Abstract
Objective
The objective of this study was to summarize relevant data from previous reports and perform a meta-analysis to compare short-term surgical outcomes and long-term oncological outcomes between emergency and elective surgery for colorectal cancer (CRC).
Methods
A systematic literature search was performed using PubMed and Embase databases, and relevant data were extracted. Postoperative morbidity, hospital mortality within 30 days, postoperative recovery, overall survival (OS), and relapse-free survival (RFS) were compared using a fixed or random-effect model.
Results
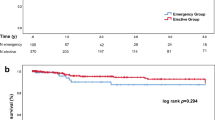
A total of 28 studies involving 353,686 participants were enrolled for this systematic review and meta-analysis, and 23.5% (83,054/353,686) of CRC patients underwent emergency surgery. The incidence of emergency presentations in CRC patients ranged from 2.7 to 38.8%. The lymph node yield of emergency surgery was comparable to that of elective surgery (WMD:0.70, 95%CI: − 0.74,2.14, P = 0.340; I2 = 80.6%). Emergency surgery had a higher risk of postoperative complications (OR:1.83, 95%CI:1.62–2.07, P < 0.001; I2 = 10.6%) and hospital mortality within 30 days (OR:4.62, 95%CI:4.18–5.10, P < 0.001; I2 = 42.9%) than elective surgery for CRC. In terms of long-term oncological outcomes, emergency surgery was significantly associated with poorer RFS (HR: 1.51, 95%CI:1.24–1.83, P < 0.001; I2 = 58.9%) and OS(HR:1.60, 95%CI: 1.47–1.73, P < 0.001; I2 = 63.4%) of CRC patients. In addition, the subgroup analysis for colon cancer patients revealed a pooled HR of 1.73 for OS (95%CI:1.52–1.96, P < 0.001), without the evidence of significant heterogeneity (I2 = 21.2%).
Conclusion
Emergency surgery for CRC had an adverse impact on short-term surgical outcomes and long-term survival. A focus on early screening programs and health education was warranted to reduce emergency presentations of CRC patients.






Similar content being viewed by others
Data availability
All data are available from its supplementary files.
References
Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A (2017) Colorectal cancer statistics. CA: Canc J Clin 67(3):177–193. https://doi.org/10.3322/caac.21395
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA: a Canc J Clin 66(2):115–132. https://doi.org/10.3322/caac.21338
Amri R, Bordeianou LG, Sylla P, Berger DL (2015) Colon cancer surgery following emergency presentation: effects on admission and stage-adjusted outcomes. Am J Surg 209(2):246–253. https://doi.org/10.1016/j.amjsurg.2014.07.014
Aquina CT, Becerra AZ, Xu Z, Boscoe FP, Schymura MJ, Noyes K, Monson JRT, Fleming FJ (2017) Nonelective colon cancer resection: a continued public health concern. Surgery 161(6):1609–1618. https://doi.org/10.1016/j.surg.2017.01.001
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91(5):605–609. https://doi.org/10.1002/bjs.4456
Oliphant R, Mansouri D, Nicholson GA, McMillan DC, Horgan PG, Morrison DS (2014) Emergency presentation of node-negative colorectal cancer treated with curative surgery is associated with poorer short and longer-term survival. Int J Colorectal Dis 29(5):591–598. https://doi.org/10.1007/s00384-014-1847-5
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 11(7):733–739. https://doi.org/10.1111/j.1463-1318.2008.01613.x
Chiarugi M, Galatioto C, Panicucci S, Scassa F, Zocco G, Seccia M (2007) Oncologic colon cancer resection in emergency: are we doing enough? Surg Oncol 16(Suppl 1):S73-77. https://doi.org/10.1016/j.suronc.2007.10.019
