Abstract
Background
Minimally invasive right hemicolectomy has been increasingly used for the treatment of right hemicolectomy disease, and both intracorporeal anastomosis (ICA) and extracorporeal anastomosis (ECA) are available to restore intestinal continuity. However, the advantages and disadvantages of these two anastomoses are highly controversial. The present meta-analysis evaluated the effectiveness of ICA versus ECA in minimally invasive right colectomy to improve the grade of evidence.
Methods
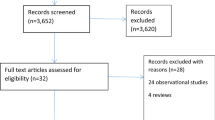
We searched the PubMed, Embase, Cochrane Library, and Web of Science databases for randomized controlled trials (RCTs) comparing intracorporeal versus extracorporeal anastomosis in laparoscopic or robotic right hemicolectomy published from database inception to February 2023. Two researchers performed the literature review, data extraction, bias assessment, and meta-analysis of the data using Review Manager 5.4 software.
Results
Seven RCTs with a total of 750 patients were included in the meta-analysis. The results showed a lower incidence of postoperative paralytic ileus (RR 0.62, 95% CI 0.39 ~ 0.99, p = 0.04) and shorter incision length (MD − 1.38; 95% CI: − 1.98 ~ − 0.78, p < 0.00001), but longer operative time (MD 10.69; 95% CI: 2.76 ~ 18.63, p = 0.008). The remaining events including bleeding (RR 0.49, 95% CI: 0.12 ~ 2.04, p = 0.33), anastomotic leak (RR 0.62, 95% CI: 0.39 ~ 0.99, p = 0.85), surgical site infection (RR 0.15, 95% CI: 0.22 ~ 1.25, p = 0.15), overall perioperative morbidity (RR 0.86, 95% CI: 0.58 ~ 1.26, p = 0.44), number of harvested lymph nodes (MD 0.75; 95% CI: − 0.15 ~ 1.65, p = 0.10), and length of hospital stay (MD − 0.27; 95% CI: − 0.91 ~ 0.38, p = 0.42) were not statistically significant.
Conclusions
Compared to ECA, ICA in minimally invasive right hemicolectomy reduced the risk of postoperative paralytic ileus and shortened the length of the incision but prolonged the operative time.




Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this manuscript will be made available by the authors without undue reservation to any qualified researcher.
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1(3):144–150
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta M A, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10(1):44–52. https://doi.org/10.1016/s1470-2045(08)70310-3
Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059. https://doi.org/10.1056/NEJMoa032651
Samia H, Lawrence J, Nobel T, Stein S, Champagne BJ, Delaney CP (2013) Extraction site location and incisional hernias after laparoscopic colorectal surgery: should we be avoiding the midline? Am J Surg 205(3):264–267; discussion 268. https://doi.org/10.1016/j.amjsurg.2013.01.006
Biondi A, Di Mauro G, Morici R, Sangiorgio G, Vacante M, Basile F (2021) Intracorporeal versus extracorporeal anastomosis for laparoscopic right hemicolectomy: short-term outcomes. J Clin Med 10(24). https://doi.org/10.3390/jcm10245967
Małczak P, Wysocki M, Pisarska-Adamczyk M, Major P, Pędziwiatr M (2022) Bowel function after laparoscopic right hemicolectomy: a randomized controlled trial comparing intracorporeal anastomosis and extracorporeal anastomosis. Surg Endosc 36(7):4977–4982. https://doi.org/10.1007/s00464-021-08854-8
Liao CK, Chern YJ, Lin YC, Hsu YJ, Chiang JM, Tsai WS, Hsieh PS, Hung HY, Yeh CY, You JF (2021) Short- and medium-term outcomes of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: a propensity score-matched study. World J Surg Oncol 19(1):6. https://doi.org/10.1186/s12957-020-02112-2
Grieco M, Marcellinaro R, Spoletini D, Menditto R, Lisi G, Russo G, Napoleone V, Carlini M (2022) Laparoscopic right colectomy: changes in surgical technique and perioperative management allow better postoperative results in a comparative series of 361 patients. Updates Surg 74(3):883–890. https://doi.org/10.1007/s13304-022-01287-5
