015.01.010
La Corte R, Trotta F, Adami S (2010) Glucocorticoid receptors and bone. Curr Pharm Des 16(32):3586–92. https://doi.org/10.2174/138161210793797924
Leupin O, Kramer I, Collette NM et al (2007) Control of the SOST bone enhancer by PTH using MEF2 transcription factors. J Bone Miner Res 22(12):1957–1967. https://doi.org/10.1359/jbmr.070804
Lu YP, Zeng S, Chu C et al (2020) Non-oxidized PTH (n-oxPTH) is associated with graft loss in kidney transplant recipients. Clin Chim Acta 508:92–97. https://doi.org/10.1016/j.cca.2020.05.022
Mirza FS, Padhi ID, Raisz LG et al (2010) Serum sclerostin levels negatively correlate with parathyroid hormone levels and free estrogen index in postmenopausal women. J Clin Endocrinol Metab 95(4):1991–1997. https://doi.org/10.1210/jc.2009-2283
Nagata Y, Imanishi Y, Tateishi T et al (2022) Parathyroid Hormone Regulates Circulating Levels of Sclerostin and FGF23 in a Primary Hyperparathyroidism Model. J Endocr Soc 6(4):bvac027. https://doi.org/10.1210/jendso/bvac027
Ohnaka K, Tanabe M, Kawate H et al (2005) Glucocorticoid suppresses the canonical Wnt signal in cultured human osteoblasts. Biochem Biophys Res Commun 329(1):177–81. https://doi.org/10.1016/j.bbrc.2005.01.117
Ojo AO (2006) Cardiovascular complications after renal transplantation and their prevention. Transplantation 82(5):603–611. https://doi.org/10.1097/01.tp.0000235527.81917.fe
Poole KE, van Bezooijen RL, Loveridge N et al (2005) Sclerostin is a delayed secreted product of osteocytes that inhibits bone formation. FASEB J 19(13):1842–1844. https://doi.org/10.1096/fj.05-4221fje
Prideaux M, Wright CS, Noonan ML et al (2021) Generation of two multipotent mesenchymal progenitor cell lines capable of osteogenic, mature osteocyte, adipogenic, and chondrogenic differentiation. Sci Rep 11(1):22593. https://doi.org/10.1038/s41598-021-02060-1
Rauner M, Taipaleenmäki H, Tsourdi E et al (2021) Osteoporosis treatment with anti-sclerostin antibodies-mechanisms of action and clinical application. J Clin Med 10(4):787. https://doi.org/10.3390/jcm10040787
Ress C, Paulweber M, Goebel G et al (2018) Circulating Wnt inhibitory factor 1 levels are associated with development of cardiovascular disease. Atherosclerosis 273:1–7. https://doi.org/10.1016/j.atherosclerosis.2018.03.045
Rossini M, Gatti D, Adami S (2013) Involvement of WNT/β-catenin signaling in the treatment of osteoporosis. Calcif Tissue Int 93(2):121–32. https://doi.org/10.1007/s00223-013-9749-z
Sevetson B, Taylor S, Pan Y (2004) Cbfa1/RUNX2 directs specific expression of the sclerosteosis gene (SOST). J Biol Chem 279(14):13849–13858. https://doi.org/10.1074/jbc.M306249200
Silva BC, Bilezikian JP (2015) Parathyroid hormone: anabolic and catabolic actions on the skeleton. Curr Opin Pharmacol 22:41–50. https://doi.org/10.1016/j.coph.2015.03.005
Silvestrini G, Ballanti P, Leopizzi M et al (2007) Effects of intermittent parathyroid hormone (PTH) administration on SOST mRNA and protein in rat bone. J Mol Histol 38(4):261–269. https://doi.org/10.1007/s10735-007-9096-3
Tepel M, Armbruster FP, Grön HJ et al (2013) Nonoxidized, biologically active parathyroid hormone determines mortality in hemodialysis patients. J Clin Endocrinol Metab 98(12):4744–4751. https://doi.org/10.1210/jc.2013-2139
Tweedy WR, Bell WP, Vicens-Rios C et al (1935) Further chemical studies on a parathyroid hormone. J Bio Chem 108(1):105–112. https://doi.org/10.1016/S0021-9258(18)75313-1
Ursem SR, Heijboer AC, D’Haese PC et al (2021) Non-oxidized parathyroid hormone (PTH) measured by current method is not superior to total PTH in assessing bone turnover in chronic kidney disease. Kidney Int 99(5):1173–1178. https://doi.org/10.1016/j.kint.2020.12.024