Lee CHA, Kong JCH, Heriot AG, Warrier S, Zalcberg J, Sitzler P (2019) Short-term outcome of emergency colorectal cancer surgery: results from Bi-National Colorectal Cancer Audit. Int J Colorectal Dis 34(1):63–69. https://doi.org/10.1007/s00384-018-3169-5
Kundes F, Kement M, Cetin K, Kaptanoglu L, Kocaoglu A, Karahan M, Yegen SF, Atici AE, Civil O, Eser M, Cakir T, Bildik N (2016) Evaluation of the patients with colorectal cancer undergoing emergent curative surgery. Springerplus 5(1):2024. https://doi.org/10.1186/s40064-016-3725-9
Wanis KN, Ott M, Van Koughnett JAM, Colquhoun P, Brackstone M (2018) Long-term oncological outcomes following emergency resection of colon cancer. Int J Colorectal Dis 33(11):1525–1532. https://doi.org/10.1007/s00384-018-3109-4
Askari A, Nachiappan S, Currie A, Bottle A, Abercrombie J, Athanasiou T, Faiz O (2017) Who requires emergency surgery for colorectal cancer and can national screening programmes reduce this need? Int J Surg (London, England) 42:60–68. https://doi.org/10.1016/j.ijsu.2017.04.050
Lavanchy JL, Vaisnora L, Haltmeier T, Zlobec I, Brugger LE, Candinas D, Schnuriger B (2019) Oncologic long-term outcomes of emergency versus elective resection for colorectal cancer. Int J Colorectal Dis 34(12):2091–2099. https://doi.org/10.1007/s00384-019-03426-8
Weixler B, Warschkow R, Ramser M, Droeser R, von Holzen U, Oertli D, Kettelhack C (2016) Urgent surgery after emergency presentation for colorectal cancer has no impact on overall and disease-free survival: a propensity score analysis. BMC Cancer 16:208. https://doi.org/10.1186/s12885-016-2239-8
Antony P, Harnoss JC, Warschkow R, Schmied BM, Schneider M, Tarantino I, Ulrich A (2019) Urgent surgery in colon cancer has no impact on survival. J Surg Oncol 119(8):1170–1178. https://doi.org/10.1002/jso.25469
Biondo S, Marti-Rague J, Kreisler E, Pares D, Martin A, Navarro M, Pareja L, Jaurrieta E (2005) A prospective study of outcomes of emergency and elective surgeries for complicated colonic cancer. Am J Surg 189(4):377–383. https://doi.org/10.1016/j.amjsurg.2005.01.009
Coco C, Verbo A, Manno A, Mattana C, Covino M, Pedretti G, Petito L, Rizzo G, Picciocchi A (2005) Impact of emergency surgery in the outcome of rectal and left colon carcinoma. World J Surg 29(11):1458–1464. https://doi.org/10.1007/s00268-005-7826-9
Ghazi S, Berg E, Lindblom A, Lindforss U (2013) Clinicopathological analysis of colorectal cancer: a comparison between emergency and elective surgical cases. World J Surg Oncol 11:133. https://doi.org/10.1186/1477-7819-11-133
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg (London, England) 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hrobjartsson A, Kirkham J, Juni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schunemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clinical research ed) 355:i4919. https://doi.org/10.1136/bmj.i4919
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Costa G, Lorenzon L, Massa G, Frezza B, Ferri M, Fransvea P, Mercantini P, Giustiniani MC, Balducci G (2017) Emergency surgery for colorectal cancer does not affect nodal harvest comparing elective procedures: a propensity score-matched analysis. Int J Colorectal Dis 32(10):1453–1461. https://doi.org/10.1007/s00384-017-2864-y
Patel SV, Patel SV, Brackstone M (2014) Emergency surgery for colorectal cancer does not result in nodal understaging compared with elective surgery. Canadian journal of surgery Journal canadien de chirurgie 57(5):349–353. https://doi.org/10.1503/cjs.019313
Sibio S, Di Giorgio A, D’Ugo S, Palmieri G, Cinelli L, Formica V, Sensi B, Bagaglini G, Di Carlo S, Bellato V, Sica GS (2019) Histotype influences emergency presentation and prognosis in colon cancer surgery. Langenbecks Arch Surg 404(7):841–851. https://doi.org/10.1007/s00423-019-01826-6