Popeskou SG, Horvath Z, Mongelli F, Roesel R, Cristaudi A, Garofalo F, Christoforidis D (2022) Bowel recovery after intra- vs extra-corporeal anastomosis for oncologic laparoscopic right hemicolectomy within an ERAS protocol: a retrospective study. Langenbecks Arch Surg 407(6):2463–2469. https://doi.org/10.1007/s00423-022-02585-7
Veneroni S, Palini GM, Pirrera B, Fantini E, Monari F, Alagna V, Vallicelli C, Garulli G (2022) Intracorporeal anastomosis versus extracorporeal anastomosis after laparoscopic right hemicolectomy for colon cancer: morbidity comparison at long-term follow-up. Minerva Surg 77(6):531–535. https://doi.org/10.23736/s2724-5691.22.09281-4
Emile SH, Elfeki H, Shalaby M, Sakr A, Bassuni M, Christensen P, Wexner SD (2019) Intracorporeal versus extracorporeal anastomosis in minimally invasive right colectomy: an updated systematic review and meta-analysis. Techniques in Coloproctology 23(11):1023–1035. https://doi.org/10.1007/s10151-019-02079-7
Hajibandeh S, Hajibandeh S, Mankotia R, Akingboye A, Peravali R (2021) Meta-analysis of randomised controlled trials comparing intracorporeal versus extracorporeal anastomosis in laparoscopic right hemicolectomy: upgrading the level of evidence. Updates Surg 73(1):23–33. https://doi.org/10.1007/s13304-020-00948-7
Lam TJR, Udonwa SA, Yaow CYL, Nistala KRY, Chong CS (2022) Intracorporeal Versus Extracorporeal Anastomosis in Laparoscopic Colectomy: A Meta-Analysis and Systematic Review Current Colorectal. Cancer Rep 18(1):1–17. https://doi.org/10.1007/s11888-022-00473-2
Liang Y, Li L, Su Q, Liu Y, Yin H, Wu D (2022) Short-term outcomes of intracorporeal and extracorporeal anastomosis in robotic right colectomy: a systematic review and meta-analysis. Tech Coloproctol 26(7):529–535. https://doi.org/10.1007/s10151-022-02599-9
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Hozo S P, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A, Collaboration DESD (2020) Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res 29(9):2520–2537. https://doi.org/10.1177/0962280219889080
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Allaix ME, Degiuli M, Bonino MA, Arezzo A, Mistrangelo M, Passera R, Morino M (2019) Intracorporeal or extracorporeal ileocolic anastomosis after laparoscopic right colectomy: a double-blinded randomized controlled trial. Ann Surg 270(5):762–767. https://doi.org/10.1097/SLA.0000000000003519
Bollo J, Turrado V, Rabal A, Carrillo E, Gich I, Martinez MC, Hernandez P, Targarona E (2020) Randomized clinical trial of intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy (IEA trial). Br J Surg 107(4):364–372. https://doi.org/10.1002/bjs.11389
Dohrn N, Yikilmaz H, Laursen M, Khesrawi F, Clausen FB, Sorensen F, Jakobsen HL, Brisling S, Lykke J, Eriksen JR, Klein MF, Gogenur I (2022) Intracorporeal versus extracorporeal anastomosis in robotic right colectomy: a multicenter, triple-blind, randomized clinical trial. Ann Surg 276(5):e294-e301. https://doi.org/10.1097/SLA.0000000000005254
Ferrer-Márquez M, Rubio-Gil F, Torres-Fernández R, Moya-Forcén P, Belda-Lozano R, Arroyo-Sebastián A, Benavides-Buleje J, Reina-Duarte A (2021) Intracorporeal versus extracorporeal anastomosis in patients undergoing laparoscopic right hemicolectomy: a multicenter randomized clinical trial (The IVEA-study). Surg Laparosc Endosc Percutan Tech 31(4):408–413. https://doi.org/10.1097/sle.0000000000000937
Mari GM, Crippa J, Costanzi ATM, Pellegrino R, Siracusa C, Berardi V, Maggioni D (2018) Intracorporeal anastomosis reduces surgical stress response in laparoscopic right hemicolectomy: a prospective randomized trial. Surg Laparosc Endosc Percutan Tech 28(2):77–81. https://doi.org/10.1097/sle.0000000000000506
Vignali A, Bissolati M, De Nardi P, Di Palo S, Staudacher C (2016) Extracorporeal vs. intracorporeal ileocolic stapled anastomoses in laparoscopic right colectomy: an interim analysis of a randomized clinical trial. J Laparoendosc Adv Surg Tech A 26(5):343–348. https://doi.org/10.1089/lap.2015.0547