Ursem SR, Vervloet MG, de Jongh RT et al (2020) Oxidation of parathyroid hormone. Clin Chim Acta 506:84–91. https://doi.org/10.1016/j.cca.2020.03.020
van Lierop AH, van der Eerden AW, Hamdy NA et al (2012) Circulating sclerostin levels are decreased in patients with endogenous hypercortisolism and increase after treatment. J Clin Endocrinol Metab 97(10):E1953-7. https://doi.org/10.1210/jc.2012-2218
van Lierop AH, Witteveen JE, Hamdy NA et al (2010) Patients with primary hyperparathyroidism have lower circulating sclerostin levels than euparathyroid controls. Eur J Endocrinol 163(5):833–837. https://doi.org/10.1530/EJE-10-0699
Wang FS, Ko JY, Yeh DW et al (2008) Modulation of Dickkopf-1 attenuates glucocorticoid induction of osteoblast apoptosis, adipocytic differentiation, and bone mass loss. Endocrinology 149(4):1793–801. https://doi.org/10.1210/en.2007-0910
Wolf M (2010) Forging forward with 10 burning questions on FGF23 in kidney disease. J Am Soc Nephrol 21(9):1427–1435. https://doi.org/10.1681/ASN.2009121293
Yamada S, Tsuruya K, Tokumoto M et al (2015) Factors associated with serum soluble inhibitors of Wnt-β-catenin signaling (sclerostin and dickkopf-1) in patients undergoing peritoneal dialysis. Nephrology (Carlton) 20(9):639–645. https://doi.org/10.1111/nep.12509
Yan JY, Tian FM, Wang WY et al (2014) Parathyroid hormone (1–34) prevents cartilage degradation and preserves subchondral bone micro-architecture in guinea pigs with spontaneous osteoarthritis. Osteoarthritis Cartilage 22(11):1869–1877. https://doi.org/10.1016/j.joca.2014.07.013
Yang CY, Chang ZF, Chau YP et al (2015) Circulating Wnt/β-catenin signalling inhibitors and uraemic vascular calcifications. Nephrol Dial Transplant 30(8):1356–1363. https://doi.org/10.1093/ndt/gfv043
Yeo FE, Villines TC, Bucci JR et al (2004) Cardiovascular risk in stage 4 and 5 nephropathy. Adv Chronic Kidney Dis 11(2):116–133. https://doi.org/10.1053/j.arrt.2004.01.010
Zeng S, Querfeld U, Feger M et al (2020) Relationship between GFR, intact PTH, oxidized PTH, non-oxidized PTH as well as FGF23 in patients with CKD. FASEB J 34(11):15269–15281. https://doi.org/10.1096/fj.202000596R
Zeng S, Slowinski T, Pommer W et al (2020) Sclerostin is an independent risk factor for all-cause mortality in kidney transplant recipients. Clin Exp Nephrol 24(12):1177–1183. https://doi.org/10.1007/s10157-020-01956-y
Zull JE, Smith SK, Wiltshire R (1990) Effect of methionine oxidation and deletion of amino-terminal residues on the conformation of parathyroid hormone. Circular dichroism studies. J Biol Chem 265(10):5671–5676. https://doi.org/10.1016/S0021-9258(19)39415-3
Acknowledgements
We would like to thank B. Yard to offer us experimental workplace and professional technique guidance.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors have no funding sources to report.
Author information
Authors and Affiliations
Contributions
B. Hocher designed the study; A.A. Hasan and B. Yard assisted with the data interpretation and preparing the manuscript; M. Li performed experiments, and together with C. Chu analyzed data and wrote the manuscript; JG. Hocher assisted in analyzing data; Y. Liu improved grammars and wording; B. Hocher, B. Yard, C. Chu, X.L. Zhang, X. Chen and B.K. Krämer revised the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Commission of Charité University, Berlin, Germany.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, M., Hasan, A.A., Chu, C. et al. Only bioactive forms of PTH (n-oxPTH and Met18(ox)-PTH) inhibit synthesis of sclerostin – evidence from in vitro and human studies. Pflugers Arch - Eur J Physiol 476, 889–899 (2024). https://doi.org/10.1007/s00424-024-02928-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-024-02928-x