Abstract
Background
Robotic surgical systems with full articulation of instruments, tremor filtering, and motion scaling can potentially overcome the procedural difficulties in endoscopic surgeries. However, whether robot-assisted minimally invasive esophagectomy (RAMIE) can overcome anatomical difficulties during thoracoscopic esophagectomy remains unclear. This study aimed to clarify the anatomical and clinical factors that influence the difficulty of RAMIE in the thoracic region.
Methods
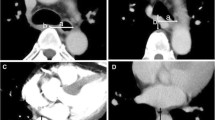
Forty-five patients who underwent curative-intent RAMIE with upper mediastinal lymph node dissection for esophageal cancer were included. Using preoperative computed tomography images, we calculated previously reported anatomical indices to assess the upper mediastinal narrowness and vertebral body projections in the middle thoracic region. The factors influencing thoracic operative time were then investigated.
Results
During the thoracic procedure, the median operative time was 215 (124–367) min and the median blood loss was 20 (5–190) mL. Postoperatively, pneumonia, anastomotic leakage, and recurrent laryngeal nerve palsy occurred in 17.8%, 2.2%, and 6.7% of the patients, respectively. The multiple linear regression model revealed that a narrow upper mediastinum and greater blood loss during the thoracic procedure were significant factors associated with a prolonged thoracic operative time (P = 0.025 and P < 0.001, respectively). Upper mediastinal narrowing was not associated with postoperative complications.
Conclusions
A narrow upper mediastinum was significantly associated with a prolonged thoracic operative time in patients with RAMIE.


Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Takeuchi H, Kawakubo H, Kitagawa Y (2013) Current status of minimally invasive esophagectomy for patients with esophageal cancer. Gen Thorac Cardiovasc Surg 61(9):513–521
Kawakubo H, Takeuchi H, Kitagawa Y (2013) Current status and future perspectives on minimally invasive esophagectomy. Korean J Thorac Cardiovasc Surg 46(4):241–248
Marubashi S, Takahashi A, Kakeji Y, Hasegawa H, Ueno H, Eguchi S, Endo I, Goi T, Saiura A, Sasaki A, Takiguchi S, Takeuchi H, Tanaka C, Hashimoto M, Hiki N, Horiguchi A, Masaki T, Yoshida K, Gotoh M, Konno H, Yamamoto H, Miyata H, Seto Y, Kitagawa Y (2021) Surgical outcomes in gastroenterological surgery in Japan: report of the National Clinical Database 2011–2019. Ann Gastroenterol Surg 5(5):639–658
Yoshida N, Baba Y, Shigaki H, Shiraishi S, Harada K, Watanabe M, Iwatsuki M, Kurashige J, Sakamoto Y, Miyamoto Y, Ishimoto T, Kosumi K, Tokunaga R, Yamashita Y, Baba H (2016) Effect of esophagus position on surgical difficulty and postoperative morbidities after thoracoscopic esophagectomy. Semin Thorac Cardiovasc Surg 28(1):172–179
Okamoto K, Inaki N, Saito H, Shimada M, Yamaguchi T, Tsuji T, Moriyama, Kinoshita J, Makino I, Nakamra K, Takamura H, Ninomiya I (2023) Analysis of factors associated with operative difficulty in thoracoscopic esophageal cancer surgery in the left-decubitus position: a single-center retrospective study. BMC Surg 23(1):242
Okamura A, Watanabe M, Mine S, Nishida K, Imamura Y, Kurogochi T, Kitagawa Y, Sano T (2016) Factors influencing difficulty of the thoracic procedure in minimally invasive esophagectomy. Surg Endosc 30(10):4279–4285
Hosoda K, Niihara M, Harada H, Yamashita K, Hiki N (2020) Robot-assisted minimally invasive esophagectomy for esophageal cancer: meticulous surgery minimizing postoperative complications. Ann Gastroenterol Surg 4(6):608–617
Rice TW, Patil DT, Blackstone EH (2017) 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: application to clinical practice. Ann Cardiothorac Surg 6(2):119–130
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, e Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Haga Y, Beppu T, Doi K, Nozawa F, Mugita N, Ikei S, Ogawa M (1997) Systemic inflammatory response syndrome and organ dysfunction following gastrointestinal surgery. Crit Care Med 25(12):1994–2000
Okamura A, Takeuchi H, Matsuda S, Ogura M, Miyasho T, Nakamura R, Takahashi T, Wada N, Kawakubo H, Saikawa Y, Kitagawa Y (2015) Factors affecting cytokine change after esophagectomy for esophageal cancer. Ann Surg Oncol 22(9):3130–3135
Violette PD, Mikhail D, Pond GR, Pautler SE (2015) Independent predictors of prolonged operative time during robotic-assisted radical prostatectomy. J Robot Surg 9(2):117–123
Haveman I, van Weelden WJ, Roovers EA, Kraayenbrink AA, Dijkhuizen F (2022) Robot-assisted total laparoscopic hysterectomy in different classes of obesity: a cohort study. JSLS 26(1):e202100077. https://doi.org/10.4293/JSLS.2021.00077
Acknowledgements
We would like to thank Editage for the English language editing.
Funding
There are no funding resources to be reported or declared.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of this study. K.K., A.O., and J.K. collected and analyzed the data. The first draft of the manuscript was written by K.K. and A.O., and all authors commented on previous versions of the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no related conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
423_2024_3378_MOESM1_ESM.tiff
Supplementary Material 1: Fig. 1 association between the UMI and the numbers of right recurrent laryngeal nerve (RRLN) or left recurrent laryngeal nerve (LRLN) retrieved rs indicates Spearman’s rank correlation coefficient. (A) Number of RRLN lymph nodes retrieved and upper mediastinal index. (B) Number of LRLN lymph nodes retrieved and middle mediastinal index.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuriyama, K., Okamura, A., Kanamori, J. et al. Anatomical factor associated with thoracic procedural difficulty in robot-assisted minimally invasive esophagectomy. Langenbecks Arch Surg 409, 190 (2024). https://doi.org/10.1007/s00423-024-03378-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03378-w