Fabozzi M, Allieta R, Brachet Contul R, Grivon M, Millo P, Lale-Murix E, Nardi M Jr (2010) Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc 24(9):2085–2091. https://doi.org/10.1007/s00464-010-0902-8
Biondi A, Santocchi P, Pennestrì F, Santullo F, D'Ugo D, Persiani R (2017) Totally laparoscopic right colectomy versus laparoscopically assisted right colectomy: a propensity score analysis. Surg Endosc 31(12):5275–5282. https://doi.org/10.1007/s00464-017-5601-2
Cleary RK, Kassir A, Johnson CS, Bastawrous AL, Soliman MK, Marx DS, Giordano L, Reidy TJ, Parra-Davila E, Obias VJ, Carmichael JC, Pollock D, Pigazzi A (2018) Intracorporeal versus extracorporeal anastomosis for minimally invasive right colectomy: a multi-center propensity score-matched comparison of outcomes. PLoS One 13(10):e0206277. https://doi.org/10.1371/journal.pone.0206277
Milone M, Elmore U, Di Salvo E, Delrio P, Bucci L, Ferulano GP, Napolitano C, Angiolini MR, Bracale U, Clemente M, D'Ambra M, Luglio G, Musella M, Pace U, Rosati R, Milone F (2015) Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 29(8):2314–2320. https://doi.org/10.1007/s00464-014-3950-7
Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D (2016) Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 30(9):3823–3829. https://doi.org/10.1007/s00464-015-4684-x
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91. https://doi.org/10.1097/01.sla.0000167857.14690.68
Hanna MH, Hwang GS, Phelan MJ, Bui TL, Carmichael JC, Mills SD, Stamos MJ, Pigazzi A (2016) Laparoscopic right hemicolectomy: short- and long-term outcomes of intracorporeal versus extracorporeal anastomosis. Surg Endosc 30(9):3933–3942. https://doi.org/10.1007/s00464-015-4704-x
Orcutt ST, Balentine CJ, Marshall CL, Robinson CN, Anaya DA, Artinyan A, Awad SS, Berger DH, Albo D (2012) Use of a Pfannenstiel incision in minimally invasive colorectal cancer surgery is associated with a lower risk of wound complications. Tech Coloproctol 16(2):127–132. https://doi.org/10.1007/s10151-012-0808-7
Benlice C, Stocchi L, Sapci I, Gorgun E, Kessler H, Liska D, Steele SR, Delaney CP (2019) Impact of the extraction-site location on wound infections after laparoscopic colorectal resection. Am J Surg 217(3):502–506. https://doi.org/10.1016/j.amjsurg.2018.10.034
Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA, Minni F (2017) A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbecks Arch Surg 402(3):417–427. https://doi.org/10.1007/s00423-016-1509-x
Baqar AR, Wilkins S, Wang W C, Oliva K, Centauri S, Yap R, McMurrick P (2022) A comparison of extracorporeal side to side or end to side anastomosis following a laparoscopic right hemicolectomy for colon cancer. ANZ J Surg 92(6):1472–1479. https://doi.org/10.1111/ans.17701
Jian-Cheng T, Shu-Sheng W, Bo Z, Jian F, Liang Z (2016) Total laparoscopic right hemicolectomy with 3-step stapled intracorporeal isoperistaltic ileocolic anastomosis for colon cancer: an evaluation of short-term outcomes Medicine (Baltimore) 95(48):e5538. https://doi.org/10.1097/md.0000000000005538
Machowicz J, Wołkowski M, Jabłońska B, Mrowiec S (2022) Ileocolonic anastomosis-comparison of different surgical techniques: a single-center study. Medicine (Baltimore) 101(51):e31582. https://doi.org/10.1097/md.0000000000031582
Author information
Authors and Affiliations
Contributions
Weizheng Mao designed the study. Tuo Zhang screened the literature, extracted the data, and completed the graphing and writing. Yigong Sun screened the literature and extracted the data. All authors contributed to the writing and revisions of the paper and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants performed by any of the authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, T., Sun, Y. & Mao, W. Meta‑analysis of randomized controlled trials comparing intracorporeal versus extracorporeal anastomosis in minimally invasive right hemicolectomy: upgrading the level of evidence. Int J Colorectal Dis 38, 147 (2023). https://doi.org/10.1007/s00384-023-04445-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04445-2