Wong SK, Jalaludin BB, Morgan MJ, Berthelsen AS, Morgan A, Gatenby AH, Fulham SB (2008) Tumor pathology and long-term survival in emergency colorectal cancer. Dis Colon Rectum 51(2):223–230. https://doi.org/10.1007/s10350-007-9094-2
Jestin P, Nilsson J, Heurgren M, Pahlman L, Glimelius B, Gunnarsson U (2005) Emergency surgery for colonic cancer in a defined population. Br J Surg 92(1):94–100. https://doi.org/10.1002/bjs.4780
Yoo PS, Mulkeen AL, Frattini JC, Longo WE, Cha CH (2006) Assessing risk factors for adverse outcomes in emergent colorectal surgery. Surg Oncol 15(2):85–89. https://doi.org/10.1016/j.suronc.2006.08.002
Littlechild J, Junejo M, Simons AM, Curran F, Subar D (2018) Emergency resection surgery for colorectal cancer: Patterns of recurrent disease and survival. World journal of gastrointestinal pathophysiology 9(1):8–17. https://doi.org/10.4291/wjgp.v9.i1.8
Crozier JE, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC (2009) Relationship between emergency presentation, systemic inflammatory response, and cancer-specific survival in patients undergoing potentially curative surgery for colon cancer. Am J Surg 197(4):544–549. https://doi.org/10.1016/j.amjsurg.2007.12.052
Hogan J, Samaha G, Burke J, Chang KH, Condon E, Waldron D, Coffey JC (2015) Emergency presenting colon cancer is an independent predictor of adverse disease-free survival. Int Surg 100(1):77–86. https://doi.org/10.9738/intsurg-d-13-00281.1
Bayar B, Yilmaz KB, Akinci M, Sahin A, Kulacoglu H (2016) An evaluation of treatment results of emergency versus elective surgery in colorectal cancer patients. Ulusal cerrahi dergisi 32(1):11–17. https://doi.org/10.5152/ucd.2015.2969
Banaszkiewicz Z, Woda L, Tojek K, Jarmocik P, Jawien A (2014) Colorectal cancer with intestinal perforation - a retrospective analysis of treatment outcomes. Contemporary oncology (Poznan, Poland) 18(6):414–418. https://doi.org/10.5114/wo.2014.46362
Sucullu I, Ozdemir Y, Cuhadar M, Balta AZ, Yucel E, Filiz AI, Gulec B (2015) Comparison of emergency surgeries for obstructed colonic cancer with elective surgeries: a retrospective study. Pakistan journal of medical sciences 31(6):1322–1327. https://doi.org/10.12669/pjms.316.8277
Ahmadinejad M, Pouryaghobi SM, Bayat F, Bolvardi E, Chokan NMJ, Masoumi B, Ahmadi K (2018) Surgical outcome and clinicopathological characteristics of emergency presentation elective cases of colorectal cancer. Archives of medical science : AMS 14(4):826–829. https://doi.org/10.5114/aoms.2016.61706
Xu Z, Becerra AZ, Aquina CT, Hensley BJ, Justiniano CF, Boodry C, Swanger AA, Arsalanizadeh R, Noyes K, Monson JR, Fleming FJ (2017) Emergent colectomy is independently associated with decreased long-term overall survival in colon cancer patients. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 21(3):543–553. https://doi.org/10.1007/s11605-017-3355-8
Norwood MG, Sutton AJ, West K, Sharpe DP, Hemingway D, Kelly MJ (2010) Lymph node retrieval in colorectal cancer resection specimens: national standards are achievable, and low numbers are associated with reduced survival. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 12(4):304–309. https://doi.org/10.1111/j.1463-1318.2009.01788.x
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 21(15):2912–2919. https://doi.org/10.1200/jco.2003.05.062
Okamura A, Takeuchi H, Matsuda S, Ogura M, Miyasho T, Nakamura R, Takahashi T, Wada N, Kawakubo H, Saikawa Y, Kitagawa Y (2015) Factors affecting cytokine change after esophagectomy for esophageal cancer. Ann Surg Oncol 22(9):3130–3135. https://doi.org/10.1245/s10434-014-4348-4
