Abstract
Purpose
Positive pathologic lymph nodes in colorectal cancer represent an important prognostic indicator. Whether lymph node distribution or the number of metastatic nodes is more strongly associated with survival prediction remains controversial.
Methods
Among 3449 colorectal cancer surgeries performed at Nagasaki University Hospital and five affiliated institutions from April 2016 to March 2022, we investigated 604 patients who underwent laparoscopic radical resection and were diagnosed with pathological stage III cancer. Patients were divided into two groups according to whether they had central vessel metastasis (LND3 group, n=42) or not (LND1/2 group, n=562). After adjusting for background factors using propensity score matching, the LND3 group included 42 patients and the LND1/2 group included 40 patients. Patient background characteristics and prognosis were compared between these two groups.
Results
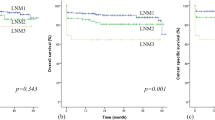
Before matching, frequencies of right-side colon cancer (64.3% vs 38.1%, p=0.001), multivisceral resection (11.9% vs 4.4%, p=0.039), clinical N2 status (40.5% vs 22.6%, p=0.032), and pathological N2 (73.8% vs 22.6%, p<0.001) were all greater, and the number of lymph nodes retrieved was higher (24 vs 19, p=0.042) in the LND3 group. After matching, no differences in any clinical factors were evident between groups. Five-year RFS (44.8% vs 77.1%, p=0.004) and OS (43.1% vs 83.2%, p<0.001) were worse in the LND3 group. Adjuvant chemotherapy improved RFS (adjuvant chemotherapy (+) vs adjuvant chemotherapy (−): 62.1% vs 27.7%, p=0.047) in the LND3 group.
Conclusion
LND3-positive patients show poorer prognosis than LND1/2 patients and should be treated with an appropriate perioperative treatment strategy.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Color Dis 11(4):354–364 discussion 64-5
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W et al (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30(15):1763–1769
Merrie AE, Phillips LV, Yun K, McCall JL (2001) Skip metastases in colon cancer: assessment by lymph node map** using molecular detection. Surgery. 129(6):684–691
**e D, Yu C, Gao C, Osaiweran H, Hu J, Gong J (2017) An optimal approach for laparoscopic D3 lymphadenectomy plus complete mesocolic excision (D3+CME) for right-sided colon cancer. Ann Surg Oncol 24(5):1312–1313
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ et al (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21(15):2912–2919
Tominaga T, Yamaguchi T, Nagasaki T, Akiyoshi T, Nagayama S, Fukunaga Y et al (2021) Improved oncologic outcomes with increase of laparoscopic surgery in modified complete mesocolic excision with D3 lymph node dissection for T3/4a colon cancer: results of 1191 consecutive patients during a 10-year period: a retrospective cohort study. Int J Clin Oncol 26(5):893–902
Hashiguchi Y, Hase K, Ueno H, Mochizuki H, Kajiwara Y, Ichikura T et al (2010) Prognostic significance of the number of lymph nodes examined in colon cancer surgery: clinical application beyond simple measurement. Ann Surg 251(5):872–881
Newland RC, Dent OF, Lyttle MN, Chapuis PH, Bokey EL (1994) Pathologic determinants of survival associated with colorectal cancer with lymph node metastases. A multivariate analysis of 579 patients. Cancer. 73(8):2076–2082
Huh JW, Kim CH, Kim HR, Kim YJ (2012) Factors predicting oncologic outcomes in patients with fewer than 12 lymph nodes retrieved after curative resection for colon cancer. J Surg Oncol 105(2):125–129
Kim CH, Huh JW, Kim HR, Kim YJ (2014) Prognostic comparison between number and distribution of lymph node metastases in patients with right-sided colon cancer. Ann Surg Oncol 21(4):1361–1368
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T et al (2020) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol 25(1):1–42
Kobayashi H, Enomoto M, Higuchi T, Uetake H, Iida S, Ishikawa T et al (2011) Clinical significance of lymph node ratio and location of nodal involvement in patients with right colon cancer. Dig Surg 28(3):190–197
