Abstract
Purpose
Anastomotic leakage after low anterior resection for rectal cancer is a critical problem. Many risk factors have been suggested and surgical techniques have improved, but anastomotic leakage remains a major postoperative challenge. This study sought to create a nomogram for precise prediction of anastomotic leakage after low anterior resection for rectal cancer.
Methods
We used data of 936 patients that had been prospectively collected by the Japanese Society for Colon and Rectal Cancer between June 2010 and February 2013. Risk factors for anastomotic leakage were identified by multivariate logistic regression analysis and used to create a nomogram. The performance of the nomogram was evaluated by using a bootstrapped-concordance index and calibration plots.
Results
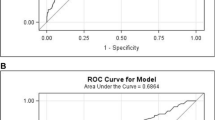
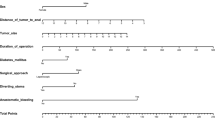
Sex, preoperative serum albumin, tumor location and diameter, and simultaneous resection of other organs were identified as significantly associated factors that could be combined for accurate prediction of anastomotic leakage. We created a nomogram for anastomotic leakage by using these risk factors. The area under the curve was 0.72 (95% confidence interval 0.67–0.76). The nomogram had a bootstrapped-concordance index of 0.72 and was well calibrated.
Conclusions
Our nomogram was a useful tool for precise prediction of anastomotic leakage after low anterior resection for rectal cancer.



Similar content being viewed by others
References
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 85(3):355–358. https://doi.org/10.1046/j.1365-2168.1998.00615.x
Enker WE, Merchant N, Cohen AM, Lanouette NM, Swallow C, Guillem J, Paty P, Minsky B, Weyrauch K, Quan SHQ (1999) Safety and efficacy of low anterior resection for rectal cancer: 681 consecutive cases from a specialty service. Ann Surg 230(4):544–552. https://doi.org/10.1097/00000658-199910000-00010
Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN (2005) Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Color Dis 7:51–57
Branagan G, Finnis D (2005) Prognosis after anastomotic leakage in colorectal surgery. Dis Colon rectum 48(5):1021–1026. https://doi.org/10.1007/s10350-004-0869-4
Merkel S, Wang WY, Schmidt O, Dworak O, Wittekind C, Hohenberger W et al (2001) Locoregional recurrence in patients with anastomotic leakage after anterior resection for rectal carcinoma. Color Dis 3(3):154–160. https://doi.org/10.1046/j.1463-1318.2001.00232.x
Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM, Tang R (2005) Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg 241(1):9–13
Law WI, Chu KW, Ho JW, Chan CW (2000) Risk factors for anastomotic leakage after low anterior resection with total mesorectal excision. Am J Surg 179(2):92–96. https://doi.org/10.1016/S0002-9610(00)00252-X
Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T et al (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92(2):211–216. https://doi.org/10.1002/bjs.4806
Battersby NJ, Bouliotis G, Emmertsen KJ, Juul T, Glynne-Jones R, Branagan G, Christensen P, Laurberg S, Moran BJ (2017) Development and external validation of a nomogram and online tool to predict bowel dysfunction following restorative rectal cancer resection: the POLARS score. Gut [Epub ahead of print]:gutjnl-2016-312695. https://doi.org/10.1136/gutjnl-2016-312695
Newton AD, Li J, Jeganathan AN, Mahmoud NN, Epstein AJ, Paulson EC (2016) A nomogram to predict lymph node positivity following neoadjuvant chemoradiation in locally advanced rectal cancer. Dis Colon rectum 59(8):710–717. https://doi.org/10.1097/DCR.0000000000000638
Hoshino N, Hasegawa S, Hida K, Kawada K, Ganeko R, Sugihara K, Sakai Y (2016) Nomogram for predicting recurrence in stage II colorectal cancer. Acta Oncol 55(12):1414–1417. https://doi.org/10.1080/0284186X.2016.1223881