Lee WS, Baek JH, You DH, Nam MJ (2013) Prognostic value of circulating cytokines for stage III colon cancer. J Surg Res 182(1):49–54. https://doi.org/10.1016/j.jss.2012.08.051
Hendren S, Birkmeyer JD, Yin H, Banerjee M, Sonnenday C, Morris AM (2010) Surgical complications are associated with omission of chemotherapy for stage III colorectal cancer. Dis Colon Rectum 53(12):1587–1593. https://doi.org/10.1007/DCR.0b013e3181f2f202
Merkow RP, Bentrem DJ, Mulcahy MF, Chung JW, Abbott DE, Kmiecik TE, Stewart AK, Winchester DP, Ko CY, Bilimoria KY (2013) Effect of postoperative complications on adjuvant chemotherapy use for stage III colon cancer. Ann Surg 258(6):847–853. https://doi.org/10.1097/sla.0000000000000312
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van de Velde CJ (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12(6):575–582. https://doi.org/10.1016/s1470-2045(11)70097-3
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF, Grem JL, Grothey A, Hochster HS, Hoffe S, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Mulcahy MF, Murphy JD, Nurkin S, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Wuthrick E, Gregory KM, Gurski L, Freedman-Cass DA (2018) Rectal Cancer, Version 2.2018, NCCN clinical practice guidelines in oncology. J Nat Comprehen Canc Net: JNCCN 16(7):874–901. https://doi.org/10.6004/jnccn.2018.0061
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, Becker H, Raab HR, Villanueva MT, Witzigmann H, Wittekind C, Beissbarth T, Rodel C (2012) Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology 30(16):1926–1933. https://doi.org/10.1200/jco.2011.40.1836
Hwang MJ, Evans T, Lawrence G, Karandikar S (2014) Impact of bowel cancer screening on the management of colorectal cancer. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland 16(6):450–458. https://doi.org/10.1111/codi.12562
Pande R, Leung E, McCullough P, Smith S, Harmston C (2014) Impact of the United kingdom national bowel cancer awareness campaign on colorectal services. Dis Colon Rectum 57(1):70–75. https://doi.org/10.1097/01.dcr.0000437689.19579.97
Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, Garcia FAR, Gillman MW, Harper DM, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Owens DK, Phillips WR, Phipps MG, Pignone MP, Siu AL (2016) Screening for colorectal cancer: US preventive services task force recommendation statement. JAMA 315(23):2564–2575. https://doi.org/10.1001/jama.2016.5989
Funding
This work was supported by the General Scientific Research Project of Education Department of Zhejiang Province (Y201636252, Y202146966), the Zhejiang Provincial Key Project of Research and Development (2019C03043), the Health Science and Technology Plan of Zhejiang Province (2022RC165), and the Clinical Research Fund of the Zhejiang Medical Association (2021ZYC-A68).
Author information
Authors and Affiliations
Contributions
Haiyan Zhou conducted data analysis and drafted the original manuscript; Yongyan ** and Jun Wang contributed to data interpretation and statistical analysis; Guofeng Chen contributed to manuscript editing and preparation; Jian Chen and Shaojun Yu conceptualized study design and critically reviewed this manuscript. All authors read and approved the final edition.
Corresponding author
Ethics declarations
Ethical approval and informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, H., **, Y., Wang, J. et al. Comparison of short-term surgical outcomes and long-term survival between emergency and elective surgery for colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 38, 41 (2023). https://doi.org/10.1007/s00384-023-04334-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04334-8