Kanemitsu Y, Komori K, Kimura K, Kato T (2013) D3 lymph node dissection in right hemicolectomy with a no-touch isolation technique in patients with colon cancer. Dis Colon Rectum 56(7):815–824
Shatari T, Fujita M, Nozawa K, Haku K, Niimi M, Ikeda Y et al (2003) Vascular anatomy for right colon lymphadenectomy. Surg Radiol Anat 25(2):86–88
Garćia-Ruiz A, Milsom JW, Ludwig KA, Marchesa P (1996) Right colonic arterial anatomy. Implications for laparoscopic surgery. Dis Colon Rectum 39(8):906–911
Nagasaki T, Akiyoshi T, Fujimoto Y, Konishi T, Nagayama S, Fukunaga Y et al (2015) Prognostic impact of distribution of lymph node metastases in stage III colon cancer. World J Surg 39(12):3008–3015
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y et al (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20(2):207–239
Balciscueta Z, Balciscueta I, Uribe N, Pellino G, Frasson M, Garcia-Granero E et al (2021) D3-lymphadenectomy enhances oncological clearance in patients with right colon cancer. Result of a meta-analysis. Eur J Surg Oncol 47(7):1541–1551
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
West NP, Morris EJ, Rotimi O, Cairns A, Finan PJ, Quirke P (2008) Pathology grading of colon cancer surgical resection and its association with survival: a retrospective observational study. Lancet Oncol 9(9):857–865
Zurleni T, Cassiano A, Gjoni E, Ballabio A, Serio G, Marzoli L et al (2018) Surgical and oncological outcomes after complete mesocolic excision in right-sided colon cancer compared with conventional surgery: a retrospective, single-institution study. Int J Color Dis 33(1):1–8
Benson AB 3rd, Venook AP, Cederquist L, Chan E, Chen YJ, Cooper HS et al (2017) Colon Cancer, Version 1.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 15(3):370–398
Weber K, Merkel S, Perrakis A, Hohenberger W (2013) Is there a disadvantage to radical lymph node dissection in colon cancer? Int J Color Dis 28(2):217–226
Cho MS, Baek SJ, Hur H, Soh Min B, Baik SH, Kyu KN (2015) Modified complete mesocolic excision with central vascular ligation for the treatment of right-sided colon cancer: long-term outcomes and prognostic factors. Ann Surg 261(4):708–715
Kim JC, Lee KH, Yu CS, Kim HC, Kim JR, Chang HM et al (2004) The clinicopathological significance of inferior mesenteric lymph node metastasis in colorectal cancer. Eur J Surg Oncol 30(3):271–279
Bertelsen CA, Kirkegaard-Klitbo A, Nielsen M, Leotta SM, Daisuke F, Gögenur I (2016) Pattern of colon cancer lymph node metastases in patients undergoing central mesocolic lymph node excision: a systematic review. Dis Colon Rectum 59(12):1209–1221
Kataoka K, Beppu N, Shiozawa M, Ikeda M, Tomita N, Kobayashi H et al (2020) Colorectal cancer treated by resection and extended lymphadenectomy: patterns of spread in left- and right-sided tumours. Br J Surg 107(8):1070–1078
Sehgal R, Coffey JC (2014) Historical development of mesenteric anatomy provides a universally applicable anatomic paradigm for complete/total mesocolic excision. Gastroenterol Rep (Oxf) 2(4):245–250
Cheong CK, Nistala KRY, Ng CH, Syn N, Chang HSY, Sundar R et al (2020) Neoadjuvant therapy in locally advanced colon cancer: a meta-analysis and systematic review. J Gastrointest Oncol 11(5):847–857
Author information
Authors and Affiliations
Contributions
KN and TT mainly designed the study and analyzed the data. TN, RO, KO, YT, MI, MH, HT, SO, and KI performed surgery and provided patient care. TN supervised this study.
Corresponding author
Ethics declarations
Ethics approval
This research study was conducted retrospectively using data obtained for clinical purposes, and was reviewed and approved by the Clinical Research Review Board of Nagasaki University Hospital (approval no. 16062715-5).
Consent to participate
Informed consent was obtained as part of routine care from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 28 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Noda, K., Tominaga, T., Nonaka, T. et al. Prognostic value of lymph node distribution after laparoscopic colectomy with Japanese D3 dissection. Langenbecks Arch Surg 409, 28 (2024). https://doi.org/10.1007/s00423-023-03222-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03222-7