Russell MC, You YN, Hu CY, Cormier JN, Feig BW, Skibber JM, Rodriguez-Bigas MA, Nelson H, Chang GJ (2013) A novel risk-adjusted nomogram for rectal cancer surgery outcomes. JAMA Surg 148(8):769–777. https://doi.org/10.1001/jamasurg.2013.2136
Jwa E, Kim JH, Han S, Park JH, Lim SB, Kim JC et al (2014) Nomogram to predict ypN status after chemoradiation in patients with locally advanced rectal cancer. Br J Cancer 111(2):249–254. https://doi.org/10.1038/bjc.2014.256
Shiomi A, Ito M, Maeda K, Kinugasa Y, Ota M, Yamaue H, Shiozawa M, Horie H, Kuriu Y, Saito N (2015) Effects of a diverting stoma on symptomatic anastomotic leakage after low anterior resection for rectal cancer: a propensity score matching analysis of 1,014 consecutive patients. J Am Coll Surg 220(2):186–194. https://doi.org/10.1016/j.jamcollsurg.2014.10.017
Katsuno H, Shiomi A, Ito M, Koide Y, Maeda K, Yatsuoka T, Hase K, Komori K, Minami K, Sakamoto K, Saida Y, Saito N (2016) Comparison of symptomatic anastomotic leakage following laparoscopic and open low anterior resection for rectal cancer: a propensity score matching analysis of 1014 consecutive patients. Surg Endosc 30(7):2848–2856. https://doi.org/10.1007/s00464-015-4566-2
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351. https://doi.org/10.1016/j.surg.2009.10.012
http://r-project.org/Accessed 6 January 2017
https://cran.r-project.org/web/packages/rms/Accessed 6 January 2017
Kawada K, Sakai Y (2016) Preoperative, intraoperative and postoperative risk factors for anastomotic leakage after laparoscopic low anterior resection with double stapling technique anastomosis. World J Gastroenterol 22(25):5718–5727. https://doi.org/10.3748/wjg.v22.i25.5718
Frasson M, Flor-Lorente B, Rodriguez JL, Granero-Castro P, Hervás D, Alvarez Rico MA et al (2015) Risk factors for anastomotic leak after colon resection for cancer: multivariate analysis and nomogram from a multicentric, prospective, national study with 3193 patients. Ann Surg 262(2):321–330. https://doi.org/10.1097/SLA.0000000000000973
Yao HH, Shao F, Huang Q, Wu Y, Qiang Zhu Z, Liang W (2014) Nomogram to predict anastomotic leakage after laparoscopic anterior resection with intracorporeal rectal transection and double-stapling technique anastomosis for rectal cancer. Hepato-Gastroenterology 61(133):1257–1261
Haskins IN, Baginsky M, Amdur RL, Agarwal S (2016) Preoperative hypoalbuminemia is associated with worse outcomes in colon cancer patients. Clin Nutr [Epub ahead of print]
Lai CC, You JF, Yeh CY, Chen JS, Tang R, Wang JY, Chin CC (2011) Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Color Dis 26(4):473–481. https://doi.org/10.1007/s00384-010-1113-4
Parthasarathy M, Greensmith M, Bowers D, Groot-Wassink T (2017) Risk factors for anastomotic leakage after colorectal resection: a retrospective analysis of 17518 patients. Color Dis 19(3):288–298. https://doi.org/10.1111/codi.13476
Rosello S, Cervantes A (2015) Extending neoadjuvant chemotherapy in rectal cancer. Lancet Oncol 16(8):880–881. https://doi.org/10.1016/S1470-2045(15)00092-3
Matsumoto T, Hasegawa S, Zaima M, Inoue N, Sakai Y (2015) Outcomes of neoadjuvant chemotherapy without radiation for rectal cancer. Dig Surg 32(4):275–283. https://doi.org/10.1159/000430469
Koike J, Funahashi K, Yoshimatsu K, Yokomizo H, Kan H, Yamada T, Ishida H, Ishibashi K, Saida Y, Enomoto T, Katsumata K, Hisada M, Hasegawa H, Koda K, Ochiai T, Sakamoto K, Shiokawa H, Ogawa S, Itabashi M, Kameoka S (2017) Efficacy and safety of neoadjuvant chemotherapy with oxaliplatin, 5-fluorouracil, and levofolinate for T3 or T4 stage II/III rectal cancer: the FACT trial. Cancer Chemother Pharmacol 79(3):519–525. https://doi.org/10.1007/s00280-017-3243-7
Glynne-Jones R, Hava N, Goh V, Bosompem S, Bridgewater J, Chau I et al (2015) Bevacizumab and Combination Chemotherapy in rectal cancer Until Surgery (BACCHUS): a phase II, multicentre, open-label, randomised study of neoadjuvant chemotherapy alone in patients with high-risk cancer of the rectum. BMC Cancer 15(1):764. https://doi.org/10.1186/s12885-015-1764-1
Acknowledgements
The following is a list of participating surgeons and centers: K. Komori (Aichi Cancer Center Hospital, Aichi), J. Okuda (Osaka Medical College Hospital, Osaka), K. Otsuka (Iwate Medical University School of Medicine, Iwate), A. Kanazawa (Japanese Red Cross Osaka Hospital, Osaka), M. Ueno (Cancer Institute Hospital, Tokyo), T. Masaki (Kyorin University Hospital, Tokyo), E. Otsuji (Kyoto Prefectural University of Medicine, Kyoto), T. Kusumi (Keiyukai Sapporo Hospital, Hokkaido), K. Minami (National Hospital Organization Kyusyu Cancer Center, Fukuoka), T. Kobatake (National Hospital Organization Shikoku Cancer Center, Ehime), Y. Nishimura (Saitama Cancer Center, Saitama), K. Sakamoto (Juntendo University Hospital, Tokyo), K. Sugihara (Tokyo Medical and Dental University, Tokyo), S. Kameoka (Tokyo Women’s Medical University Hospital, Tokyo), Y. Saida (Toho University Ohashi Medical Center, Tokyo), N. Tomita (Hyogo College of Medicine, Hyogo), M. Yoshimitsu (Hiroshima City Asa Hospital, Hiroshima), K. Hase (National Defence Medical College Hospital, Saitama), M. Hamada (Kochi Health Sciences Center, Kochi), M. Ito (National Cancer Center Hospital East, Chiba), K. Maeda (Fujita Health University School of Medicine, Aichi), Y. Kinugasa (Shizuoka Cancer Center Hospital, Shizuoka), M. Ota (Yokohama City University Medical Center, Kanagawa), M. Shiozawa (Kanagawa Cancer Center, Kanagawa), H. Horie (School of Medicine, Jichi Medical University, Tochigi), H. Yamaue (Wakayama Medical University, School of Medicine, Wakayama), H. Ike (Saiseikai Yokohamashi Nanbu Hospital, Kanagawa), N. Takiguchi (Chiba Cancer Center, Chiba), H. Yamagami (Sapporo-Kosei General Hospital, Hokkaido), S. Nishikawa (Aomori Prefectural Central Hospital, Aomori), Y. Akagi (Kurume University School of Medicine, Fukuoka), M. Ohue (Osaka Medical Center for Cancer and Cardiovascular Disease, Osaka), and M. Watanabe (Kitasato University School of Medicine, Kanagawa).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
This study was approved by the Ethics Committee of JSCCR and by the institutional review board of each participating hospital. Informed consent was obtained from all patients.
Electronic supplementary material
Table S1
(DOCX 40 kb)
Fig. S1
Nomogram for grades B and C anastomotic leakage after low anterior resection for rectal cancer. To estimate the probability of grades B and C anastomotic leakage, mark patient values on each axis, draw a straight line perpendicular to the point axis, and sum the points of all variables. Next, mark the sum on the total point axis and draw a straight line perpendicular to the probability axis. NR, no residual tumor (GIF 58 kb)
Fig. S2
Receiver operating characteristic curve for the prediction model of grades B and C anastomotic leakage. Area under the curve was 0.71 (95% confidence interval 0.67–0.76) (GIF 21 kb)
Fig. S3
Calibration of the nomogram for grades B and C anastomotic leakage. The x-axis shows the predicted probability of grades B and C anastomotic leakage, and the y-axis shows the observed probability of grades B and C anastomotic leakage. (GIF 35 kb)
Rights and permissions
About this article
Cite this article
Hoshino, N., Hida, K., Sakai, Y. et al. Nomogram for predicting anastomotic leakage after low anterior resection for rectal cancer. Int J Colorectal Dis 33, 411–418 (2018). https://doi.org/10.1007/s00384-018-2970-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-2970-5